 Research Article
Research Article
A Comparative Study between the Routine Using of Ultrasound Guidance versus Anatomical Guidance in Femoral Artery Access for Endovascular Treatment of Chronic Lower Limb Ischemia
Mina Ragaa Fekry Abdelmalak1*, Usama Saeed Imam2, Ayman Refaat Abdelhaseeb2, Mohamed Hassan Abd El Mawla2, Mohamed Elhousseiny Aboeliazed Elhetamy3 and Mohamed Nashat Sayed Mohamed4
1Vascular Surgery Registrar, Sheffield Teaching Hospitals, UK
2General and Vascular Surgery Department, Beni-Suef University, Egypt
3Tanta General Hospitals, Egypt
4Beni Suef Health Insurance Hospital, Egypt
Mina Ragaa Fekry Abdelmalak, Vascular Surgery Registrar, Sheffield Teaching Hospitals, UK.
Received Date: March 11, 2020; Published Date: April 13, 2020
Abstract
The goal of this study is comparison between the using of ultrasound guidance versus anatomical guidance in femoral artery access for endovascular treatment of chronic lower limb ischemia, by assessment of first pass success rate, total number of attempts required for access, rate of accidental venipunctures, rate of PFA puncture and time to sheath insertion, and assessment of post procedural puncture site complications defined as bruises local hematoma or and retroperitoneal hematoma formation. The study found that US guidance is superior to anatomical guidance in femoral artery access in endovascular treatment of chronic lower limb ischemia in reducing access time, total number of punctures, and number of incidental venipuncture, the incidence of PFA access, incidence of local bruises and retroperitoneal hematoma.
Keywords: US guidance, Endovascular, Femoral artery access, Anatomical access.
Introduction
Chronic lower-extremity ischemia is considered one of the common causes of morbidity and mortality. The vast majority of patients usually are presented with intermittent claudication; a term refers to pain in the leg muscles after activity, or ischemic rest pain that affects the foot and leads to ulceration as well as severe tissue loss later. In fact, the incidence of chronic lowerextremity ischemia is likely to increase as a result of increasing the percentage of elderly people. In the developed countries, peripheral arterial disease (PAD) is common influencing about 14- 20% of the adult population, with a ratio between symptomatic and asymptomatic patients of 1:3 to 1:4 [1]. The first option for treating infrainguinal PAD is usually endovascular treatment as percutaneous transluminal angioplasty (PTA) with adjunctive stenting that has become increasingly used and accepted approach frequently employed for infrainguinal endovascular treatment [2]. The traditional access procedure includes the use of palpation, anatomic landmarks, fluoroscopic guidance or combinations of these maneuvers in order to reach an arterial access [3]. Access site complications such as hematoma, venipuncture, pseudoaneurysm, and arteriovenous fistula, are the major cause of post procedural morbidity &mortality in individuals undergoing percutaneous vascular interventions (PVI) with longer hospital stays, elevated rates of discharge to rehabilitation/nursing facilities, increased 30-Day mortality, and increased one year mortality [4]. In the last decades, US guidance has been widely used for central venous access. In several randomized trials , real time US guidance has been proved to decrease complications, number of trials, and time to access in central venous cannulation [5]. The traditional access procedure includes the use of palpation, anatomic landmarks, fluoroscopic guidance or combinations of these maneuvers in order to reach an arterial access, despite using fluoroscopic guidance seems to be promising in decreasing the complications of access site, randomized trials have not detect the superiority of this maneuver in comparison with the anatomical landmark guidance [3]. On the contrary, the use of ultrasound guidance (UG) has been proved to improve 1st pass success rate and reduce access site complications after common femoral artery access in comparison with the anatomical landmark guidance with & without fluoroscopy [6].
Patients and Methods
The study is prospective, randomized trial involving 200 patients with chronic lower limbs arterial diseases .The study is conducted in vascular surgery unit of Beni-Suef University Hospital. Patients were submitted to percutaneous transluminal angioplasty through common femoral artery access. The patients were divided into 2 group:
Group (1): 100 patients with femoral artery access through the using of anatomical guidance.
Group (2): 100 patients with femoral artery access through the using of US guidance.
Inclusion Criteria
i. Patients with a diagnosis of chronic occlusive or stenotic lower limb arterial disease and considered for interventional angioplasty.
ii. Both males and females.
Exclusion Criteria
i. Patients with unpalpable femoral pulses.
ii. Patients with recent ST elevation myocardial infarction
iii. Pregnant females
iv. Patients with deranged kidney functions
All Patients were subjected to
Pre-procedural Preparation: 1-History taking, clinical examination, Duplex scanning and CT Angiography.
Steps of the procedure: In group A: After being draped, all patients received manual palpation of anatomic landmarks: the anterior superior iliac spine, pubic symphysis, and the femoral pulse. Puncture were made over the femoral pulse until a jet of arterial blood was noted followed by passing of a 0.035’’ guide wire and 6fr sheath then an angiogram was made in order to confirm the position of the guide wire and the sheath. In group B: the US machine was set up and draped, with transmission gel applied. The US imaging was performed in the axial plane. The modified Seldinger technique was intended to be used in all cases.
Post-interventional surveillance: follow up of the patient to evaluate immediate, early or late complications in femoral artery access site within thirty days of the procedure.
i. 1ry end point: Cannulation of common femoral artery occurred successfully.
ii. 2ry end point: total time needed to establish a proper access, the rate of successful endoluminal arterial access, total punctures number needed for access, rate of accidental femoral vein puncture, rate of accidental PFA access. Post procedural puncture site complications as local bruises, local hematoma, pseudoaneurysm or retroperitoneal hemorrhage.
Statistical Methodology
Femoral angiograms were reviewed for proper CFA placement. Angiograms were analysed for the position of the sheath, CFA bifurcation, and origin and most inferior reflection of the inferior epigastric artery relative to the femoral head Collected data were analysed on an intention-to-treat basis. The unpaired Student’s t test or Wilcoxon rank sum test were used for continuous variables, and the chi-square test was used for proportions. The Fisher’s exact test was used for clinical outcomes. A 2-tailed p value of _0.05 was used for significance.
Results
This is a prospective, randomized, single-blinded trial involving patients with chronic lower limbs arterial ischemia. The study was conducted on 200 patients diagnosed as chronic occlusive or stenotic lower limb arterial diseases and considered for interventional angioplasty.
The studied cases were randomly allocated into two groups according to the method of femoral artery access for endovascular treatment of chronic lower limb ischemia:
Group (1): 100 patients with femoral artery access through the using of an anatomical guidance.
Group (2): 100 patients with femoral artery access through the using of ultrasound guidance. The patients’ age ranged from (49) to (69) with an average age of (59.35 ± 5.7) years old (Table 1 & 2).
Table 1:Lesion Site among Studied Population
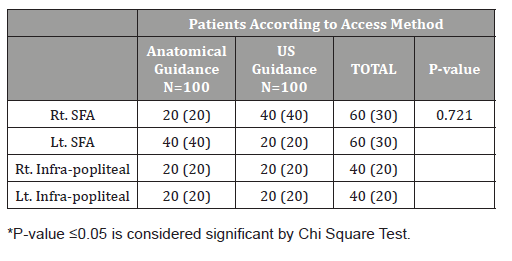
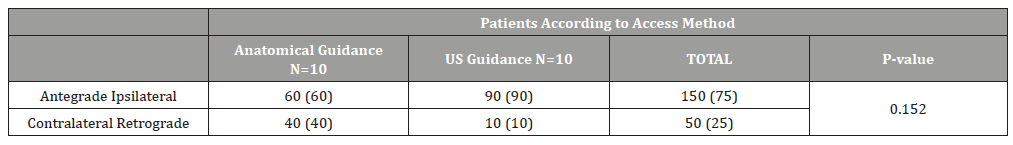
Table 2:Intra-Operative Access to Femoral Artery.
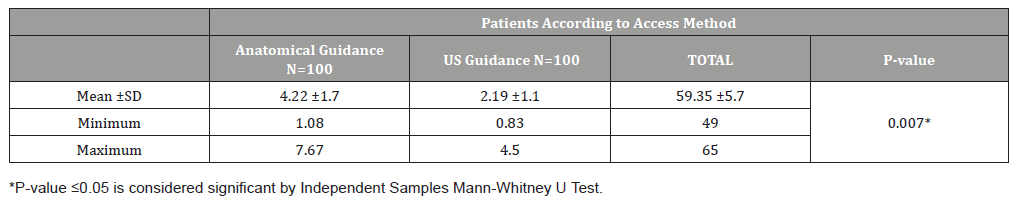
The intraoperative time needed to access the femoral artery was significantly shorter among studied patients who have undergone femoral artery access through uses of ultrasound guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average time in minutes was (2.19 vs. 4.22) in US guidance and anatomical guidance respectively; (p-value= 0.007) (Table 3).
Table 3:Comparison of Time in Minuets to Access the Femoral Artery among the Studied Patients.
Total number of attempts required for access the femoral artery was significantly fewer among studied patients who have undergone femoral artery access through uses of ultrasound guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average number of attempts was (1.60 vs. 2.80) in US guidance and anatomical guidance respectively;(p-value=0.011) (Figure 1) (Table 4).
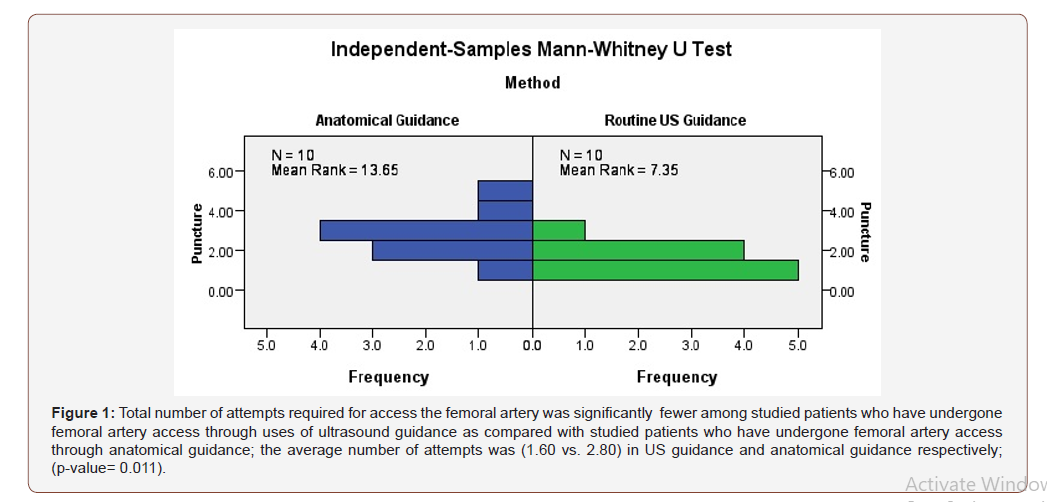
Table 4:Comparison of rate of accidental venipunctures among the studied patients.
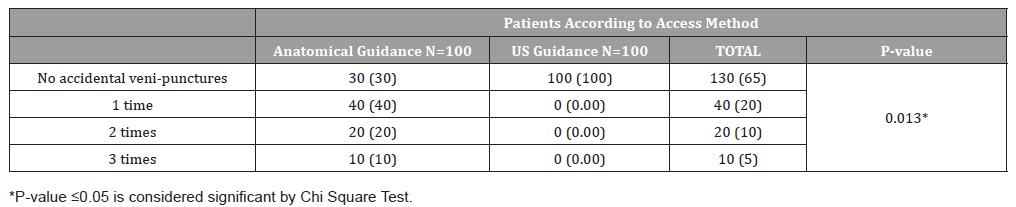
All the studied patients who have undergone femoral artery access through the using of ultrasound guidance had no accidental venipunctures in the present study with a statistically significant difference as compared with the anatomical guidance; (p-value= 0.013).
On the other hand; no accidental venipunctures occurred only in 30 cases (30%) among patients who have undergone femoral artery access through anatomical guidance, 40 cases (40%) had accidental veni-punctures one time, 20 cases (20%) had accidental venipunctures two times, and only ten cases had accidental venipunctures three times (Table 5).
Table 5:PFA Puncture among Studied Cases.
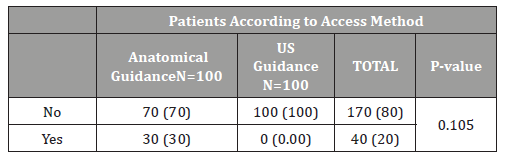
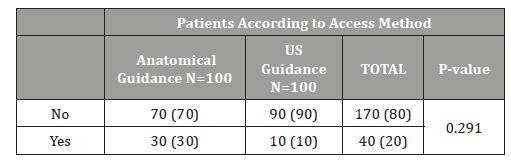
The occurrence of bruises post-operatively was higher among the group of anatomical guided access rather than the US Guidance group; (p-value= 0.291). Thirty cases (30%) in anatomical guidance access method had post-operative bruises in opposite to ten case (10%) among US guidance access method (Table 6).
Table 6:Post-Operative Bruises among Studied Cases.
Discussion
Chronic lower-extremity ischemia is one of the commonest causes of morbidity and mortality, Endovascular treatment is usually the 1st choice for treatment of infrainguinal PAD, Percutaneous transluminal angioplasty (PTA) with adjunctive stenting is a widely used and accepted procedure, and it is the procedure most frequently employed for infrainguinal endovascular treatment [2]. Complications of access site such as hematoma, pseudoaneurysm, venipuncture and AV fistula, are considered a major source of post procedural morbidity and mortality in patients undergoing PVI [4].In this study, we compared the anatomical guidance versus the US guidance in femoral artery access as regard the number of total trial to successfully cannulate CFA defined as mid-way between the origin of inferior epigastric vessels and bifurcation into SFA&PFA, the time needed for the access, the number of venipunctures, the number of PFA punctures and the rate of bruises and hematoma formation in 200 patients divided into 2 groups. The past randomized multicentre studies detected that routine US guidance of femoral arterial access doesn’t achieve improvement of the rate of CFA successful cannulation except in patients with high CFA bifurcations, otherwise it results in time wasting with no significant difference; besides, it needs the availability of US devices and specific training in each centre.
Based on our study findings, US guidance decreased the risk of vascular access complications, improved the 1st pass success rate and approximately eliminated accidental venipunctures, whereas decreasing the time required for access and demonstrated an increased CFA successful cannulation rate in the patients with a CFA bifurcation occur higher than the inferior border of the femoral head. This subgroup of patients can’t be usually detected before catheterization in the absence of previous angiogram data. The intraoperative time required for accessing the femoral artery was significantly shorter among studied patients who have undergone femoral artery access through uses of US guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average time in minutes was (2.19 vs. 4.22) in US guidance and anatomical guidance respectively; (p-value= 0.007). Arnold Seto Arnold H and Morton J Kern [7] in 2016 concluded that US guidance leads to an improved 1st-pass success rate (83% vs. 46%, p ˂ 0.0001). Abu-Fadel MS, et al. [8] in 2009 found that US guidance decreased the number of trials to successfully cannulate CFA (1.3 vs. 3.0, p ˂ 0.0001). In our study the total number of attempts needed for access the femoral artery was significantly fewer among studied patients who have undergone femoral artery access through uses of US guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average number of attempts was (1.60 vs. 2.80) in US guidance and anatomical guidance respectively; (p-value= 0.011). A systematic review of 4 trials with a total of 1422 subjects who underwent femoral artery catheterization revealed 42% improvement in likelihood of 1st-attempt success and 49% decrease in overall access site complications with the use of UG in comparison with traditional palpation approaches.
All the studied patients who have undergone femoral artery access through the using of US guidance had no accidental venipunctures in the present study with a statistically significant difference in comparison with the anatomical guidance; (p-value= 0.013). On the other hand; no accidental venipunctures occurred only in 30 cases (30%) among patients who have undergone femoral artery access through anatomical guidance, 40 cases (40%) had accidental venipunctures one time, 20 cases (20%) had accidental venipunctures two times, and only ten cases had accidental venipunctures three times.
The occurrence of post-operative bruises was higher among the group of anatomical guided access rather than the US Guidance group; (p-value= 0.291). Thirty cases (30%) in anatomical guidance access method had post-operative bruises in opposite to ten cases (10%) among US guidance access method. Inagaki et al., in a study published in Annals of Vascular Surgery in 2018 [9] reported that US guidance was protective against bruises and hematoma formation amongst high-volume of procedures. (P=0.030) The clinical benefit of US guidance is most likely mediated by a decrease in tissue and vessel trauma caused by multiple attempts and venipunctures. Also, US guidance is more likely to achieve a true anterior wall puncture that may permit better arterial wall apposition and more appropriate seating of the introductory sheath. Anatomical guidance in femoral artery access may decrease its caliber, elevating the risk of a posterior or double wall puncture. With US guidance, any compression of the artery is both minimized and made visible during the procedure, potentially reducing the risk of a posterior wall puncture.
Conclusion and Recommendations
Routine US guided femoral artery access was found to be superior to anatomical guided femoral access and improved CFA cannulation by decreasing the number of trials, time to access, risk of venipunctures, PFA puncture and local vascular complications as bruises and hematoma formation in femoral arterial access in endovascular treatment of chronic lower limb ischemia.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Ellis SG, Bhatt D, Kapadia S, Lee D, Yen M, Whitlow P (2006) Correlates and outcomes of retroperitoneal hemorrhage complication percutaneous vascular intervention. Catheter Cardiovasc Interv 67(4): 541-545.
- Adams HP, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. (2007) Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation 115(20): e478-e534.
- Johnston KW (2013) Errors and artifacts of carotid ultrasound evaluation. In: AbuRahma AF, Bandyk DF (eds.), Noninvasive Vascular Diagnosis: A Practical Guide to Therapy 3rd (edn.), Springer, USA, pp. 25-27.
- Ortiz Daniel, Jahangir A, Singh M, Allaqaband S, Bajwa TK, et al. (2014) Access site complications after peripheral vascular interventions: incidence, predictors, and outcomes. Circ Cardiovasc Interv 7(6): 821-828.
- Le Ray Ferrières I, Guinier D (2009) Ultrasound guidance of central venous catheterisation. J Chir 146(6): 528-531.
- Sobolev M, Slovut DP, Lee Chang A, Shiloh AL, Eisen LA (2015) Ultrasound-guided catheterization of the femoral artery: a systematic review and meta-analysis of randomized controlled trials. J Invasive Cardiol 27(7): 318-323.
- Seto AH, Kern MJ (2016) Transulnar catheterization: The road less travelled. Catheter Cardiovasc Interv 87(5): 866-867.
- Abu Fadel MS, Sparling JM, Zacharias SJ, Aston CE, Saucedo JF, et al. (2009) Fluoroscopy vs. traditional guided femoral arterial access and the use of closure devices: a randomized controlled trial. Catheter Cardiovasc Interv 74(4): 533-539.
- Inagaki E, Farber A, Siracuse JJ, Mell MW, Rybin DV, et al. (2018) Routine use of ultrasound guidance in femoral arterial access for peripheral vascular intervention decreases groin hematoma rates in high-volume surgeons. Ann Vasc Surg 51: 1-7.
-
Usama SI, Ayman Refaat A, MH Abd El Mawla, MR Fekry Abdelmalak, ME Aboeliazed Elhetamy, et al., A Comparative Study between the Routine Using of Ultrasound Guidance versus Anatomical Guidance in Femoral Artery Access for Endovascular Treatment of Chronic Lower Limb Ischemia. Anaest & Sur Open Access J. 1(5): 2020. ASOAJ.MS.ID.000521.
-
Ultrasound guidance, Endovascular, Femoral artery access, Anatomical access, Limb, Limb ischemia, Venipuncture, Retroperitoneal hematoma, Pain, Ischemic rest pain, Leg muscles
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






