 Research Article
Research Article
Development of the Family Support Scale (FSS) for Newly Pregnant Women
Mohammad Abbas Uddin1*, Minara Khatun2 and Yongling Hua3
1Research Officer, Directorate General of Nursing and Midwifery, Bangladesh
2Teacher, Sylhet Nursing College, Bangladesh
3Spinal Surgery Department, First Affiliated Hospital of Dali University, Dali, the People’s Republic of China
Mohammad Abbas Uddin, Research Officer, Directorate General of Nursing and Midwifery, Mohakhali, Dhaka-1212, Bangladesh.
Received Date: May 17, 2021; Published Date: June 24, 2021
Maternal mortality and morbidity are challenging issues particularly for developing countries such as Bangladesh. Pregnant women (particularly newly pregnant women) are vulnerable to both maternal mortality and morbidity. Family support, which varies according to social and family situations, may be an important factor in the welfare of pregnant women. An assessment scale for measuring family support for newly pregnant women would be useful for describing their real living situations. The aim of this study was to develop a vigorous family support scale for newly pregnant women in Bangladesh. The study participants were 30 newly pregnant women (aged between 20 to 30 years) who were asked about the support they perceived that they receive from their families. The developed family support scale was found to be a reliable scale for newly pregnant Bangladeshi women, with an internal consistency reliability level of 0.74 (Cronbach’s Alpha Coefficient). The study’s findings are considered transferable to other developing countries. The scale can be used to assess newly pregnant women’s perceived family support in Bangladesh and other developing countries and can support initiatives to improve family support.
Keywords:Newly pregnant women; Family support
Introduction
Maternal mortality ratio is the annual number of female deaths per 100,000 live births from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes). The mortality ratio includes deaths during pregnancy, childbirth, or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, for a specified year [1]. Globally, about 99% of maternal deaths happen in lowand middle-income countries [2]. The Maternal Mortality Ratio in Bangladesh is quite high [3] at 173 deaths/100,000 live births [1], and 13% of deaths of women aged between 15 and 49 occur due to maternal causes, including hemorrhage and abortion-related complications [4]. In addition, about 14 pregnant mothers die every day while giving birth to children in Bangladesh particularly in the rural areas where inadequate health care including safe delivery care facilities [5]. Maternal health is a national priority in Bangladesh. To reduce maternal deaths, the Bangladesh government has initiated programs such as the prevention of early marriage (before 18 years old) [6], implemented World Health Organization (WHO) recommended ideal antenatal visits [7], increased safe delivery facilities, and encourages the use of skilled maternity services. Additionally, in the district and Upazila levels, government deployed skilled midwives to ensure available and skilled delivery care [8]. In Bangladesh, two ongoing problems are particularly relevant to maternal welfare. Firstly, about one-fourth of the total population lives below the poverty level. Secondly, the male-dominated social system creates and perpetuates gender inequality [9]. Also, women are often treated as subordinates by their husbands and are sociallyand economically dependent on them. Under this male domination, many women may not visit a health facility or care provider unless accompanied by a family member, nor can they make spending decisions without the approval of their husband [10]. As a result, many women, particularly pregnant women, are fully- or partially dependent on family support for access to antenatal care.
In rural areas, other factors that may affect pregnant women’s health are low economic and nutritional status, ignorance, physical violence, domestic quarrels with husband and in-laws, stress, poor relationships, and absence of family fanning methods [11-14]. Studies found that lack of attention from the husband will lead to increased pregnancy complications [15-16]. Family Support helps families to access services, including formal supports and informal supports to promote the well-being of families with special needs [17]. Thus, a correct tool for measuring this family support system is useful.
Family support is the support that individuals get from other family fellows. This support varies according to the individual and their needs. Pregnancy is a physiological condition where pregnant women need special care and services. Family support is key to meeting pregnant women’s needs, ensuring they receive appropriate care and can access necessary services. Good family support also contributes positively to reduced maternal mortality and morbidity and infant mortality and morbidity. The following instruments exist for assessing family support: (a) The Family Support Scale [18]. This 13-item scale is suitable for inpatients and epidemiological studies; (b) The Perceived Social Support from Friends and Family [19] consists of 20 items; the participants were undergraduate students and it was developed in an American cultural context; (c) The Chinese Family Support Scale [20] was developed specifically to measure family support in hypertension patients; (d) The Perceived Family Support Scale to Individuals with Special Needs [21] was developed for hearing-impaired individuals; (e) The Thai Family Support Scale for Elderly Parents [22]; and (f) The Family Support Scale (FSS) for Elderly Persons [23]. Nevertheless, no one of these scales is fit for assessing family support for newly pregnant women in Bangladesh due to traditional, societal, and health care services differences. Consequently, there is an earnest need to develop a family support scale (FSS) for Bangladeshi pregnant women.
Data and Methods
Family support is the care that pregnant women get from their husband and other household members. It is similarly significant to assess pregnant women’s insight that their family is capable and ready to deliver such support. Literature about family support [18- 23] has been reviewed and the results applied in the development of the current study’s Family Support Scale for newly pregnant women.
Sample
The sample of this research was 30 newly pregnant women who were using a divisional town’s model family planning clinic in the Sylhet division of Bangladesh in November 2020. The clinic provides antenatal and other family planning care. Before data collection, the investigator obtained oral permission from the model family planning clinic authority. The researcher assigned a research assistant to data collection. The research assistant was informed of the research’s purposes and data collection methods. Newly pregnant women who visited the model family planning clinic for services were considered as participants. After they had accessed the services, they were asked to participate in an interview for data collection. Informed written consent was obtained from those patients who agreed to participate in the interview. The research assistant read the Bengali-language questionnaire to the newly pregnant women and marked their responses on the questionnaire sheet.
Validity of the Family Support Scale for Newly Pregnant Women
‘Content validity’ denotes to the precision of a measurement tool. The researcher requested three (03) specialists to evaluate the English version instrument to check its content validity and cultural suitability. The specialists were from the National Institute of Advanced Nursing Education and Research [NIANER], College of Nursing, Sher-E Bangla Nagar, Dhaka and Fozderhat Nursing College, Chittagong, Bangladesh. The final version of the scale was reviewed based on the specialists’ remarks. The final English version of the Family Support Scale for newly pregnant women was converted using the back–conversion method [24]. The original English scale was converted into Bengali by an interpreter. The Bengali scale was then converted back to English by another convertor. Subsequently, a third convertor linked the two English forms and recognized any contradictions. These were then corrected.
Instruments
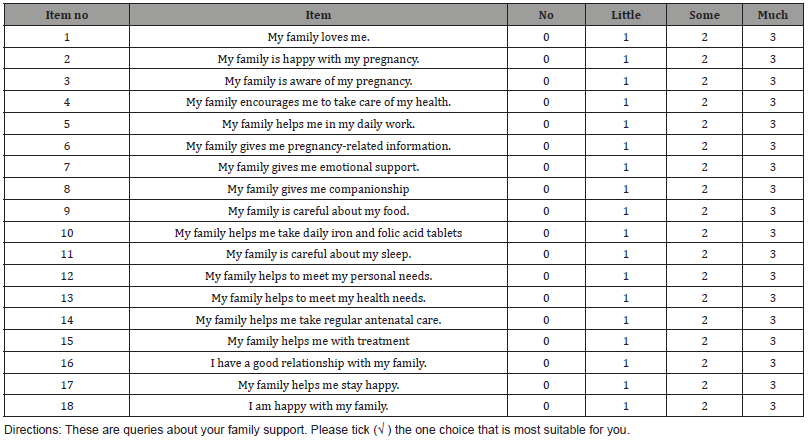
This study used a self–directed questionnaire, developed by the researcher, originated on current literature about family support. The instrument had two parts. Part 1: the Demographic information with seven items: age, occupation, religion, highest educational level, number of family members, family’s monthly income, and husband’s occupation. Part 2: the Family Support Scale for newly pregnant women, in which the newly pregnant women evaluated their perception of their family’s support for them using 18 criteria: love, family’s happiness with, and awareness of, the pregnancy (2 items), health, help, information, emotions, companionship, food, taking of iron and folic acid, sleep, personal needs, health needs, antenatal care, treatment, relationship with family, family’s contribution to the participant’s happiness, and personal happiness. Each item was assessed via a 4-point, Likertstyle scale, with potential scores ranging from 0 (none) to 3 (much). Total potential scores were between 0 and 54. Greater scores indicate greater perceived family support for the newly pregnant women.
Results
Demographic information
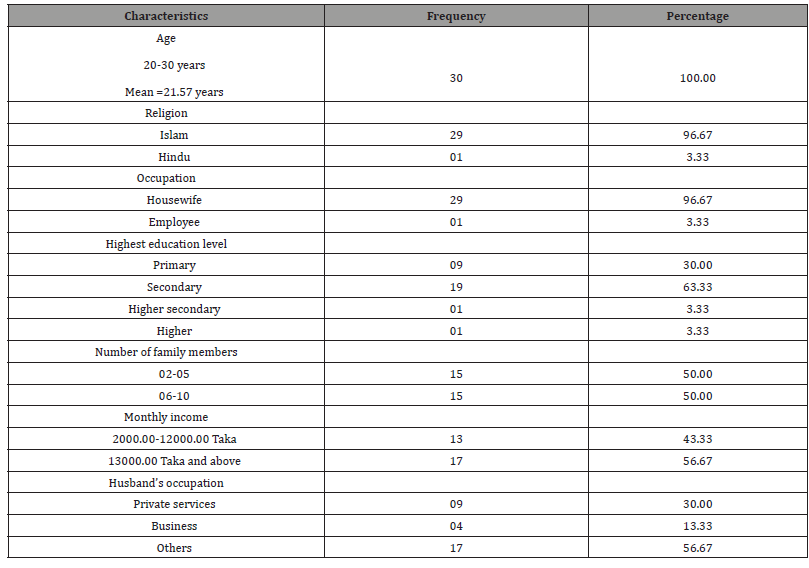
The participants were 30 newly pregnant women between 20 and 30 years old, with a mean age of 21.57 years. Twenty-nine were Muslim and one was Hindu. Twenty-nine were housewives and one was employed. Nine had completed only primary level education, nineteen has also completed secondary level education, one had also completed higher secondary level education, and one had also completed higher level education. Their family sizes were between 2 and 10 people. Family’s monthly incomes were between 2000.00 and 25000.00 Taka. Participants’ husbands were engaged in private services, business, and other professions (Table 1).
Table 1:Demographic features of the sample (n=30).
Reliability of the Family Support Scale for Newly Pregnant Women
The Family Support Scale for newly pregnant women was confirmed for internal consistency reliability. The SPSS program was used to examine the data. All 18 items were entered into the package and analyzed. The result was a Cronbach’s Alpha Coefficient of 0. 74 (Table 2 & 3).
This goal of this study was to develop a usable and consistent tool for assessing family support for newly pregnant women. The Family Support tool was developed based on the results of the literature review. Twenty- five areas of support were recognized during the literature review. More than half had contained in earlier studies’ tools for assessing family support: love, activities, personal needs [16], information, and company [18], emotional support, health needs, personal needs, treatment, food, and sleep [23]. The present study’s researcher also included one common item of “taking good care” which enclosed a variety of support areas, including the family’s awareness of the pregnancy, their encouragement with maintaining health, the taking of daily iron and folic acid tablets, antenatal care, and the relationship between the participant and their family. Item analysis was performed. Seven items were deleted to raise the standard level (Cronbach’s Alpha Coefficient equal to or more than. .70). The 18 items were selected, and their mean and Standard Deviation given (Table 4).
Table 2:Reliability of the family support scale (Reliability Statistics).
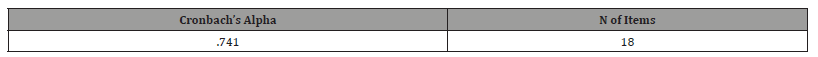
Table 3:Item analysis statistics of family support scale.
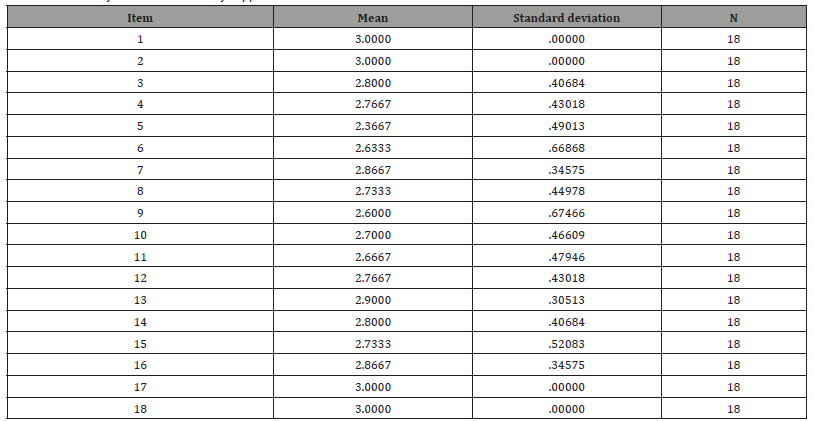
Table 4:Eighteen (18) items of family support for the newly pregnant women.
Discussion
This study aimed to develop a scale to measure the newly pregnant women’s perceived family support from the family. The participants were 30 newly pregnant women. They were selected from a family planning clinic located in Sylhet division in Bangladesh. A self-administered scale consisting of 25 questions was used to collect the data. The data were analysed and internal consistency reliability (Cronbach’s Alpha Coefficient) was found to be less than .70, below the standard level. To increase the internal consistency reliability level, seven (07) items were gradually deleted. Internal consistency reliability (Cronbach’s Alpha Coefficient) was then verified again and was found to be .74, the standard level. Finally, the 18 items were selected to develop the family support scale (FSS) for newly pregnant women. The limitations of this study were: a) data were collected from a single setting; b) most participants were housewives; c) most participants’ highest education levels were primary or secondary.
Conclusion
The final form of the 18-item FFS is a self-reporting questionnaire which assesses newly pregnant women’s perceived family support. An acceptable and standard number of samples were used to collect data. The psychometric properties of the scale were established through back conversion, assessment of cultural suitability, assessment of content validity, and validation of reliability using the SPSS package. The FSS’s reliability was above the suitable level [25].
Recommendations
Further study may be conducted to collect data from different hospital settings, including rural and urban, and from various groups, including the employed and unemployed, the moreeducated and less-educated, and those with small and large families.
Ethical Considerations
Approval was obtained from the study setting’s authority and participants.
Acknowledgments
The researchers express appreciation to the newly Bangladeshi pregnant females for their co- operation.
Conflicts of Interest
No conflict of interest has been stated by the researchers.
References
- Singla S, Singla R (2016) Stroke in India: Bio-socioeconomic determinants. J Soc Health Diabetes 04(02): 071-6.
- Kamalakannan S, Gudlavalleti ASV, Gudlavalleti VSM, Goenka S, Kuper H (2017) Incidence & prevalence of stroke in India: A systematic review. Indian J Med Res 146(2): 175-185.
- Pandian JD, Sudhan P (2013) Stroke Epidemiology and Stroke Care Services in India. J Stroke. 15(3): 128-134.
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, et al. (2013) An Updated Definition of Stroke for the 21st Century: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 44(7): 2064-2089.
- NINDS Post-Stroke Rehabilitation [Internet]. Available from: https://www.stroke.nih.gov/materials/rehabilitation.htm
- Sunderland A (2000) Recovery of ipsilateral dexterity after stroke. Stroke 31(2): 430-433.
- Boukadida A, Piotte F, Dehail P, Nadeau S (2015) Determinants of sit-to-stand tasks in individuals with hemiparesis post stroke: A review. Ann Phys Rehabil Med 58(3): 167-172.
- Warlow CP, Dennis MS, Van Gijn J, Hankey G, Barnett HJM, et al. (2001) Stroke- A practical guide to management. 2nd ed. United Kingdom: Blackwell.
- Fahey M, Crayton E, Wolfe C, Douiri A (2018) Clinical prediction models for mortality and functional outcome following ischemic stroke: A systematic review and meta-analysis. PLOS ONE 13(1): e0185402.
- Tempest S, McIntyre A (2006) Using the ICF to clarify team roles and demonstrate clinical reasoning in stroke rehabilitation. Disabil Rehabil 28(10): 663-667.
- Silva SM, Corrêa FI, Faria CD, Buchalla CM, Silva PF, et al. (2015) Evaluation of poststroke functionality based on the International Classification of Functioning, Disability, and Health: a proposal for use of assessment tools. J Phys Ther Sci 27(6): 1665- 1670.
- ICF Definition- WHO. https://www.who.int/classifications/icf/icfbeginnersguide.pdf?ua=1
- Sykes C (2006) Health Classifications 1 - An introduction to the ICF. WCPT Keynotes. World Confederation for Physical Therapy.
- Brasure M, Lamberty GJ, Sayer NA, Nelson N, Macdonald R, et al. (2012) Multidisciplinary Post-acute Rehabilitation for Moderate to Severe Traumatic Brain Injury in Adults [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); (Comparative Effectiveness Reviews, No. 72.).
- Hislop H, Montgomery J (2007) Daniels and Worthingham’s Muscle Testing: Techniques of Manual Examination, 8th ed. W.B. Saunders St. Louis.
- Lunar FRM, Gorgon EJR, Lazaro RT (2017) Clinimetrics of the Upright Motor Control Test in chronic stroke. Brain Behav 7: e00826.
- Janssen WG (2008) The sit-to-stand movement recovery after stroke and objective assessment, Ph.D. dissertation Erasmus Medical Center Erasmus University Rotterdam The Netherlands.
- Janssen WG, Bussmann HB, Stam HJ (2002) Determinants of the sit-to-stand movement: a review. Physical Therapy 82(9): 866-879.
- Oh D (2013) Community Ambulation: Clinical Criteria for Therapists’ Reasoning and Decision-making in Stroke Rehabilitation. International Jrnl of Physical Med and Rehab 1(4): 2329-9096.
- Adegoke BO, Olaniyi O, Akosile CO (2012) Weight bearing asymmetry and functional ambulation performance in stroke survivors. Glob J Health Sci 4(2): 87-94.
- Perry J, Garrett M, Gronley JK, Mulroy SJ (1995) Classification of walking handicap in the stroke population. Stroke 26(6): 982-989.
- Shumway-Cook A, Wollacott MH (1995) Motor Control: Theory and Practical Applications. Baltimore, Md: Williams and Wilkins Inc.
- MMSE guidelines. https://www.ncbi.nlm.nih.gov/projects/gap/cgibin/ GetPdf.cgi?id=phd001525.
- Mao YR, Wu XQ, Zhao JL, Le L, Xiu QW, et al. (2018) The Crucial Changes of Sit to Stand Phases in Subacute Stroke Survivors Identified by Movement Decomposition Analysis. Front Neurol 9: 185.
- Wagatsuma M, Kim T, Sitagata P, Lee E, Vrongistinos K, et al. (2019) The biomechanical investigation of the relationship between balance and muscular strength in people with chronic stroke: a pilot cross-sectional study. Top Stroke Rehabil 26(3): 173-179.
- Berger RA, Riley PO, Mann RW, Hodge WA (2019) Total body dynamics in ascending stairs and rising from a chair following total knee arthroplasty. Trans Orthop Res Soc 13: 542.
- de Haart M, Geurts AC, Dault MC, Nienhuis B, Duysens J (2005) Restoration of weight shifting capacity in patients with postacute stroke: a rehabilitation cohort study. Arch Phys Med Rehabil 86(4): 755-762.
- Dettmann MA, Linder MT, Sepic SB (1987) Relationships among walking performance, postural stability, and functional assessments of the hemiplegic patient. Am J Phys Med 66: 77-90.
- Lomaglio M, Eng J (2005) Muscle strength and weight-bearing symmetry relate to sit-to-stand performance in individuals with stroke. Gait and Posture 22(2): 126-131.
- Bohannon RW (2007) Muscle strength and muscle training after stroke. J Rehabil Med 39(1):14-20.
- Xu J, Ejaz N, Hertler B, Widmer M, Kitago T, et al. (2017) Separable systems for recovery of finger strength and control after stroke. J Neurophysiol 118(2): 1151- 1163.
- Geyh S, Cieza A, Schouten J, Dickson H, Frommelt P, et al. (2004) ICF Core Sets for stroke. J Rehabil Med 44: 135-141.
- Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A (2002) Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci 57(8): M539-M543.
- Pinheiro M, Polese JC, Machado G, Scianni AA, Hirochi TC, et al. (2010) Balance analysis during the sit-to-stand movement of chronic hemiparetic individuals based upon their functional levels. Man Ther Posturology Rehabil J 12: 260-264
- Akulwar IS (2019) Can Quantitative Balance Measures Discriminate between Functional Ambulation Categories in Chronic Stroke Survivors? Physiother Rehabil 4: 178.
- Ju S (2020) Correlation between lower limb muscle asymmetry during the sit-to-stand task and spatiotemporal gait asymmetry in subjects with stroke. J Exerc Rehabil 16(1): 64-68.
- Lee G, An S, Lee Y, Park DS (2016) Clinical measures as valid predictors and discriminators of the level of community ambulation of hemiparetic stroke survivors. J Phys Ther Sci 28(8): 2184-2189.
- Danielsson A, Meirelles C, Willen C, Sunnerhagen KS (2014) Physical activity in community-dwelling stroke survivors and a healthy population is not explained by motor function only. PM R 6(2): 139-145.
- Akbari A, Karimi H (2006) The Relationship Between Lower-extremity Muscle Strength and Functional Performance in Hemiparetic Patients. Journal of Medical Sciences 6: 327-331.
- Moriello C, Finch L, Mayo NE (2011) Relationship between muscle strength and functional walking capacity among people with stroke. J Rehabil Res Dev 48(3): 267-275.
- Nadeau S, Arsenault AB, Gravel D, Bourbonnais D (1999) Analysis of the clinical factors determining natural and maximal gait speeds in adults with a stroke. Am J Phys Med Rehabil 78(2): 123-130.
- Eng JJ, Tang PF (2007) Gait training strategies to optimize walking ability in people with stroke: a synthesis of the evidence. Expert Rev Neurother 7(10): 1417-1436.
-
Mohammad Abbas Uddin, Minara Khatun, Yongling Hua. Development of the Family Support Scale (FSS) for Newly Pregnant Women. Arch Neurol & Neurosci. 10(4): 2021. ANN.MS.ID.000743.
-
Newly pregnant women, Family support, Maternal health, emotional support, health needs, personal needs, treatment, food, sleep.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






