 Mini Review
Mini Review
Combined Intracorneal Ring Segments and Corneal- Collagen Crosslinking
Larissa Gouvea1, Karolinne Maia Rocha1*, Drew Dickson1, and George O Waring IV2
1Department of Ophthalmology, Storm Eye Institute, Medical University of South Carolina
2Waring Vision Institute, USA
Karolinne Maia Rocha, Department of Ophthalmology, Storm Eye Institute, Medical University of South Carolina, USA.
Received Date: December 07, 2018; Published Date: January 03, 2019
Abstract
Keratoconus (KCN) is a bilateral, progressive, non-inflammatory corneal disease of which etiology is not completely understood. If left untreated, it may lead to significant visual impairment due to irregular astigmatism. Corneal crosslinking (CXL) is currently the only treatment option that halts the progression of the disease and may help avoid corneal transplantation. Although it may not improve visual acuity (VA), CXL can be combined with refractive procedures such as intracorneal ring segment (ICRS) implantation to achieve a better postoperative outcome. The sequence of treatment is a cause of discussion. Some believe sequence is not important with halted progression and improvement in refractive outcome achieved regardless, while different studies have shown the superiority of ICRS implantation followed by either concurrent of sequential CXL.
Keywords:Corneal crosslinking; Intracorneal rings; Keratoconus
Abbreviations: CXL: Corneal Cross-Linking; DCVA: Distance Corrected Visual Acuity; ICRS: Intracorneal Ring Segment; I-S: Inferior-Superior; KCN: Keratoconus; Kmax: Maximal Keratometry; MRSE: Mean Refraction Spherical Equivalent; OD: Right Eye; UVA: Ultraviolet A; VA: Visual Acuity
Introduction
Keratoconus is an asymmetric, progressive disease in which the cornea assumes a conical shape and usually presents with progressive non-inflammatory stromal thinning and irregular astigmatism, which in turn reduces quality of vision [1,2].
The only available treatment to halt the progression of KCN is CXL [3]. Furthermore, it is a procedure that could avoid the necessity of corneal transplantation such as lamellar or penetrating keratoplasty [4]. To halt progression, CXL uses ultraviolet A (UVA) and vitamin B2 (Riboflavin) to strengthen the corneal stroma collagen bonds and make it less flexible and elastic [3,5]. ICRS on the other hand, improve visual acuity in patients intolerant to contact lenses by inducing flattening of the cornea, which improves corneal astigmatism and myopia [3-6].
Several studies have been published on the effects and safety of CXL PLUS (CXL combined with a refractive procedure, usually ICRS) [4-8] on refractive outcomes, VA, and corneal topography. It is hypothesized that CXL induces an additional flattening in corneas with ICRS, which in turn produces a superior effect in visual outcome [9]. The purpose of this article is to quickly review the aspects of combined corneal crosslinking and intracorneal ring segments implantation to stop progression of keratoconus.
Discussion
CXL PLUS has been found to be a relatively safe and effective procedure when compared to either standalone technique [3,4,7,9]. Nevertheless, concerns on treatment sequence have been reported. Coskunseven et al [8] have reported that ICRS before CXL provides a better outcome than CXL before ICRS and hypothesized that CXL as the first procedure may produce a stiffening of the cornea that prevents full effectiveness of ICRS. Alternatively, a halt in KCN progression has also been reported when performing the CXL procedure before ICRS implantation [10]. In studies where no difference was found in CXL alone versus combined ICRS-CXL, it has been said that the CXL effect on collagen and corneal biomechanics actually reduces the effect on ICRS [4].
Concurrent procedures may result in a greater corneal improvement due to an accumulation of riboflavin on the recently created corneal tunnels. This enhances the effects of CXL flattening on the cornea, thereby resulting in lower postoperative keratometry readings, with improvements reaching as high as 5D and greater refractive outcome [3,7,11]. Nevertheless, complications such as central corneal haze and paradoxical central corneal steepening have been reported in concurrent procedures [9]. To prevent such complications, it has been recommended to suture the ring channels to prevent uneven distribution of riboflavin that could cause a contraction in the cornea and paradoxically increase central steepening [9].
The thickness and quantity of Ring segments are determined accordingly on the nomogram based on the patient’s preoperative manifest refraction spherical equivalent (MRSE), type, and location of KCN. Symmetric ICRS are used in central KCN with MRSE greater than cylindrical power, whereas asymmetric or single ICRS are used in decentered or inferior cones, with less MRSE than cylinder [12]. By contrast, 1 ring segment has been found to be more effective in KCN due to a greater differential corneal flattening, which is believed to improve the conic shape of the cornea and reduce irregular astigmatism. Furthermore, a single segment can also lessen the amount of induced glare [6].
To exemplify, we report a case of a 27-year-old male with asymmetric KCN and contact lens intolerance in the right eye (OD) in which we did concurrent ICRS-CXL treatment. One ICRS was placed inferiorly due to the asymmetric inferior steepening and high cylinder [6,12]. In accordance to previous recommendations, a 10-0 nylon suture was placed at the incision site after ICRS implantation and before corneal de-epithelization and CXL [9]. Postoperatively, we observed a 4D flattening of the corneal and improved DCVA from 20/60 to 20/30.
Case Report
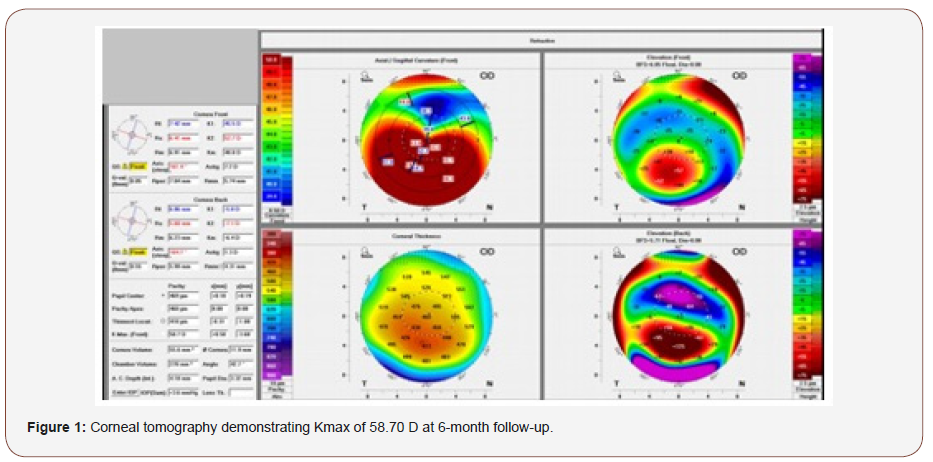
A 27-year-old male presented complaining of worsening vision in his right eye (OD). His examination revealed a manifest refraction of -3.50 -6.00 @ 70° and a distance corrected visual acuity (DCVA) of 20/60. Initial corneal tomography showed an irregular astigmatism with inferior steepening, superior flattening, an increase in the inferior-superior (I-S) ratio, and irregular astigmatism. Maximal keratometry (Kmax) at this time was 54.40 D, which increased to 58.70 D 6 months later (Figure 1). The patient had attempted to use contact lenses in the past but did not tolerate them.
The patient agreed to undergo combined ICRS-CXL. A F200 Femtosecond Laser (Alcon, USA) was used to create a tunnel, and a 0.45-mm segment was placed inferiorly. One single segment was placed inferiorly to correspond to the keratoconic apex in order to lift it and produce the maximal flattening effect. The incision was secured, and an epithelium-off CXL with the KXLTM System (Avedro, USA) was performed. One drop of moxifloxacin hydrochloride ophthalmic solution 0.5% (Vigamox; Alcon) was placed and the end of the case, followed by placement of a bandage contact lens. The patient was instructed to use moxifloxacin and prednisolone acetate 1% four times daily and to use preservative-free artificial tears frequently. He was seen the next day, and the bandage contact lens was removed at post-op day [7].
At the patient’s 3-month follow-up appointments, the Kmax was 54.50 D (Figure 2), improved from 58.70 prior to his combined ICRS and CXL. The manifest refraction was -2.50 -4.00 @ 65°, and the DCVA was 20/30 +1 in the right eye. The corneal tomography at this time showed a more regular astigmatism that was more amenable to correction with glasses and contact lenses. Epithelial remodeling with a more regular thickness profile was seen on spectral-domain OCT.

Conclusion
Combined procedures have been shown to have a greater effect in the treatment and improvement of visual acuity and quality of vision in patients with KCN. Concurrent or sequential procedures as safe as standalone treatments and are a great alternative to patients intolerant to contact lenses.
Acknowledgement
None.
Conflict of interest
No conflicts of interest.
References
- Rabinowitz YS (1998) Major review. Surv Ophthalmol 42(4): 297-319.
- Tur VM, Macgregor C, Jayaswal R, Ed F, Brart DO, et al. (2017) ScienceDirect A review of keratoconus: Diagnosis, pathophysiology, and genetics. Surv Ophthalmol 62(2): 770-783.
- Hashemi H, Alvani A, Seyedian MA, Yaseri M, Khabazkhoob M, et al. (2018) Appropriate Sequence of Combined Intracorneal Ring Implantation and Corneal Collagen Cross-Linking in Keratoconus. Cornea 37(12): 1601- 1607.
- Legare ME, Iovieno A, Yeung SN, Lichtinger A, Kim P, et al. (2013) Intacs with or without same-day corneal collagen cross-linking to treat corneal ectasia. Can J Ophthalmol 48(3): 173-178.
- Ibrahim O, Elmassry A, Said A, Abdalla M, El Hennawi H, et al. (2016) Combined femtosecond laser-assisted intracorneal ring segment implantation and corneal collagen cross-linking for correction of keratoconus. Clin Ophthalmol 10: 521-526.
- Yeung SN, Ku JYF, Lichtinger A, Low SAW, Kim P, et al. (2013) Efficacy of single or paired intrastromal corneal ring segment implantation combined with collagen crosslinking in keratoconus. J Cataract Refract Surg 39(8): 1146-1151.
- Saleem MIH, Ibrahim Elzembely HA, AboZaid MA, Mohammed Elagouz, Ahmed Mohamed Saeed, et al. (2018) Three-Year Outcomes of Cross-Linking PLUS (Combined Cross-Linking with Femtosecond Laser Intracorneal Ring Segments Implantation) for Management of Keratoconus. J Ophthalmol: (1-8).
- Coskunseven E, Jankov MR, Hafezi F, Atun S, Arslan E, Kymionis GD, et al. (2009) Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg 35(12): 2084-2091.
- Avni-Zauberman N, Rootman DS, Hafezi F, Atun S, Arslan E, et al. (2014) Cross-linking and intracorneal ring segments - Review of the literature. Eye Contact Lens 40(6): 365-370.
- Henriquez MA, Izquierdo L, Bernilla C, McCarthy M (2012) Corneal collagen cross-linking before ferrara intrastromal corneal ring implantation for the treatment of progressive keratoconus. Cornea 31(7): 740-745.
- El-Raggal TM (2011) Sequential versus concurrent KERARINGS insertion and corneal collagen cross-linking for keratoconus. Br J Ophthalmol 95(1): 37-41.
- Rocha KM (2018) A two-pronged approach to keratoconus. Cataract Refract Surg Today.
-
Larissa Gouvea, Karolinne Maia Rocha, Drew Dickson, George O Waring IV. Combined Intracorneal Ring Segments and Corneal- Collagen Crosslinking. W J Opthalmol & Vision Res. 1(2): 2019. WJOVR.MS.ID.000510.
-
Corneal crosslinking, Intracorneal rings, Keratoconus, Stromal thinning Irregular astigmatism, Corneal topography, Visual acuity, Maximal keratometry, Intracorneal ring segment, Inferior-superior, Right eye, Ultraviolet A, Visual acuity.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






