 Review Article
Review Article
Central and Lateral Cystocele
Gharib EL*
Emeritus Professor of Obstetrics & Gynaecology, Tanta University, Egypt
Gharib EL, Emeritus Professor of Obstetrics & Gynaecology, Tanta University, Egypt.
Received Date: June 27, 2018; Published Date: December 14, 2018
Introduction
Anterior vaginal wall prolapses or cystocele is by the International Urogynaecological Association (IUGA) defined as a downward descent of the anterior vaginal wall and bladder. A cystocele is a pathological descent of the anterior vaginal wall and bladder base [1].
Etiology
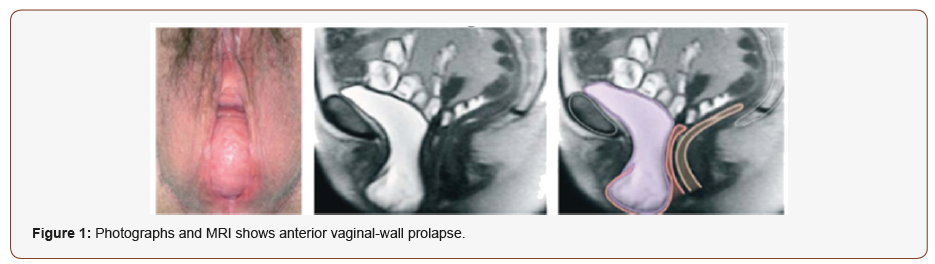
The etiology of prolapse is multifactorial. Advancing age, parity and collagen weakness, drooping, separation of rupture of the pubocervial ligament are all quoted as significant predisposing factors [1]. The risk factors include pregnancy, childbearing, obesity, congenital or acquired connective tissue abnormalities, chronic constipation, family history of POP, denervation or weakness of the pelvic floor, obesity, the menopause and aging [2] (Figure 1).
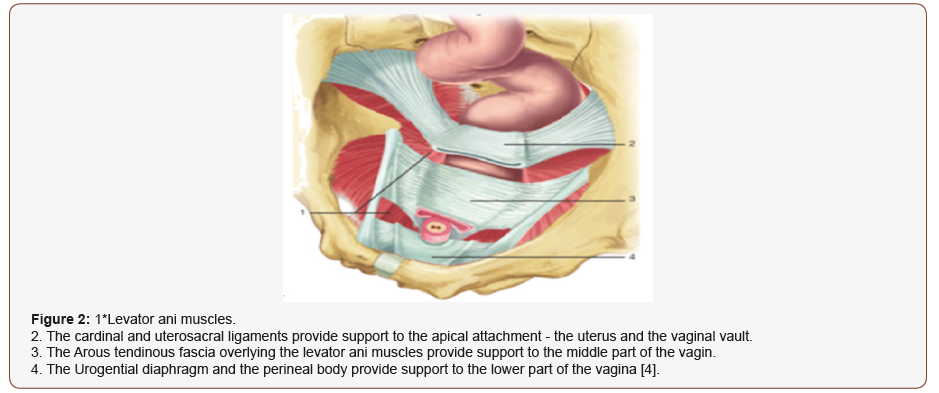
Vaginal delivery, hysterectomy, chronic straining, normal ageing, and abnormalities of connective tissue or connective-tissue repair predispose some women to disruption, stretching, or dysfunction of the levator Ani complex, connective-tissue attachments of the vagina, or both, resulting in prolapse. Epidemiologic studies indicate that vaginal birth and aging are two major risk factors for the development of pelvic organ prolapse [3]. The vaginal walls derive support from the strong fascia and ligaments in the hip. DeLancey [4] described three levels of support to the vagina (Figure 2):
1. Stage 1: The cardinal and uterosacral ligaments provide support to the apical attachment—the uterus and the vaginal vault.
Level 2: The arcus tendinous fascia pelvis and the fascia overlying the levator ani muscles provide support to the middle part of the vagina.
3. Stage 3: The urogenital diaphragm and the perineal body provide support to the lower portion of the vagina.
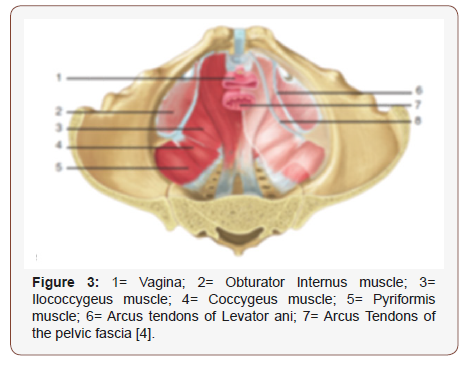
Disruption to any of these social systems will result in a POP, and surgical correction aims to rectify these defects and restore anatomy. Anatomical support of pelvic viscera is mainly supplied by the levator ani muscle complex and connective-tissue attachments of the pelvic organs (endopelvic fascia). Disruption or dysfunction of one or both of these factors can contribute to deprivation of sustenance and, eventually, pelvic organ prolapse. The levator ani muscle complex consists of the pubococcygeus, the puborectalis, and iliococcygeus muscles. These muscles are tonically contracted at rest and act to close the genital hiatus and provide a stable platform for the pelvic viscera as shown in Figure 3. Decline of normal levator ani tone by denervation or direct muscle trauma results in an open urogenital hiatus, weakening of the horizontal orientation of the levator plate, and a bowl-like configuration [4].
Clinical Varieties
One form of anterior vaginal wall descent is due to distension due to stretching of the vaginal wall such that occurs after vaginal delivery. The other is due to displacement of the anterior vagina due to pathological detachment of its funding. Anterior vaginal wall prolapse may be due to central or lateral defects. Central defects result from vertical defects in the endopelvic fascia. Lateral defects result from a detachment of the lateral vaginal wall from the Arcus tendineus fascia pelvis. The central is further divided into anterior and posterior. Prolapse anterior to the interuretic bar (Mercier’s bar) is concerned to as anterior cystocele or urethrovaginal prolapse, whereas prolapse posterior to Mercier’s bar is called posterior cystocele.
Lateral vaginal wall defects were first reported in 1912 by White, who described a vaginal procedure to resuspend the detached, often prolapsed, vagina by suturing its lateral surface of the Arcus tendineus fasciae pelvis. The tendinous arch of the hip is the glacial source of the Levator ani group of muscles, puborectalis, pubococcygeus, and iliococcygeus [5].
Clinical Picture
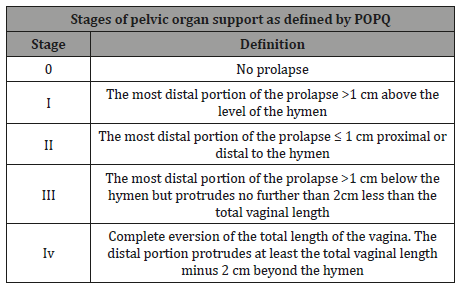
Vaginal bulging is the only symptoms specific to cystocele. Adult females who develop cystocele can present either with one symptom, such as vaginal bulging or pelvic pressure, or with various charges, including many bladder, intestine, and pelvic symptoms. Ellerkmann and colleagues noted that 63% of patients present with bulge symptoms, 73% urinary incontinence, 86% urinary urgency or frequency, 62% voiding dysfunction [6]. Some sexually active women with cystocele complain that their prolapse interferes with sexual role [7] (Table 1).
Table 1:Five stages of pelvic organ support as defined by the pelvic organ prolapse quantitation system.
Ineffective results
The studies showing that ozone treatment does not provide additional benefit to mechanical therapy is available in the literature [20-23]. In an in vitro study, it was reported that ozone was effective on E.fecalis but did not show this effect in biofilm [24]. In another in-vitro study, it was observed that the effect of ozone on microorganisms within organized cryogenic biofilms was minimal. (25).
Evaluation
5.1. Baden-Walker classification grade III–IV (pelvic organ prolapse quantification [POP-Q] system stage III–IV) cystocele is associated with a constellation of abnormalities, including urethral hypermobility, lateral defect, central defect, and concomitant vault and posterior wall prolapse. Patients with Baden-Walker classification grade III–IV cystoceles by definition have the bladder outside the introitus with strain (grade III) or at rest (grade IV) [8].
5.2. Preoperative evaluation included history and physical examination, dynamic pelvic magnetic resonance imaging, Urodynamics, and symptom questionnaire.
5.3. Assessment of bladder neck mobility is an important step in the evaluation of women with stress urinary incontinence. A numeral of methods has been employed for this purpose, including ultrasound, radiographic studies, and the Q-tip test (Figure 4). Because the Q-tip test is simple to perform and inexpensive, it has become a widely used component of the urogynecologic evaluation.
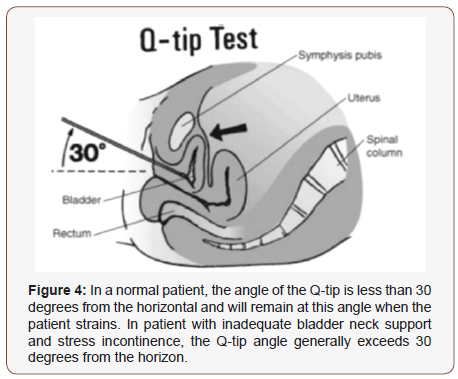
5.4. Crystal et al introduced the Q-tip test and reported that its angle of deflection with straining reflected urethral axis rotation. By comparing the results of radiographic bead chain studies, they found that patients with good urethral support had rotational angles of less than 20° from the horizontal axis. Hence, rotational angles of greater than 30° have generally been considered unreasonable [9].
Treatment
6.1. Successful treatment of anterior vaginal prolapse remains one of the most challenging aspects of pelvic reconstructive surgery. Anterior colporrhaphy has been the standard surgical treatment for anterior vaginal prolapse.
6.2. Current management options for women with symptomatic pelvic organ prolapse include observation, pessary use, and surgery. Cystoceles are mainly treated by anterior colporrhaphy, paravaginal repair, Burch colposuspension and even sacrocolpopexy [10].
6.3. Anterior colporrhaphy corrects anterior vaginal wall prolapse by plicating the layers of vaginal muscularis and adventitia overlying the bladder or by plicating paravaginal tissue in such a way as to reduce the protrusion of the bladder and anterior vagina. Thither is a little advantage seems to be made by placing absorbable mesh over a traditional anterior colporrhaphy.
6.4. Transvaginal mesh repairs have resulted in lower recurrence of anatomical prolapse and marginally reduced symptoms of bulge compared with native tissue repairs. Nevertheless, quality of life does not appear to differ between transvaginal mesh and native tissue repairs.
6.5. Recurrence rates after the traditional anterior colporrhaphy have been reported as high as 30% to 70%. This large failure rate can be attributed to the approximation of attenuated perivesical fascia to the midline for the repair [11].
6.6. Concomitant tension-free vaginal tape-obturator plus modified anterior colporrhaphy with ample lateral are safe procedures for the handling of stress urinary incontinence and with associated cystocele with a high success rate.
Paravaginal defect repair may be performed laparoscopically, abdominally, or vaginally. In this process, the retropubic space of Retzius is entered to reattach the anterolateral vaginal success with its overlying endopelvic fascia to the obturator internus and pubococcygeus muscles and fascia at the point of the Arcus tendineus fascia of the pelvis bilaterally [9] Figure 5) and thus touches on the lateral vagina to its normal place of attachment (De Lancey’s level III support). Burch found Cooper’s ligament to be stronger than the arcus tendinous [5].
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Walters MD, Weber AM (2001) Anterior vaginal prolapse with and without genuine stress incontinence. In: Cardozo L, Staskin D, editors. Textbook of female urology and urogynaecology, (1st edn), England7 Isis Medical Media Ltd, London.
- Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev (4).
- Mant J, Painter R, Vessey M (1997) Epidemiology of genital prolapse: observations from the Oxford Family Planning Association study. Br J Obstet Gynaecol 104: 579.
- De Lancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166, pp. 1717–28.
- Burch JC (1961) Urethrovaginal fixation to Cooper’s ligament for correction of stress incontinence, cystocele, and prolapse. Am J Obstet Gynecol 81: 281-290.
- Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, et al. (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185: 1332-1337.
- Weber AM, Walters MD, Schover LR, Mitchinson A (1995) Sexual function in women with uterovaginal prolapse and urinary incontinence. Obstet Gynecol 85: 483-487.
- Baden W, Walker T (1992) Surgical repair of vaginal defects. Philadelphia JB Lippincott.
- Crystle CD, Charme LS, Copeland WE (1971) Q-tip test in stress urinary incontinence. Obstet Gynecol 38: 313–315.
- Cronje HS (2003) Management of an extremely large cystocele. J Obstet Gynaecol 23: 89-90.
- Weber AM, Walters MD, Piedmonte MR, Ballard LA (2001) Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol 185(6): 1299-1306.
-
Gharib EL. Central and Lateral Cystocele. Sci J Research & Rev. 1(1): 2018. SJRR.MS.ID.000505.
-
Anterior Vaginal; Prolapse; Cystocele; Urogynaecological; Pathological Descent; Pubocervial Ligament; Pregnancy; Childbearing; Obesity; Congenital; Menopause; Hysterectomy; Chronic Straining; Normal Ageing; Abnormalities; Urogenital Hiatus; Urethral Hypermobility; Urodynamics; Symptom Questionnaire; Radiographic Bead Chain; Sacrocolpopexy; Paravaginal Defect
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






