 Case Report
Case Report
Vestibular Migraine-A Diagnostic Dilemma (A Case Report with Review of Literature)
Dr Avinash Bijlani, Sanjana John, Srinivas D and Dr Ravi Nayar*
Madhaw Medical Centre, India
Ravi Nayar, Madhaw Medical Centre, Delhi, India.
Received Date: June 25, 2019; Published Date: July 19, 2019
Abstract
Vestibular migraine has been classified as a specific entity in which vestibular symptomatology presents as part of a migrainous disorder. New and appropriate diagnostic criteria have been proposed by the Barany and International Headache Societies [1]. The diagnosis of vestibular migraine isdetermined on the basis of the patient history and the exclusion of other causes of vertigo [2]. We present a case of vestibular migraine, which no definitive clinical findings [3] and a few nonspecific VNG abnormalities [4]. After exclusion of other conditions and by applying the diagnostic criteria, a diagnosis of Vestibular migraine was made. The patient is being treated conservatively.
Case summary: A 31-year-old woman complained of a few episodes of dizziness and persistent imbalance over the last 2 weeks. She had a long-standing history of episodes of headaches during which she reported intolerance to bright lights and loud sounds. The headaches as well as dizziness were related to periods of stress and mental exertion. She underwent pure tone audiometry, videonystagmography and MRI of the brain which were all within normal limits. A provisional diagnosis of vestibular migraine was arrived based on the history and by ruling out other causes of vertigo. Interventions: She was advised lifestyle modifications in terms of work life balance creation and measures to managestress [5].
Outcome: The patient is asymptomatic to date. She is receiving prophylactic medication for migraine. Regular visits to the therapist are helping in her overall approach to stressfull events in her life.
Conclusion: Vestibular migraine can be diagnosed by a process of exclusion of other conditions after detailed history, evaluation and investigations. Conservative treatment is often adequate.
Keywords: Vestibular migraine; VNG; Lifestyle alterations; diagnostic dilemma; Case report
Introduction
Migraine is one of the common forms of primary headache. Each patient with migraine on this planet is a variant. The term Vestibular Migraine (VM) is used for patients with a past or current history of migraine, presenting with dizziness as the predominant symptom with or without headache. Prosper Meniere, the French physician who first described the vertiginous syndrome that now goes after his name, was a victim of severe migraine himself .The relationship between these two illnesses was suspected, and written about for many years, under various names such as Migraine -Anxiety Related Dizziness (MARD), Migraine-induced Vertigo or Migrainous Vertigo. But it was only in the year 2001 that the International Headache Society and Barany Society reached a consensus on the diagnostic criteria of Vestibular Migraine. Diagnosing vestibular migraine is a challenging task, as Migraine can be present in association with Meniere’s disease [6], BPPV, Epilepsy and often Audio-vestibular investigations and imaging are needed to exclude other peripheral and central vestibular disorders [7].
Case presentation
History: A 31-year-old woman presented with complaints of persistent postural imbalance for two weeks. Superimposed on this, the patient had two short episodes of sensation of dizziness (non-rotatory) which lasted for less than two minutes. These two episodes were not related to change in head position or change in posture. There was an associated mild nausea. There were no aural symptoms. There was no difficulty in walking, speech visual disturbance or any indication of a neurological affliction. She was not on any medications. She had complained of positional vertigo 3 to 4 years ago. This occurred while lying down in bed and turning to either side. The duration of each episode was a few minutes, without related nausea or vomiting. These symptoms spontaneously resolved in 2 weeks. In the past she had migrainous headaches since her school days. The headaches were unilateral, throbbing in nature. She couldn’t tolerate bright light and loud sounds during the headaches. However, the dizziness was not related temporally to the headaches, though the headaches as well as dizziness were related to periods of stress and mental exertion. Clinical examination and Neuro-otology tests: The ears were normal. Romberg’s test and Unterberger’s stepping test were normal. There was no gait abnormality. Pure tone audiometry revealed normal hearing in both ears. Videonystagmography findings (using the Balance Eye VNG (R)) were as follows
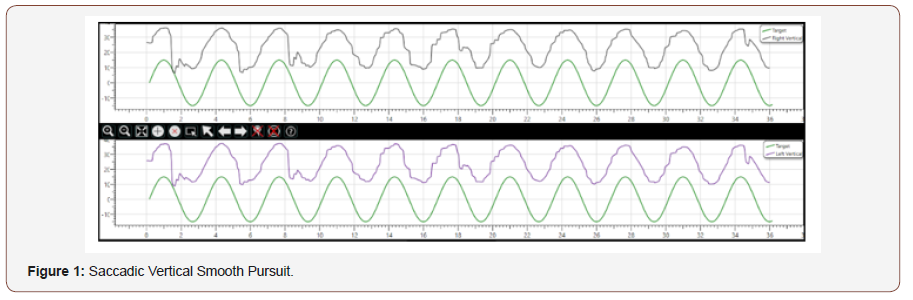
1. A saccadic vertical smooth pursuit.
2. A low amplitude up-beating nystagmus on removal of fixation.
3. A left beating horizontal nystagmus on gaze testing without fixation (Figure 1).
An MRI of the brain was requested (in view of saccadic vertical smooth pursuit and up-beating nystagmus), which was reported as normal. A provisional diagnosis of vestibular migraine was made. Acute treatment of the vertigo was not required, as the patient’s symptoms were mild at the time of presentation. She was advised lifestyle modifications including avoidance of stress [8] For Migraine prophylaxis she was advised Tab Flunarizine [9] which was started in a dose of 5 mg per day which was discontinued after a month and she was advised a close follow up. She is asymptomatic for the past 6 months.
Discussion
Vestibular Migraine (VM) is the recommended term for this condition. The previous terms used were migrainous vertigo, migraine-associated vertigo, migraine-associated dizzinessmigraine-related vestibulopathy [10], Despite the notes on association between episodic vertigo and migraine as early as 1873, VM remained a poorly defined entity [11]. In 1979, Dr Robert Slater, a Neurologist described features of a vertiginous syndrome without auditory symptoms and named it as “benign recurrent vertigo”. The spectrum of VM however is still evolving and more clarity is being obtained through investigation and research. Migraine and vertigo are common neurologic complaints in the general population, each being more common in the presence of the other. The link therefore was initially suspected on the basis of epidemiology. Migraine classically is a headache with or without aura though migraine related conditions can be diagnosed without headache. The aura may be abnormal smells, lights or hallucinations. Vertigo is not an aura like symptom, as its duration is too long and may arise during or after the headache. Other auras may co-exist with vertigo.
Vestibular symptoms commonly seen are spontaneous vertigo, vertigo induced by position, vertigo on exposure to complex visual stimulus, vertigo on head motion, imbalance, dizziness and extreme sensitivity to motion. Typically, VM is spontaneous and positional or spontaneous transforming into positional.VM can affect children as well adults. Females appear to be more affected than males. Various potential mechanisms of pathogenesis have been proposed like stimulation of trigemino- vestibular connections, migraine induced ischemia of inner ear, ion-channel defect, and endolymphatic hydrops in migraine [12,13]. Our patient is a 31-year-oldwoman with a history of long-standing migraine who presented with symptoms of dizziness and imbalance. The features of vertigo which lead us to suspect vestibular migraine include the nature and duration of the first episode of positional vertigo as well as the presence of preexisting migraine since childhood. Positional vertigo is described to occur in vestibular migraine, as either spontaneous or positional or both. It differs from Benign Paroxysmal Positional Vertigo in that the duration of the vertigo episode is longer, lasting often as long as the head position is maintained in the dependant position, the condition often self-limits earlier even without treatment [14].The patient’s episode of positional vertigo fits with this description, hence our initial suspicion. In addition, she complained of nausea, which along with other vegetative symptoms are often described in VM.
There are no conclusive diagnostic tests. In the acute phase there is minimal or no spontaneous nystagmus [15]. Vestibular testing by VNG usually reveals non-specific abnormalities, however the presence of up beating nystagmus as noted in our patient, has been described as a differentiating feature from other vestibular syndromes. However, as this can also suggest a central lesion, she was advised MRI imaging. The other common differentials of VM are Meniere’s disease, BPPV, persistent postural phobic dizziness, brainstem ischemia, migraine with brainstem aura (Formerly Basilar migraine) and vestibular paroxysmia.
The patient did not complain of tinnitus and the audiometry findings were normal enabling us to rule out Menieres disease. The other conditions could be ruled out with a judicious review of history, findings and investigations. The treatment of acute attacks is reserved for episodes lasting longer than 20-30 minutes. This is done using vestibular suppressants such as Meclizine, Dimenhydrinate, Droperidol, Promethazine, Prochlorperazine [16-20]. It is to be noted that the drugs used for acute attacks of vestibular migraine are different from those used to treat acute headaches of migraine. In our case, however we adopted a more conservative approach, as the symptoms had subsided.
Preventive treatment for migraine includes avoidance of triggers and use of drugs for prophylaxis in line with those used to treat classical migraine as suggested by the American Association of Neurology (AAN) namely beta-blockers, tricyclic anti-depressants, calcium channel blockers and some anti-epileptic drugs [21]. Treatment of the co-morbid conditions like anxiety includes physical exercise, lifestyle changes, stress management, diet, which need careful evaluation and long term follow up [22].In our patient, we suggested lifestyle changes to reduce stress and change attitudes to stressful circumstances and used the help of a therapist to ensure continuance of treatment and prevent recurrence of symptoms, with sparing use of prophylactic medications for headache as advised by the neurologists [23].
Conclusion
Vestibular migraine is a difficult diagnosis to make and it requires a high index of suspicion and careful methodical ruling out of other conditions. Awareness of this cause of vertigo is the first step in establishing the diagnosis hence our desire to present this case. The need for neurotologic investigation, and imaging to rule out other differentials and the ability to treat this condition conservatively are highlighted.
Acknowledgements
None.
Conflict of interest
No conflict of interest.
References
- Sohn JH (2016) Recent Advances in the Understanding of Vestibular Migraine. Behav Neurol 180-1845.
- Lee H, Jen JC, Cha YH, Nelson SF, Baloh RW (2008) Phenotypic and genetic analysis of a large family with migraine-associated vertigo. Headache 48(10): 1460-1467.
- Lempert T, Olesen J, Furman J, Waterston J, Seemungal B, et al. (2012) Vestibular migraine: diagnostic criteria. J Vestib Res 22(4): 167-72.
- Furman JM, Marcus DA, Balaban CD (2013) Vestibular migraine: clinical aspects and pathophysiology. Lancet Neurol 12(7): 706-715.
- Neuhauser HK, Raudtke A, Von Breven, Feldmann M, Lezius F, et al. (2006) Migrainousvertigo: prevalence and impact on quality of life. Neurology 67: 1028-1033.
- Radtke A, Lempert T, Gresty MA, Brookes GB, Bronstein AM, Neuhauser H (2002) Migraine and Meniere’s disease: is there a link? Neurology 59(11): 1700-1704.
- Barbosa F, Villa TR (2016) Vestibular migraine: diagnosis challenges and need for targeted treatment. Arq Neuropsiquiatr 74(5): 416-422.
- Lauritsen CG, Marmura MJ (2017) Current Treatment Options: Vestibular Migraine. Curr Treat Options Neurol 19(11): 38.
- Liu F, Ma T, Che X, Wang Q, Yu S (2017) The Efficacy of Venlafaxine, Flunarizine, and Valproic Acid in the Prophylaxis of Vestibular Migraine. Front Neurol 11: 8-524.
- Bikhazi P, Jackson C, Ruckenstein MJ (1997) Efficacy of antimigrainous therapy in the treatment of migraine-associated dizziness. Am J Otol 18(3): 350-354.
- Dietrich M, Obermann M, Celebisoy N (2016) Vestibular migraine: the most frequent entity of episodic vertigo. J Neurol 263: 82-89.
- Foster CA, Breeze RE (2013) The Meniere attack: An ischemia/ reperfusion disorder of inner ear sensory tissues. Medical Hypotheses 81(6): 1108-1115.
- Liu IY, Ishiyama A, Sepahdari AR, Johnson K, Ishiyama G (2016) Bilateral Endolymphatic Hydrops in a Patient with Migraine Variant Without Vertigo: A Case Report. Headache: The Journal of Head and Face Pain 57(3): 455-459.
- Von Breveren M, Radtke A, Clarke AH, Lempert T (2004) Migrainous Vertigo presenting as episodic positional vertigo. Neurology 62(3): 469- 472.
- Ana H Kim, Michele M Gandolfi (2005) Migraines as a source of Vestibular Disorders: Diagnosis and management. In: Vertigo and Disequilibrium-A practical guide to diagnosis and Management (2nd edn.), Peter Weber. Thieme New York, USA, Chapter 16: 170-173.
- Polensek SH, Tusa RJ (2010) Nystagmus during attacks of vestibular migraine: an aid in diagnosis. Audiol Neurootol 15(4): 241-246.
- Shih RD, Walsh B, Eskin B, Allegra J, Fiesseler FW, et al. (2017) Diazepam and Meclizine Are Equally Effective in the Treatment of Vertigo: An Emergency Department Randomized Double-Blind Placebo-Controlled Trial. J Emerg Med 52(1): 23-27.
- Scholtz AW, Ilgner J, Loader B, Pritschow BW, Weisshaar G (2015) Cinnarizine and dimenhydrinate in the treatment of vertigo in medical practice. Wien Klin Wochenschr 128(9-10): 341-347.
- Thomas MC, Musselman, ME, Shewmaker J (2014) Droperidol for the Treatment of Acute Migraine Headaches. Ann Pharmacother 49(2): 233- 240.
- Deitrick CL, Mick DJ, Lauffer V, Prostka E, Nowak D, et al. (2015) A Comparison of Two Differing Doses of Promethazine for the Treatment of Postoperative Nausea and Vomiting. J Perianesth Nurs 30(1): 5-13.
- Hoy SM, Scott LJ (2011) Indomethacin/Prochlorperazine/Caffeine. CNS Drugs 25(4): 343-358.
- Cavalcante Salmito MC, Duarte JA, Morganti LO (2017) Prophylactic treatment of vestibular migraine. Braz J Otorhinolaryngol 83(4): 404- 410.
- O Connell Ferster AP, Priesol AJ, Isildak H (2017) The clinical manifestations of vestibular migraine: A review. Auris Nasus Larynx 44(3): 249-252.
-
Dr Avinash Bijlani, Sanjana John, Srinivas D, Dr Ravi Nayar. Vestibular Migraine-A Diagnostic Dilemma (A Case Report with Review of Literature). On J Otolaryngol & Rhinol. 1(5): 2019. OJOR.MS.ID.000521.
-
Vestibular Symptomatology, Headache, Migraine, Sensation of Dizziness, Paroxysmia, Brainstem Ischemia, Dimenhydrinate, Droperidol
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






