 Case Report
Case Report
Pregnancy, Submucous uterine myoma, Cesarean section, Myomectomy
Sinchikhin Sergei Petrovich*, Stepanyan Lusine Vardanovna
Astrakhan State Medical University, Russia
Sinchikhin Sergey Petrovich, Professor, Head of the Department of Obstetrics and Gynecology, Faculty of Medicine, Astrakhan State Medical University, 414000. Astrakhan, Russia.
Received Date: July 24, 2020; Published Date: August 04, 2020
Abstract
This article presents the results of our study on the prevalence of uterine fibroids in women of different age groups, as well as infertility, miscarriage and other diseases of the internal genital organs.
We gave an example of an unusual case of a combination of a uterine pregnancy and a large submucous myomatous node.
It has been proved that the use of new original technologies helps to reduce blood loss while performing a cesarean section and myomectomy.
Keywords: Pregnancy; Submucous uterine myoma; Cesarean section; Myomectomy
Case Report
The most common tumors of the internal genital organs in women include uterine fibroids. In the structure of gynecological pathology, it ranks second after inflammatory diseases. This disease is observed, in general, in European countries in 24 million women, and in North American countries in 20 million patients [1-3].
The results of our own research show that uterine fibroids during prophylactic examinations are detected in 18-20% of women, during pregnancy in 8-10% of patients, among patients in gynecological hospitals in 25-30% of them, and among all those operated on, morphological signs of a benign uterine tumor are diagnosed in biopsy material in 85% of cases [3].
According to our data, uterine fibroids are more often (up to 65%) detected at the age of 40-50 years, when the clinical manifestations of the disease force a woman to seek medical help. However, at the age of 21 to 36 years, uterine fibroids are most often combined with infertility (up to 21%), miscarriage (up to 27%), ovarian dysfunction (up to 29%) [3].
In recent years, there has been a “rejuvenation” of the disease, which some re-searchers associate with an increase in the frequency of inflammatory diseases of the genital organs and early onset of sexual relations [1]. According to our data, among all women in whom fibromatous nodes are detected using ultrasound, patients under the age of 21 are found in 4% of cases.
In the reproductive age, according to the pathogenetic development, the growth of myomatous nodes is noted [2]. At the same time, without drug therapy, the most in-tense annual increase is observed with the intermuscular arrangement of the nodes, because at this localization, a benign tumor of the uterus is in optimal conditions for blood supply. Slower growth was noted with subserous location of the myomatous node. However, any, even small size of the node with a given localization can create an urgent situation associated with the torsion of its “long leg”. The submucous myomatous nodes increase in size most slowly, given the smallest blood supply. However, in the presence of this localization, there are clinical manifestations that are the reason for a woman to seek medical help: intermenstrual bleeding from the genital tract, infertility, miscarriage, etc.
Currently, we are of the opinion that if a patient has a myomatous node with a diameter of more than 40 mm or if it is submucous, it is necessary to carry out special treatment in the pregravid period on an individual basis, aimed at reducing its size or removing it (drug therapy, myomectomy, etc.) [3]. This is due to the fact that in the gestational period, with the continued accelerated growth of uterine fibroids, the risk of developing myometrial ischemia in the area of the node location increases many times, and with the location of the node deforming the contours of the uterine cavity, there is a high risk of miscarriage. At the same time, we note that there are also unusual clinical cases that are of professional interest. We would like to acquaint with one of such clinical cases.
Patient B, 29 years old, was admitted to the gynecological department with clinical signs of a threat of miscarriage at 7-8 weeks of gestation. From the anamnesis it was known that the real pregnancy was the first, desired. The patient got registered for pregnancy in the antenatal clinic at 6-7 weeks, after an ultrasound examination, in which not only a uterine pregnancy was diagnosed, but also the presence of a large submucous myomatous node. After that, the patient was recommended to terminate the pregnancy and undergo myomectomy, which she categorically refused. The patient indicated that she did not seek medical help for extragenital pathology and gynecological diseases.
On the day of admission to the hospital, a sonographic study was performed, during which the presence of an ovum with gestational sizes of 7-8 weeks was diagnosed, as well as the presence of retro chorial hematoma and a myoma node submucous located on the posterior wall of the uterus (measuring 77x64mm). Conservative hemostatic therapy and, in general, preserving therapy was effective, the patient with progressive pregnancy was discharged from the gynecological department after 10 days of inpatient treatment.
It should be noted that in the subsequent clinical signs of termination of pregnancy with the presence of retro chorial hematoma repeated at 11-12 weeks of gestation. At the same time, the therapy aimed at prolonging pregnancy was also effective.
We are supporters of prophylactic metabolic therapy during the gestational period in patients at risk of developing placental dysfunction, because we believe that this therapy can improve the function of the feto-placental complex and prevent, in some cases, the progression of placental insufficiency [4,5]. It should be noted that despite the ongoing preventive therapy to improve the function of the planet, intrauterine growth retardation against the background of uterine fibroids was observed in this clinical case, however, the fetal condition throughout the gestational period was satisfactory and did not cause any concerns.
At 35 weeks of gestation, the pregnant patient had mild iron deficiency anemia, for which antianemic therapy was carried out.
At 38 weeks in the obstetric hospital, an ultrasound examination was performed, during which it was found that the total dimensions of the submucous node were 88x64 mm, and its echo graphic structure indicated edema of its tissue. The fetal head was below the node location. Taking into account the appearance of scanty bloody dis-charge from the uterus and sonography data, as well as taking into account the unusual clinical situation, it was decided to perform abdominal delivery and perform surgical organ-preserving treatment of uterine fibroids. At the same time, in order to reduce intraoperative blood loss, it was decided to use the methods previously developed by us, for which patents of the Russian Federation for inventions were obtained [6,7].
In particular, to prevent the development of coagulopathic bleeding during the incision of the anterior abdominal wall during the cesarean section, 10 ml of 10% calcium gluconate solution and 10 ml of tranexamic acid were sequentially injected into the patient’s peripheral vein intravenously (RF patent No. 2629040 for the invention “Method of prevention coagulopathic bleeding during caesarean section) [6].
The proposed dosage of the above drugs is the most optimal for achieving rapid drug hemostasis in the perioperative period, and also safe not only for the operated patient, but also for the newborn, since the maximum concentration of drugs in the mother’s body occurs after the fetus is removed from the uterus.
The mechanism of action of calcium gluconate is increased coagulation and rapid thrombosis of the vascular wall defect. This is due to the fact that calcium ions belong to the IV plasma factor of the blood coagulation system and play a role in the sequential activation of other plasma coagulation factors (II, III, Va, Xa, XIa, XIIa, XIIIa). In addition, calcium takes part in the contraction of the smooth muscles of the body of the uterus, which has a positive effect on the prevention of uterine hypotension.
The pharmacokinetics of another drug that is used in this method of the invention is that tranexamic acid prevents the transition of profibrinolysin (plasminogen) to fibrinolysin (plasmin), i.e. tranexamic acid inhibits the fibrinolytic activity of the hemostatic system and slows down the resorption of the formed thrombus in the damaged vessel. The use of tranexamic acid does not increase the systemic blood coagulation potential in pregnant women. Therefore, the likelihood of developing thrombosis in this category of pregnant women is not higher than in patients who did not take this drug. The use of the tranexamic acid preparation helps to reduce tissue bleeding during and after surgery, reduce the volume of blood loss, and, consequently, the need for transfusion of donor erythrocytes. An additional important pharmacological property of tranexamic acid is its anti-inflammatory effect, which is due to the suppression of the formation of kinins, pro-inflammatory cytokines (tumor necrosis factor, interleukin-1, interleukin-2) and other active peptides involved in inflammatory and allergic reactions [6].
To carry out devascularization of the uterus during a cesarean section in this clinical case, we used our original method of temporary mechanical ischemia of the uterus, according to the developed invention (RF patent No. 2638459 “Method for reducing blood loss during cesarean section”) [7].
It should be noted that the proposed invention uses a loop made of plastic (Figure 1), which has the necessary plasticity and strength, has a convenient lock for its reliable fixation, and after use is easily cut off with scissors. This plastic hinge with a lock is included in the register of medical devices and has a low cost.
The main stages of the implementation of this method are carried out as follows. During a cesarean section after a surgical incision in the uterus, the removal of the fetus and afterbirth from the uterine cavity, a plastic tightening loop with a lock is brought in to the isthmus of the uterus with the capture of its ligaments and the vessels passing through them, which is applied below the incision on the uterus, tightly tightened and fixed in castle. Then the operating wound on the uterus is sutured, after which the plastic loop is cut with scissors and removed from the abdominal cavity [7].
Distinctive features of the proposed method are ease of implementation, which does not require high qualifications of the doctor, the ability to quickly perform manipulations and the absence of systemic effects on the body. In addition, compression with a plastic loop in the area of the isthmus of the uterus of the main blood vessels supplying it contributes to temporary ischemia of both the upper and lower segments of the uterus.
An additional advantage of the developed method is that it can be used not only for prophylactic reduction of blood loss during a cesarean section, but also for stop-ping the developed uterine bleeding. It should be emphasized once again that the com-pression of tissues in the area of the isthmus of the uterus and compression of the uterine vessels does not have a negative effect on the contractility of the myometrium. The practical significance of the proposed method is to reduce blood loss and prevent perioperative complications (by 60%) [7].
When performing an abdominal delivery, a live female full-term baby was retrieved, weighing 2,600 g, height 51cm and an Apgar score of 8/9.
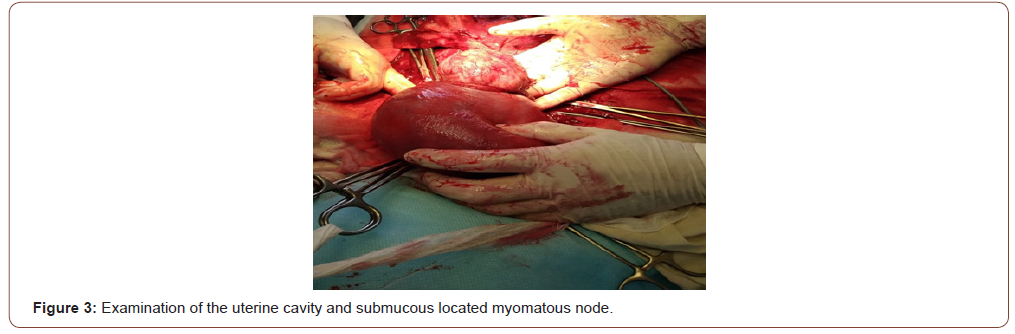
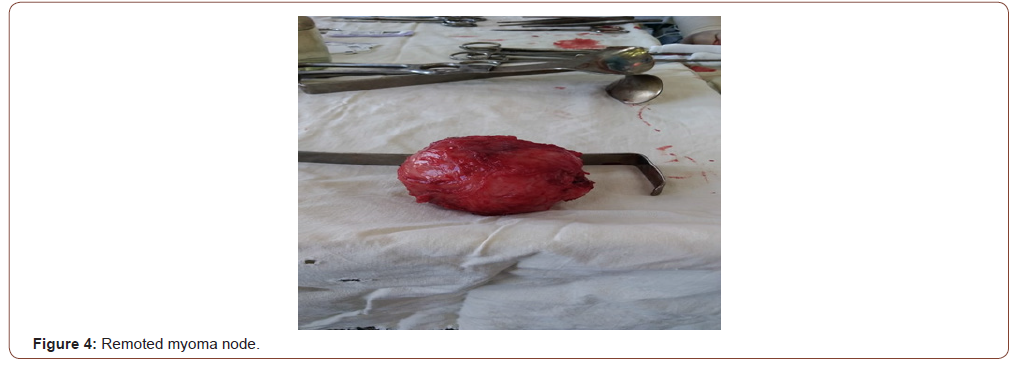
After placing a plastic loop below the incision on the uterus and fixing it in the lock (Figure 2), the uterine cavity was examined and it was found that a submucous node with a diameter of 90 mm, soft consistency was located on the posterior wall of the uterus (Figure 3). Enucleation of the above node was performed (Figure 4), while its bed was sutured with separate vicryl sutures in one row. The total intraoperative blood loss was 450 ml.

Postoperative follow-up of the postoperative woman and her newborn child did not reveal any complications. On the 5th day after the operative delivery, they were discharged from the obstetric hospital.
Thus, a favorable outcome for the mother and the fetus with a submucous location of the myomatous node is possible. However, this can be attributed more to extremely rare cases. When making a decision to maintain pregnancy with the above localization of uterine fibroids, the patient must understand her measure of responsibility for herself and the unborn child. At the same time, the attentive attitude of medical workers to the management of pregnancy with the presence of a pathological condition of the uterus and the use of new technologies for operative delivery contributes to the achievement of a favorable obstetric and perinatal outcome in patients with unusual clinical situations.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Nikitina ES, Rymashevskij AN, Naboka YUL, Rymashevskij MA, Babaeva ML (2016) Vaginal microbiocenosis with uterine myoma. Tavrichesky medical and biological bulletin 2: 104-107.
- Tihomirov AL (2017) Modern medical treatment of uterine fibroids - the ability to avoid hysterectomy and its negative effects. Medical alphabet 10: 17-22.
- Sinchihin SP, Mamiev OB, Magakyan SG (2015) Algorithm of treatment-and-prophylactic tactics of management of patients with uterine myoma. Gynecology 3: 4-8.
- Zajnalova SA, Sinchihin SP, Stepanyan LV (2014) Placental insufficiency issues of etiopathogenesis, diagnosis, clinic and therapy. Astrakhan Medical Journal 2: 15-23.
- Ivanov II, Braude IE (2013) The effectiveness of modern diagnosis and treatment of placental dysfunction during pregnancy. Tavrichesky medical and biological bulletin 2: 159-160.
- Sinchihin SP, Sarbasova AE, Stepanyan LV, Mamiev OB (2017) Prevention of increased blood loss and coagulopathic bleeding during abdominal delivery. Gynecology 19: 46-50.
- Sinchihin SP, Sarbasova AE, Mamiev OB, Stepanyan LV, Ruseckaya NP, et al. (2017) Transient mechanical ischemia of the uterus during cesarean section in young women. Reproductive health of children and adolescents 1: 51-58.
-
Sinchikhin Sergei Petrovich, Stepanyan Lusine Vardanovna. The Unusual Combination of Pregnancy and Uterine Fibroids (Clinical Observation). W J Gynecol Women’s Health. 4(2): 2020. WJGWH.MS.ID.000585.
Giant teratoma, Pelvic mass, Laparotomy, Computed tomography, Epithelial tumors, Ovarian tumors, Carcinoembryonic antigen
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






