 Research Article
Research Article
The Challenge of Female Genital Mutilation
Gharib EL*
Emeritus Professor of Obstetrics & Gynaecology, Tanta University, Egypt
Gharib EL, Emeritus Professor of Obstetrics & Gynaecology, Tanta University, Egypt.
Received Date: December 17, 2018; Published Date: January 24, 2019
Abstract
Female genital mutilation is a worldwide problem, though it is universally prohibited. The aim of this clause is to shed light on his magnitude and importance of this problem in different residential districts and its campaigns and how to get rid of. The definition, historical origin, indications and types of mutilations, technic of performance, and complication are discussed in this clause.
Definition
Female genital mutilation (FGM), also referred to as ‘female circumcision’ or ‘female genital cutting’, refers to all procedures involving partial or full removal of the external female genitals or other trauma to the female genital organs for non-medical grounds [1]. It is a tradition performed in some patriarchal societies to control female sexuality and chastity, reduce women’s sexual pleasure, increase men’s sexual pleasure and/or increase the sexual attractiveness the genitalia [2].
Historical Review
The historical origin of FGM is still unclear. However, we emphasize that its origins predate predates Christianity, Judaism, and Islam. Also, it is worthy to mention that Islamic communities, Christianity, and Judaism also practice female circumcision [3]. Allasraeliat said that Sarah swore to cut three supervision of Hager, Abraham (peace be upon him) said to her: can you justify your right? She said: how to make? He said: prick Her ears, just down, and the cut is circumcision, done, but Allah bless emigrated in her ears, earring, grew up. There is no conclusive indication to show where female circumcision first originated, but circumcised women have been found among the mummies of ancient Egyptians. In the middle of fifth century B.C. Herodotus (the Greek historian) during his travel discovered that the Egyptians were practicing male and female circumcision. A Greek papyrus dated 163 B.C. in the British museum refers to the operations performed on girls in Memphis at the age when they received dowries. Strabo, a Greek geographer, also reported the circumcision of girls as a custom of Egyptian women in 25 BC [4]. The Greek geographer Strabo visited Egypt in about 25 B.C.E. and mentioned that the Egyptians circumcised every child that is born and excised the females. The excision of the females probably consisted in the clitoris and labia minora [5]. Female circumcision is believed to have originated in ancient Egypt during the rule of the Pharaohs. The first confirmed instance of this practice dated back to female mummies in 484 B.C. [6]. The Greek historian Herodotus confirmed the practice of female circumcision in Egypt during his mid-fifth-century B.C. visit to the country. Nile Nubians circumcised nine- and ten-year-old girls with either Sanaa or Pharaonic types [7]. The Egyptian history the mark of circumcision represented slavery and defilement. Certainly, the ancient Egyptians were known to have defiled captured slaves through various forms of mutilation, such as castration or the amputation of other appendages. Circumcision, however, might have been a more cost-effective way to permanently mark human property without the morbidity (and, therefore, loss of productivity) of a slave marked by some other mutilation [8].
A Greek papyrus from 163 B.C. made specific reference to operations performed on girls in Memphis (i.e., the ruined capital of ancient Egypt, located south of present-day Cairo) when they were of age to receive their dowry [9]. The Greek geographer Agatharchides of Cnidus also reported that the practice of excision was prevalent among tribes, on the western coast of the Red Sea. Moreover, the Greek geographer Strabo reported the ritual practice of female circumcision when he visited Egypt in 25 B.C. More specifically, Strabo distinguished “between the operations of circumcision and excision” [10]. Dorkenoo and Elworthy suggest that there are two possible interpretations about its origins: it either developed in Egypt and spread or originated as an African tribal puberty rite that extended to places such as Egypt [11]. It is a bit more difficult to uncover the historical origin of “infibulation,” but it dates to at least the Romans and a procedure they performed on the slaves. “The Romans, to prevent sexual intercourse, fastened a ‘fibula’ or ‘clasp’ through the large lips of women” [4].
Prevalence
Cyberspace is now critical to every nation’s socio-economic, cultural and political activities. When it is disrupted or fails, a country may experience strong adverse effects. On the contrary, its correct functioning and pliability is transforming modern society with exceptional pecuniary and social benefits. With many activities increasingly moving to the Internet, cyberspace has become a new stage for innovations, enterprises, social networking, criminality and war [5] (Figure 1). The above diagram estimated INEC presence in the cyberspace to 0.615. INEC is rated alongside Federal Inland Revenue Service (FIRS), Honeywell Company, Ericsson Nigeria and Interswitch while organizations like Central Bank of Nigeria, Arm Financial service, Arik air and Eko hotel were rated higher than INEC. None of the organization or parastatals rated alongside or above INEC in reality should be rated close to INEC who pride itself of 84million registered voters ahead of 2019 general election. No organization or parastatals can boast of such data; yet it seems INEC is not doing much to make itself more pronounced in the cyber space (Table 1) The table above compares the presence of INEC in the cyberspace with some organizations and personalities in Nigeria. Wizkid, a young Nigerian celeb and Bukola Saraki, a prominent politician both beat INEC in popularity and presence in the social space; whereas INEC with over 84 million voters in its database in reality is more popular than both. More works are needed to be done to improve INEC presence in the social space.
Table 1:Countries in which female genital mutilation of Types I, II, III and IV has been documented as a traditional practice, and number of permanent and temporary residents (both sexes) received in Canada from those countries in the years 2005 to 2009.
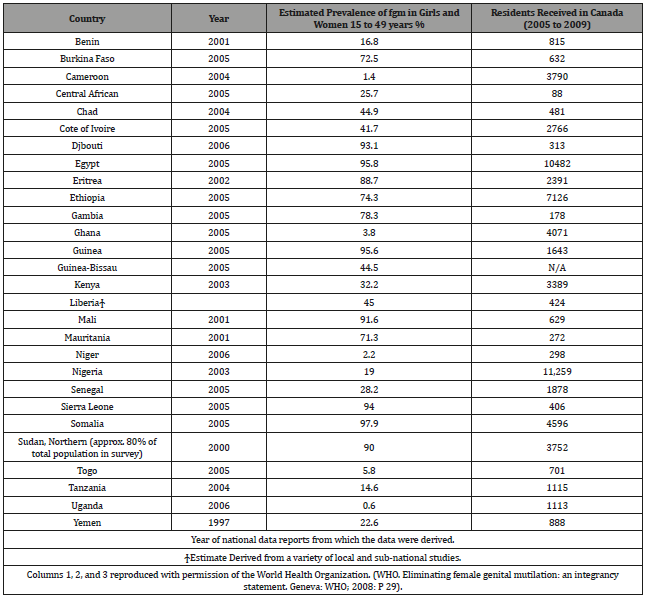
FGH is also practiced among immigrant populations in such countries as Australia, the United States, the United Kingdom, France, Italy, Belgium, Norway, Sweden, and Finland. In the United States alone, over 7,000 women emigrate annually from countries that routinely practice female circumcision [17]. Maher (1996) claims FGM is practiced in over 40 countries [18]. Recent estimates show that in 2012, around 513,000 women and girls in the United States were at risk for FGM/C or its consequences [19]. FGM is illegal in many countries of the world [20]. However, the highly entrenched sense of social obligation overrides any potentially positively modifying influence of legal and moral norms, thereby fuelling the continuation of this practice. The eradication of FGM has been prioritized, as a key issue of the African Union, [21] and the global community [22]. Although FGM/C has been illegal in Egypt for almost 50 years, previous literatures showed that FGM/C, especially in Upper Egypt, is almost universal and reached a high of 73.9%, 75.5% and 85.5% in Beni-Suef, Assiut and Luxor, respectively. Religious, traditional, sexual and hygienic reasons have been reported by advocates of FGM/C, which could explain its high prevalence rates and the intension of many mothers to encourage the continuation of the practice [23]. In the United States, FGM is most common in immigrant communities and in major metropolitan areas. CDC reports using information from the early 2010-2013 have shown a decrease in FGM in the United States, although growing levels of immigration cause numbers to appear higher [24]. In addition to its prevalence in immigrant communities in the US, FGM was considered a standard medical procedure in America for most of the 19th and 20th centuries. Physicians performed surgeries of varying invasiveness to treat a number of diagnoses, including hysteria, depression, nymphomania, and frigidity. The medicalization of FGM in the United States allowed these practices to continue until the end of the 20th century, with some procedures covered by Blue Cross Blue Shield Insurance until 1977 [25]. With the passage of the federal law ban, the Female Genital Mutilation Act in 1996, performing FGM on anyone under age 18 became a felony in the United States [26].
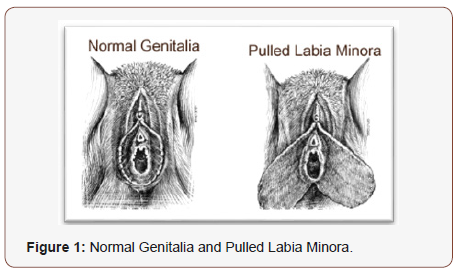
The Procedures of FGM
FGM is carried out using special knives, scissors, razors, or pieces of glass. On rare occasions sharp stones have been reported to be used (e.g. In eastern Sudan), and cauterization (burning) is practiced in some parts of Ethiopia. Finger nails have been used to pluck out the clitoris of babies in some areas in the Gambia. The instruments may be re-used without being cleaned. The operation is usually performed by an elderly woman of the village specially designated this task, who may also be a traditional birth attendant (TBA). Anesthesia is rarely used, and the girl is held down by several women, frequently including her own relatives. The procedure may take 15 to 20 minutes, depending on the skill of the operator, the extent of excision and the amount of resistance put up by the girl. The wound is dabbed with anything from alcohol or lemon juice to ash, herb mixtures, porridge or cow dung, and the girl’s legs may be bound together until healing is completed. In some areas (e.g. parts of Congo and mainland Tanzania), FGM entails the pulling of the labia minora and/or clitoris over a period of about 2 to 3 weeks. The procedure is usually started by an elderly woman designated this task, who places sticks of a special type to hold the stretched genital parts so that they do not revert back to their original size. The girl is instructed to pull her genitalia every day, to stretch them further, and to add additional sticks from time to time to hold the stretched parts. Usually no more than four sticks are used, as further pulling and stretching would make the genitals unexceptionally long (Figure 1).
Indications
The reasons given for this practice have included religious demand, cleanliness, purifications, family honor, a sense of belonging and enhancement of marital opportunities because a circumcised woman is sexually more pleasing to her husband. The closer she is sewn, the more pleasure he receives. An uncircumcised woman would become a social outcast in her community. She would be a girl regardless of her age [27]. From the 19th into the mid- 20th century, doctors in Russia, England, France, and the United States performed FGM as a treatment for hysteria, lesbianism, and masturbation. Circumcision in its mild form will decrease the sexual desire of the girl thus hindering the chances of sexual promiscuity.
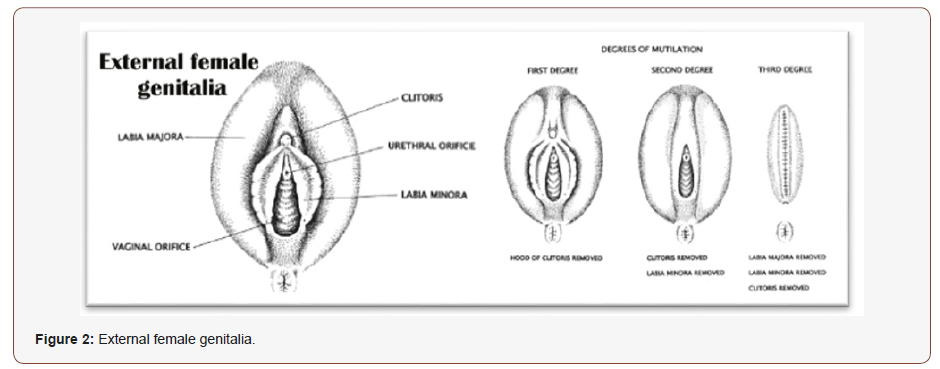
The World Health Organization (2008) has Classified FGM into Four Types: [28]
1. Type I: partial or total removal of the clitoris and/or the prepuce (Type I a removal of the clitoral hood/prepuce only, appears to be rare and is generally performed in medical rather than traditional settings; Type I b, removal of the clitoris with the prepuce).
2. Type II: Partial or total Removal of the clitoris and the labia minora, with or without excision of the labia majora (Type II a, removal of the labia minora only; Type IIb, partial or total removal of the clitoris and the labia minora, Type II c, partial or total removal of the clitoris, the labia I b, minora the labia majora).
3. Type III (infibulation): Narrowing of the vaginal orifice with the creation of a covering seal cutting and positioning the labia minora (Type the labia majora (Type III b), or both, with or without excision of the clitoris.
4. Type IV: Unclassified, all other harmful procedures of the female genitalia for non-medical purposes.
Types of Female Circumcision
Figure 2.
The View of Religions on FGM
1. Adverse to the opinion that it is a practice carried out by Muslims alone, it is also done by Christians and a minority group of Ethiopian Jews. However, FGM is neither mentioned in the Torah, nor in the Gospels, and – like in Islam – bodily mutilation is condemned by both faiths.
2. Granted the fact that some Sunni Muslims, legitimate FGM by quoting a controversial hadith (a saying ascribed to the Prophet Mohammed) in which the Prophet allegedly did not object to FGM provided cutting was not too severe [5, 6] and that the least Invasive type of FGM (partial or full removal of the clitoris and/or the prepuce) is likewise called “Sunna Circumcision” [29].
3. Granting to the Hebrew bible, circumcision is taken for all male Jewish children in observance of God’s commandment to Abraham (Genesis 12-17), female circumcision was never allowed in Judaism, according to the Oxford Dictionary of the Jewish Religion [30].
4. Literature dealing with the Christian view on FGM is very scarce, however, Christian authorities unanimously agree that FGM has no basis in the spiritual texts of Christianity [31].
Complications
Complications of FGM depend on: type (level/classification) performed, the ability of the circumciser, age of the girl, operating conditions (e.g. Lighting, sanitary environment), an instrument used (razors, blunt/sharp knives, or jagged rocks), presence of antiseptics, use of traditional bleeding, reducing products, in addition to other variables. Complications can also be classified as physical (immediate, late, and obstetrical), psychological, and psychosexual. There are two forms of complications that occur during and after the procedure:
Immediate complications
During and immediately following the procedure, hemorrhage, shock, severe pain, infection, damage to adjacent tissue, tetanus, urinary problems -- incontinence, dribbling, recurrent infections, broken bones, sepsis and septicemia, HIV and Hepatitis B infection. Necrotizing fasciitis has been reported. Deaths from FGM have been reported. Other immediate reported complications include damage to other adjacent organs and incomplete healing.
Long term health consequences
FGM causes, complications throughout the life span and these can broadly divide into three main areas: Gynecological, Obstetrical, Psychological, sexual complications.
Gynecological
Long term gynecological concerns that have been linked to FGM include infection, scarring and keloid, menstrual difficulties, urinary symptoms and infertility.
Infection
FGM has been implicated in long term infections, including chronic genital abscesses, vaginal infections and blood borne infections such as Hepatitis B and HIV. A systematic review examined Infection rates in 22 052 African women with FGM of all main types [32]. Types of infections identified included urinary tract infections, genitourinary tract infections, abscess formation, septicemia and HIV. Infections were more frequent in who had undergone Type III FGM. Additionally, a literature review of articles revealed that FGM is a particular risk factor for genitourinary disorders It has been suggested that FGM increases the risk of transmission of Hepatitis B, C and HIV by the use of unsterile and shared instruments. However, although this is plausible, there are no epidemiological studies to support this and in many FGM practicing countries Hepatitis B is endemic and rates of HIV can be high [33].
Genital complications
Genital scarring is a common but can be very variable due to the extent of tissue removed and immediate complication such as infection. Painful and unsightly scarring due to the keloid has been reported. Inclusion cysts over the clitoral area can obstruct the vagina and cause pain. They can be very large and require surgical excision.
Menstrual complications: Painful and prolonged periods have been attributed to FGM, but the mechanisms are unknown. It is possible that a very narrow vaginal opening might slow down menstrual flow and case reports of hepatoscopies do exist.
Urinary complications: Damage to the urethra during FGM may lead to fistula and urethral strictures. Poor urinary flow and recurrent urinary tract infections have been reported in up to 22% of women following FGM and are thought to be due to obstruction of the urethral opening by scar tissue sealing the vagina. It would seem logical to expect that these symptoms are relieved by deinfibulation where the scar tissue is incised but there are no studies to confirm this [34].
Infertility: It has been suggested that FGM leads to infertility, although there is little good data to support this. One study has suggested a link between more extensive FGM, and primary infertility has been suggested. Difficult or painful intercourse because the vagina is infibulated has been suggested as a possible mechanism, as has ascended pelvic infection at the time of FGM [35].
Obstetric complications: FGM increased the risks of prolonged labor, postpartum hemorrhage, perineal trauma and Caesarean section [36]. In addition, there was an increased risk of neonatal resuscitation, low birth rate, stillbirth and early neonatal death with FGM thought to lead to an extra 1–2 perinatal deaths per 100 deliveries [37]. Women who have undergone FGM suffer more frequently from prolonged, difficult labor, have a higher rate of obstetric lacerations, more often require instrumental delivery, and have increased rates of obstetric hemorrhage. This may be due, in part, to the inelasticity of scar tissue. This conclusion is supported by evidence that more invasive forms of FGM cause increased scarring and more significant delays in the second stage of labor [38]. Other studies have also reported an increased rate of perineal tears [39]. and high rates of episiotomy particularly with Type III FGM (infibulation) [40].
Psychological complications: Small studies have identified depression, anxiety and post-traumatic stress disorder (PTSD) [41]. Behrendt and Moritz carried out structured clinical interviews with 47 Senegalese women, assessing their mental health status. Twenty-three of these had undergone FGM as children, most commonly between 4 and 10 years. They found a high prevalence of posttraumatic stress disorder (30.4%) and other psychiatric syndromes, including memory problems (47.9%) in women with FGM. The prevalence of mental health problems in women with FGM was statistically significant compared to the comparison subjects [42].
Sexual complications: There is increasing evidence that FGM damages sexual function and this would seem logical given the removal of sexually sensitive tissue such as the clitoris. Alsibiani and Rouzi recruited 130 sexually active women with FGM and 130 sexually active women without FGM in Jeddah, Saudi Arabia. Each participant completed a version of the Female Sexual Function Index (FSFI) questionnaire translated into Arabic. The results showed no group difference in mean desire score or pain score. However, there were statistically significant differences between the two groups in their scores for arousal, lubrication, orgasm, and satisfaction, as well as the overall sexual function score [43]. A study on UK women depicted a significantly reduced sexual quality of life, based on the Sexual Quality of Life-Female (SQOL-F) questionnaire [44]. Berg and Denison meta-analysis results showed that women who had been subjected to FGM were 52% more likely to report dyspareunia, more than twice as likely to report the absence of sexual desire, and a third of recipients reported reduced sexual satisfaction [45]. Recent surgical reports claim that clitoral reconstruction may restore sexual function [46].
Acknowledgement
None
Conflict of Interest
None
References
- (2016), Female Genital Mutilation/Cutting: A Global Concern UNICEF, New York.
- Abdulcadir J, Margairaz C, Boulvain M, Irion O (2011) Care of women with female genital mutilation/cutting. 140: w 13137.
- Ahmady KA (2015) Comprehensive research study on female genital mutilation/cutting (FGM/C) in Iran.
- Hosken FP (1982) The Hosken report: Genital and sexual mutilation of females, Lexington MA: Women’s International Network News. 15.
- Strabo, Geogeaphicka (1932) XVII, II. In the Strabo of the Loeb Classical Library published.
- Slack AT (1988) Female circumcision: A critical appraisal. Human Rights Quarterly. 10: 437–486.
- Colon AR, Colon PA (2001) A history of children: A socio-cultural survey across millennia. Westport, CT: Greenwood Press.
- Kaicher DC, Swan KG (2010) A cut above: circumcision as an ancient status symbol. J Urology 76(1): 18-20.
- Kouba LJ, Muasher J (1985) Female circumcision in Africa: An overview. African Studies Review. 28 (1): 95–110.
- Bryk F (1934) Circumcision in man and woman: Its history, psychology and ethnology. New York: American Ethnological Press 271.
- Dorkenoo E, Elworthy S (1992) Female genital mutilation: Proposals for change (Minority Rights Group International Rep. No. 92/3) London.
- Ohchr U, Undp U (2008) Eliminating female genital mutilation: an interagency statement. Geneva: WHO.
- Feldman-Jacobs C, Clifton D (2010) Female genital mutilation/cutting: data and trends. Population Reference Bureau, USAID.
- Dorkenoo E, Morison L, Macfarlane A (2001) A statistical study to estimate the prevalence of female genital mutilation in England and Wales: summary report. Foundation for Women’s Health, Research and Development (FORWARD).
- Mahmoud MIH (2016) Effect of female genital mutilation on female sexual function, Alexandria, Egypt. Alexandria J Med 52 (1): 55–59.
- Abdalla, Raquiya HD (1982) Sisters in Affliction: Circumcision and Infibulation of Women in Africa. London: Zed Press 72.
- Burstyn L (1995) Female circumcision comes to America. Atlantic Monthly 276(4): 28–35.
- Maher RH (1996) Female genital mutilation: The struggle to eradicate this rite of passage. Human Rights 23 (4): 12–15.
- Goldberg H, Stupp P, Okoroh E, Besera G, Goodman D, et al. (2016) Female genital mutilation/ cutting in the United States: updated estimates of women and girls at risk, 2012. Public Health Rep 131(2): pp 340-347.
- Rahman A, Toubia N, Rasheed SM, Abed-Ellah AH, Yousef FM (2011) Female Genital Mutilation: A Practical Guide to Worldwide Laws & Policies. Zed Books.
- AU (2011) Decision on the Support of a Draft Resolution at the Sixty Sixth Ordinary Session of the General Assembly of the United Nations to Ban Female Genital Mutilation in the World. African Union, Malabo, Equatorial Guinea.
- UNFPA/UNICEF (2011) Joint Programme on Female Genital Mutilation/ Cutting Accelerating Change Annual Report. New York.
- Arafa AE, Elbahrawe RS, Shawky SM, Abbas AM (2018) Epidemiological and gynecological correlates with female genital mutilation among Beni- Suef University students; cross sectional study. Middle East Fertility Society Journal 23: 184–188.
- Goldberg Howard, Stupp Paul, Okoroh Ekwutosi, Besera Ghenet, Goodman David, et al. (2016) Female Genital Mutilation/Cutting in the United States: Updated Estimates of Women and Girls at Risk, 2012. Public Health Reports 131 (2): 340–347.
- Webber Sara, Schonfeld, Toby L (2003) Cutting History, Cutting Culture: Female Circumcision in the United States. The American Journal of Bioethics 3(2): 65–66.
- 18 US Code § 116 - Female genital mutilation”. LII / Legal Information Institute.
- Abusharaf RM (1998) Unmasking Tradition: A Sudanese Anthropologist Confronts Female circumcision and its Terrible Tenacity. The Sciences 38(2): 22.
- WHO (2008) Eliminating Female Genital Mutilation: An Interagency Statement. World Health Organization, Department of Reproductive Health and Research, Geneva.
- Sunna circumcision (2012) In: Segen’s medical dictionary, Farlex Inc.
- Circumcision, Zwi Werblowsky RJ, Wigoder G (1997) Editors: Oxford dictionary of the Jewish religion. Oxford University Press: New York & Oxford.
- El-Damanhoury (2013) The Jewish and Christian view on female genital mutilation. African Journal of Urology 19: 127–129.
- Iavazzo C, Sardi TA, Gkegkes ID (2013) Female genital mutilation and infections: A systematic review of the clinical evidence. Arch Gynecol Obstet 287 (6): 1137–1149.
- Monjok E, Essien EJ, Holmes L (2007) Female genital mutilation: potential for HIV transmission in sub-Saharan Africa and prospect for epidemiologic investigation and intervention. Afr J Reprod Health 11(1): 33–42.
- Amin MM, Rasheed S, Salem E (2013) Lower urinary tract symptoms following female genital mutilation. Int J Obstet Gynecol 123: 21–33.
- Almroth L, Elmusharaf S, El Hadi N, Obeid A, El Sheikh MA, et al. (2005) Primary infertility after genital mutilation in girlhood in Sudan: a case control study 366: 385–391.
- WHO study group on female genital mutilation and obstetric outcome, Banks E, Meirik O, Farley T, Akande O, Bathija H, et al. (2006) Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries. Lancet 367: 1835–1841.
- Berg RC, Underland V (2013) The obstetric consequences of female genital mutilation/cutting: a systematic review and meta-analysis. Obstet Gynecol Int.
- Browning A, Allsworth JE, Wall LL (2010) The relationship between female cutting and obstetric fistulae. Obstet Gynecol 115(3): 578–583.
- Millogo Traore F, Kaba ST, Thieba B, Akotionga M, Lankoande J (2007) Maternal and foetal prognostic in excised women delivery. J Gynecol Obstet Biol Reprod 36: 393–398.
- Al-Hussaini TK (2003) Female genital cutting: types, motives and perineal damage in laboring Egyptian women. Med Principles Practice 12(2): 123–128.
- Vloesberg E, Vanden Kwaak A, Knipscheer J, Vanden Muijesenberg M (2012) Coping and chronic psychosocial consequences of female genital mutilation in the Netherlands. Ethnicity Health 17(6): 677–695.
- Behrendt A, Moritz S (2005) Posttraumatic stress disorder and memory problems after female genital mutilation. Am J Psychiatry 162 (5): 1000–1002.
- Alsibiani SA, Rouzi AA (2010) Sexual function in women with female genital mutilation. Fertil Steril 93 (3): 722–724.
- Andersson SH, Rymer J, Joyce DW, Momoh C, Gayle CM (2012) Sexual quality of life in women who have undergone female genital mutilation: a case-control study. BJOG 119(13): 1606–1611.
- Berg RC, Denison E (2012) Does female genital mutilation/cutting (FGM/C) affects women’s sexual functioning? a systematic review of the sexual consequences of FGM/C. Sexual Res Social Policy 9 (1): 41–56.
- Foldes P, Cuzinb B, Andro A (2012) Reconstructive surgery after female genital mutilation: a prospective cohort study. Lancet. 380: 134–141.
-
Gharib EL. The Challenge of Female Genital Mutilation. Sci J Research & Rev. 1(3): 2019. SJRR.MS.ID.000512.
Female Genital Mutilation, Magnitude, Campaigns, Historical Origin, Indications, Complication, Memphis, Female Circumcision, Morbidity, fibula, Clasp, Clusters, Obligation, Diagnoses, Including Hysteria, Depression, Nymphomania, Frigidity, Cauterization, Hysteria, Lesbianism, Masturbation, Gospels.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






