 Short Communication
Short Communication
Achieving Tumor Free Margins: Intraoperative Pathology Consultation to Lower Re-Excision Rates at a Community Hospital
Shahrzad Abbassi Rahbar*, Monica Zipple, Amy Kirby, Maya Rauth and Mossum Sawhney
St Joseph Mercy Oakland, USA
Shahrzad Abbassi Rahbar, Department of General Surgery, St Joseph Mercy Oakland Pontiac, USA.
Received Date: November 06, 2018; Published Date: November 16, 2018
Abstract
Objective: Achieving tumor free margins in a single surgery is the primary goal for breast conserving therapy (BCT). It is not uncommon for these patients to undergo more than one operation for positive margins. Within our patient population, lumpectomies requiring re-excision had gross pathological findings that could have warranted further margin excision at the index surgery.
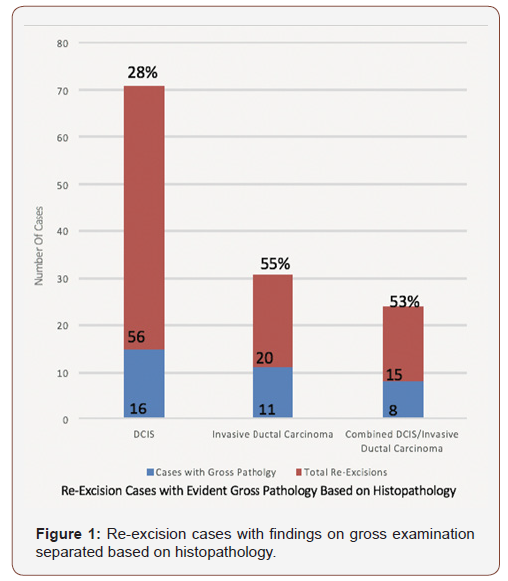
Material and Methods: 579 patients who underwent lumpectomy were reviewed retrospectively from 2010 to 2017. 478 cases of ductal carcinoma in situ (DCIS) and invasive ductal carcinoma (IDC) were included. 91 patients underwent re-excision. Gross specimen findings that came within 2mm margins for DCIS and ink-on-tumor for IDC were considered potentially avoidable re-excisions based on the Society of Surgical Oncology-American Society for Radiation Oncology Consensus Guideline on margins. 35 cases of 91 re-excisions were found to have positive margins on gross pathologic evaluation.
Results and conclusion: The re-excision rate from 2010 to 2017 was calculated to be 19% with an average of 11 women each year. 38% of these patients had grossly positive margins. The re-excision rate according to types of histopathology was 28% for DCIS, 55% for IDC, and 53% for combined DCIS-IDC. The re-excision rate for BCT is 25% in the US. Re-excision surgery has the potential for added discomfort, surgical complications, increased health care cost, and additional emotional stress for patients. Our re-excision rate could have been reduced from 19% to 12%, by over one-third, if intra-operative pathology consultation had been utilized, with the highest impact in patients with IDC and combined DCIS-IDC.
Keywords: Re-excision; Lumpectomy; Breast conserving therapy; Ductal carcinoma in situ; Invasive ductal carcinoma
Introduction
Breast conserving therapy (BCT) is the surgical excision of a tumor followed by whole-breast radiation for breast pathology including DCIS and stage I and II invasive breast cancer. The goal of BCT is to achieve adequate margins at the index surgery. Historically, breast tumor margins were ill-defined and with the lack of consensus on adequate margins in DCIS, the Society of Surgical Oncology (SSO), American Society for Radiation Oncology (ASTRO), and the American Society of Clinical Oncology (ASCO) published guideline recommendations in 2014 and 2016. For stages I and II invasive ductal carcinoma, no ink on tumor is consistent with negative margins and for DCIS, margins free of tumor for least 2mm is adequate. Since this consensus, there was significant decrease seen with ipsilateral tumor recurrence [1].
Achieving tumor-free margins is challenging and close or positive margins after BCT can occur in up to 40% of patients [2]. The incidence of positive margins in DCIS alone after lumpectomy can be up to 57% [3]. Re-excision surgery after lumpectomy poses significant burden on the patient including additional surgery, delay in starting radiation, and added trauma for the patient. It is advisable after multiple failed re-excision procedures to ultimately undergo mastectomy. Reoperation after lumpectomy has been associated with increased rates of bilateral mastectomy [3]. Breast lumpectomies that result in re-excision have the potential for increased health care cost, added discomfort, surgical complications, and emotional stress for patients and their families.
Margin re-excision is the most common cause of reoperation in those undergoing BCT. Various methods have been explored to reduce re-excision rates. Intraoperative frozen section for margin evaluation offers significant reduction in re-excision, however this is not common practice at our institution. This method can be costly and time-consuming especially in a hospital without such resources. Intraoperative pathology consultation for gross evaluation of margins can decrease the need for reoperation and allow a time efficient and cost-effective alternative. To explore ways to reduce our re-excisions per year, we investigated the potential that intraoperative pathology consultation for gross margin evaluation could offer.
Methods
A retrospective chart review was carried out assessing 579 lumpectomy cases over the years 2010 to 2017 at St. Joseph Mercy Oakland. Inclusion criteria consisted of patients who underwent BCT and had pathology results consistent with DCIS, invasive ductal carcinoma, and combined invasive ductal carcinoma and DCIS. Exclusion criteria included other breast pathology and surgeries that utilized intraoperative pathology consultation. 478 lumpectomy cases were thus reviewed and of these, 91 women required re-excision lumpectomy for positive margins. We used the SSO, ASTRO, and ASCO margin guidelines for DCIS and invasive breast cancer. Pathologists’ documentation on gross examination of margins was reviewed and cases with positive margins were considered potentially avoidable re-excisions. 35 such cases were identified.
Results
Given the 91 cases that required re-excision for positive margins found on microscopic evaluation, the re-excision rate over the years 2010 to 2017 was found to be approximately 19%. These lumpectomy cases were further separated based on histopathology including DCIS, invasive ductal carcinoma, and combined DCIS and invasive ductal carcinoma groups. Any positive margin seen on gross examination by the pathologist was considered a reexcision that could have been managed with further excision at the index surgery. In the DCIS group, 56 cases had positive margins on microscopic evaluation and 28% (n=16) of those had positive margins on gross examination. In the invasive ductal carcinoma group, 20 cases had positive microscopic margins and 55% (n=11) of those had findings on gross examination. For the combined group, 15 cases had positive microscopic margins and 53% (n=8) of those had findings on gross examination. The relationship between grossly positive margins and microscopically positive margins is demonstrated in Figure 1. The reason for these differences may be related to the variation in gross pathological findings for DCIS and invasive ductal carcinoma. Invasive ductal carcinoma appears to be a solid tumor with irregular borders infiltrating the adjacent adipose tissue [4]. DCIS on gross examination is not as defined and apparent. It presents with a background of fatty or fibrous tissue and firmness on palpation. Extensive comedo-type DCIS may show more visible pathology with a granular character and necrotic material exuding from the ducts.
The majority of re-excision cases consisted of specimens containing DCIS primarily because obvious abnormality seen on gross examination is rare in DCIS. Conversely, the majority of re-excisions with positive margins seen on gross examination consisted of specimens containing invasive ductal carcinoma.
Conclusion
For community hospitals that may not have resources to conduct intraoperative microscopic margin assessment of lumpectomies, intraoperative pathology evaluation of gross margins may be more feasible.
By analyzing our findings, we were able to identify the potential benefit that intraoperative pathology consultation for gross margin assessment could offer our community. The limitation of gross evaluation includes the potential error that may arise in misdiagnosis without microscopic evaluation. Thus, intraoperative pathology consultation for gross evaluation of margins may offer the highest yield if utilized in invasive ductal carcinoma cases.
Moving forward in surgical practice, lumpectomies for invasive ductal carcinoma identified preoperatively on core needle biopsy can be scheduled to have intraoperative pathology consultation performed. Selective excision of concerning margins identified on gross examination can better ensure negative margins. Overall operative times may remain within average limits even with this additional measure and can be cost-effective [5]. Potentially, intraoperative pathology consultation can be routinely used in lumpectomy procedures requiring margin assessment moving forward.
With the current re-excision rate of approximately 25% in the U.S., the re-excision rate of 19% at our community hospital is below the national average [3]. With the added benefit of intraoperative pathology consultation for immediate evaluation of margins of lumpectomy specimens, our re-excision rate can be lowered by over one-third, to 12%. This can significantly help our community of patients afflicted with breast cancer in north Oakland County and improve their surgical experience while battling this disease.
Acknowledgement
None.
Conflict of interest
No Conflict of Interest.
References
- Morrow M, Van Zee KJ, Solin LJ, Houssami N, Chavez-MacGregor M, et al. (2016) Society of surgical oncology–American Society for radiation oncology–American Society of clinical oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situPract Radiat Oncol 6(5): 287-295.
- Moran MS, Schnitt SJ, Giuliano AE, Harris JR, Khan SA, et al. (2014) SSOASTRO consensus guideline on margins for breast-conserving surgery with whole breast irradiation in stage I and II invasive breast cancer. Int J Radiat Oncol Biol Phys 88(3): 553-564.
- Morrow M, Abrahamse P, Hofer TP, Ward KC, Hamilton AS, et al. Trends in reoperation after initial lumpectomy for breast cancer: addressing overtreatment in surgical management. JAMA Oncol 3(10): 1352-1357.
- Fu YS (1997) DCIS - Ductal carcinoma in situ. TransMed: DCIS Pathology.
- Jorns JM, Visscher D, Sabel M, Breslin T, Healy P, et al. (2012) Intraoperative frozen section analysis of margins in breast conserving surgery significantly decreases reoperative rates: one year experience at an ambulatory surgical center. Am J Clin Pathol 138(5): 657-669.
-
Shahrzad Abbassi Rahbar, Monica Zipple, Amy Kirby, Maya Rauth , Mossum Sawhney. Achieving Tumor Free Margins: Intraoperative Pathology Consultation to Lower Re-Excision Rates at a Community Hospital. W J Gynecol Women’s Health. 1(2): 2018. WJGWH.MS.ID.000510.
-
Re-excision, Lumpectomy, Breast conserving therapy, Ductal carcinoma, In situ, Invasive ductal carcinoma, Tumor, Breast, Ductal carcinoma, Oncology, Trauma, Reoperation, Bilateral mastectomy, Surgical complications, Intraoperative pathology, Fibrous tissue, Comedo type, Misdiagnosis, Biopsy, Battling.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






