 Case Report
Case Report
Sinonasal Tumor Associated with Paraneoplastic Syndrome
Zubair Ahmed1*, Syed Umair Iftikhar2 and Syed Ahmad Shakeel Ahsan3
1FCPS.FICS, FRCS Professor of ENT, University of Lahore, Pakistan
2Senior registrar Department of ENT, University of Lahore, Pakistan
3Consultant ENT Surgeon, Surraya Azeem hospital, Lahore, Pakistan
Zubair Ahmed, FCPS, FICS, FRCS Professor of ENT, University of Lahore, Pakistan.
Received Date: August 21, 2023; Published Date: September 07, 2023
Abstract
Sinonasal tumors are rare constituting less than 3% of head-neck tumors. A rare form of sinonasal tumors is Glomangiopericytima, which a tumor of low malignant potential and doesn’t metastasize. Of the few cases described in literature, none has been shown to be associated with paraneoplastic syndrome. Later are remote effects of a tumor not because of primary tumor or its metastasis.
We present a case of Glomangiopericytoma of nose, in a 34-year old male, which was associated with paraneoplastic features in the form of unexplained high levels of PTH and pathological fractures of both femurs. He did not respond to conventional medical treatment and was considered to be due to ectopic PTH secreted by tumor. The tumor was successfully removed surgically through mid-facial degloving approach, after which paraneoplastic manifestations disappeared.
Keywords:Sinonasal tumor; Glomangiopericytoma nose; Paraneoplastic syndrome
Introduction
Sinonasal tumors are not common; they account for less than 1% of all malignant tumors and less than 3% of all head and neck carcinomas [1]. Common malignant sinonasal tumors include squamous cell carcinoma, lymphoepithelial carcinoma, undifferentiated nasal-sinus carcinoma adenocarcinomas, and neuroendocrine tumors [2] while Common benign tumors are Osteoma , inverted papilloma and hemangioma are the common benign tumors [3] Glomangiopericytoma is borderline tumor or a tumor of low malignant potential which is a variant of hamangiopericytoma. This tumor arises from pericytes surrounding the blood vessels. It is very rare and constitutes 0.5% of sinonasal neoplasms [4] only few cases have been described in literature.
Paraneoplastic syndromes are remote manifestations of a tumor which are not due to the tumor itself or its metastasis. Instead they are due to hormones or peptides produced by the tumor [5] . Their manifestations can be neurological, hematological, endocrine or musculoskeletal etc [6] Common tumors associated with paraneoplastic syndromes are lung, ovarian, lymphatic, or breast cancer, [7] By and large, they have been described in association with malignant tumors. We describe here a case of paraneoplastic syndrome associated with Glomangiopericytoma, a rare sinonasal neoplasm, associated with paraneoplastic syndrome. No such case has been described in literature to best of our knowledge.
Case Report
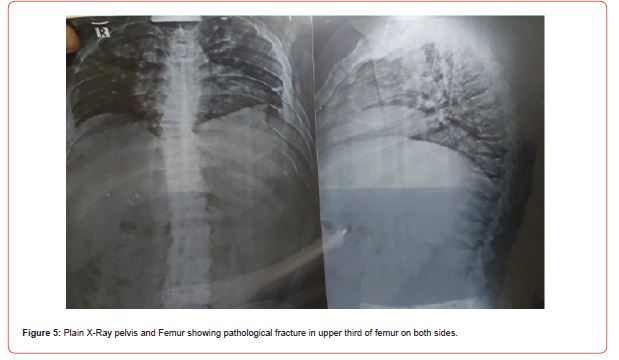
A 34-year-old male presented in ENT department with the complaint of progressive nasal obstruction for the last 18 months. He also complained loss of smell, dull headache and occasional bleeding from nose. There was no history of pain or fever. He had no ocular complaints and had normal vision. About two months after his nasal complaints patient developed pain over upper end of femur and shortly afterwards, he could not bear weight on his legs and could walk with support only; in addition he developed kyphosis and scoliosis in lumber region. He also noticed shortening in his height by about 2 inches.
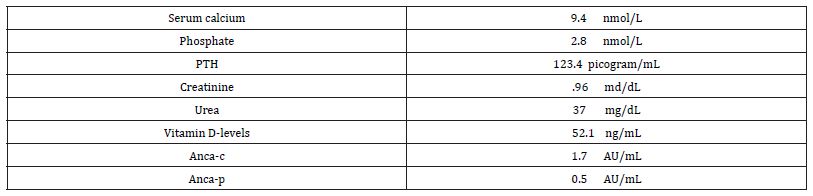
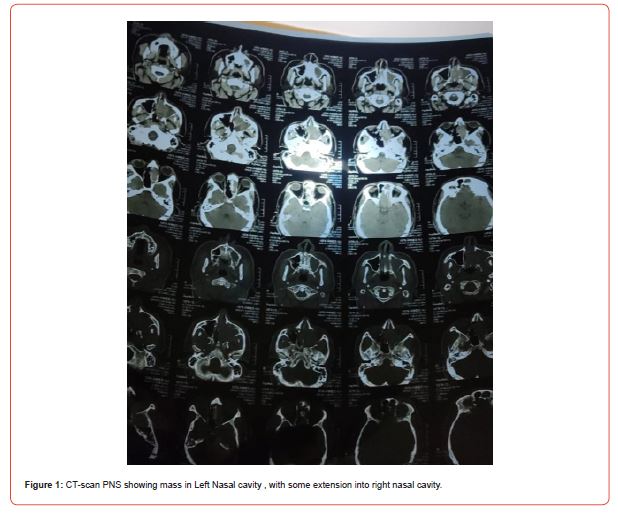
On nasal examination there was no external deformity; air-way was reduced on both sides, more so on left. Anterior rhinoscopy and nasal endoscopy revealed a fleshy polypoidal mass which was filling the left nasal cavity and partially occluding the right. Nasal septum was deflected to right side. No extension of the mass was seen on posterior rhinoscopy. His eyes were normal; there was no proaptosis, restriction of eye-ball movement, defect in visual acuity or visual field defect. No neck node was palpable on cervical examination. Orthopedic examination revealed kyphosis and scoliosis in lumber region to the right side. The patient showed limping gait and could not walk without support. There was tenderness at the upper end of femur on right side. Muscle power was decreased in right lower limb. Superficial and deep reflexes were normal. There was no sensory deficit No swelling of joints was noted.
Investigations
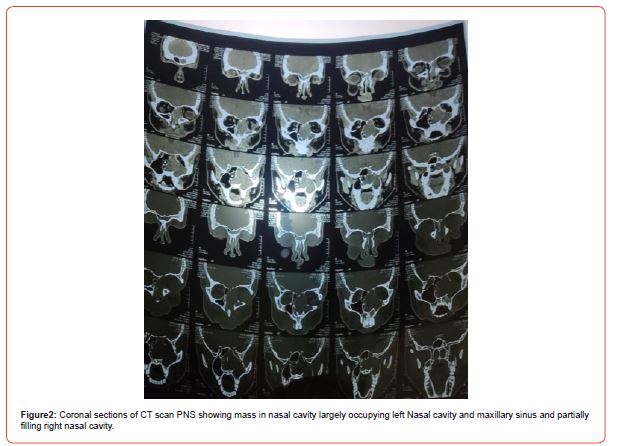
Investigations revealed pathological fractures of both femurs in upper third. In addition, CT-scan of the spine revealed compression fractures of L-4/5. Investigations for pathological fracture revealed elevated PTH; however, no source could be found. There was no evidence of adenoma on MIBI scan. Remaining panel of investigations is presented below.
Table 1:
Patient remained under c/o rheumatologist and orthopedic surgeon. He was prescribed NSAIDS, Calcium-vitamin D preparations and biphosphates. However, no improvement was seen despite extensive medical treatment. It was assumed that high PTH, pathological fractures were result of ectopic hormone secretion by tumor. After detailed investigation and counselling, we planned surgical removal. The tumor was removed through midfacial degloving approach, along with use of endoscope to achieve complete clearance. His recovery was uneventful; the symptoms started improving 3-4 weeks after surgery; PTH level came back to normal, pathological fractures showed signs of healing and after two months patient was able to walk upright, without any support. He is under regular follow-up and there is no sign of recurrence two years after removal.
Discussion
First case of GPC was described by Stout and Murray in 1942 [3] earlier they were considered as a type of hamangiopericytoma. In 1945, WHO categorized it as a separate entity because of distinct histopathological features and distinct immunostaining pattern [8]. They arise from the pericytes of blood vessels and have potential for local spread but distant metastasis has not been described . Grossly, tumor grossly appears as fleshy polypoidal mass which may bleed on palpation. Histologically it is non-encapsulated and subepithelial tumor composed of tightly packed spindle cells. On immunohistochemistry the tumor stains positively with vimentin and betacatenin but is negative for keratin and desman . It shows limited mitotic activity and atypia, as compared to aggressive tumors. That is why it is considered as tumor of low or borderline malignant potential [6]. In literature few cases that have been described, none has highlighted distant metastasis.
Paraneoplastic syndromes are the complex signs and symptoms thought to be produced by hormones or peptides produced by the tumors [7]. Though they have been described in association with many malignancies, reports relating to sinonasal tumors are rare. We could find only one case olfactory neuroblastoma that was associated with paraneoplastic syndrome [9]. There has been no report so far describing paraneoplastic syndrome associated with Glomangiopericytoma.
Our case was different in many aspects; firstly, our case was male (though a female preponderance has been described). Secondly, our case was 34 years old whereas these tumors commonly occur in 6th and 7th decade [8]. However the unique and distinctive feature of our case is association with paraneoplastic features. Sinonasal tumors are rarely if at all, associated with PNS. We could find only one case report of olfactory neuroblastoma associated with PNS [9]. Despite exhaustive search we couldn’t find any case of Glomangiopericytoma associated with PNS.
Two mechanisms have been described for presentation of paraneoplastic syndromes; one is secretion of hormones or peptides by them. For example, syndrome of inappropriate ADH secretion in small cell Ca of lung [10]. Second is through an autoimmune mechanism in which tumor cells show cross reactivity with indigenous tissues of the host [11]. We believe this due to the former because we found high level of PTH, possibly causing pathological fractures of both femurs. There was no evidence in favor of autoimmune pathology as ESR was low and levels of ANCAc and ANCAp were not elevated.
Further evidence comes from the fact the patient had been treated with different drugs such as NSAIDS, Calcium phosphate and Vitamin D preparations before surgical removal, but no improvement was seen. However, two months after surgical removal all musculoskeletal manifestations disappeared.
Treatment of Glomangiopericytoma is largely surgical; generally results of surgical removal are good [4]; there are chances of recurrence however [12]. Our case has not shown any recurrence in 2-year post surgery. We did not use and adjuvant radiotherapy or chemotherapy.
We believe our case is first and only one of its kind described in literature. It adds some new information to the medical literature that paraneoplastic syndromes can occur in borderline lie tumors and tumors of low malignancy as well and should be kept in mind in differential diagnosis and screening of paraneoplastic syndromes.


Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Malignant Tumors of the Nasal Cavity: Practice Essentials, Epidemiology, Etiology.
- Bracigliano A, Tatangelo F, Perri F, Di Lorenzo G, Tafuto R, et al. (2021) Malignant Sinonasal Tumors: Update on Histological and Clinical Management. Curr Oncol 28(4): 2420-2438.
- Benign Sinonasal Tumor Symptoms, Diagnosis & Treatment | Pacific Eye & Ear Center.
- Roy NP, Desai DP, Jain SA (2015) Glomangiopericytoma of nasal cavity. Indian J Pathol Microbiol 58(4): 554-556.
- Kono M, Bandoh N, Matsuoka R, Goto T, Akahane T, et al. (2019) Glomangiopericytoma of the Nasal Cavity with CTNNB1 p.S37C Mutation: A Case Report and Literature Review. Head Neck Pathol 13(3): 298-303.
- Kazi AA, McDougal EM, Howell JB, Schuman TA, Nord RS (2021) Glomangiopericytoma: a case series with review of literature. Braz J Otorhinolaryngol 88(5): 817-820.
- Paraneoplastic Syndromes | National Institute of Neurological Disorders and Stroke.
- Al-Jobory YM, Pan Z, Manes RP, Omay SB, Ikuta I (2021) Sinonasal Glomangiopericytoma: Review of Imaging Appearance and Clinical Management Update for a Rare Sinonasal Neoplasm. Yale J Biol Med 94(4): 593-597.
- Kunc M, Gabrych A, Czapiewski P, Sworczak K (2015) Paraneoplastic syndromes in olfactory neuroblastoma. Contemp Oncol 19(1): 6-16.
- Chung C, Allen E, Umoru G (2020) Paraneoplastic syndromes: A focus on pathophysiology and supportive care. Am J Health-Syst Pharm 79(22): 1988-2000.
- Pelosof LC, Gerber DE (2010) Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment. Mayo Clin Proc 85(9): 838-854.
- Harvey RJ, Sheahan PO, Schlosser RJ (2009) Surgical Management of Benign Sinonasal Masses. Otolaryngol Clin North Am 42(2): 353-375.
-
Zubair Ahmed*, Syed Umair Iftikhar and Syed Ahmad Shakeel Ahsan. Sinonasal Tumor Associated with Paraneoplastic Syndrome. On J Otolaryngol & Rhinol. 6(4): 2023. OJOR.MS.ID.000641.
-
Sinonasal tumor, Paraneoplastic syndrome, Glomangiopericytima, Nasal sinus carcinoma, Sinonasal neoplasms, Malignant tumors, Headache, Loss of smell, ENT, Nasal septum
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






