 Case Report
Case Report
Management of Suicidal Cut Throat Injury: Lessons Learnt
Akhila Albert1, Nambiar Sapna S2*, Susmitha VP3 and Nigil Sreedharan4
1Junior Resident ENT, Department of ENT, Govt Medical College Kozhikode, Kerala, India
2Associate Professor (ENT), Department of ENT, Government Medical College Kozhikode, Kerala, India
3Senior Resident, Department of ENT, Government Medical College Kozhikode, Kerala, India
4Assistant Professor (ENT), Department of ENT, Govt Medical College Kozhikode, Kerala, India
Nambiar Sapna S, Associate Professor (ENT), Department of ENT, Government Medical College Kozhikode, Kerala, India.
Received Date: September 19, 2023; Published Date: October 11, 2023
Abstract
Background: Cut throat injury (CTI) is an emergency requiring the services of an otolaryngologist. The various vital structures in the neck make it an important site with the likelihood of life threatening complications. Besides the airway, injuries to the neurovascular structures and gastrointestinal tract can also affect the treatment and likely outcome. Swallowing difficulty, cough requires evaluation and treatment for complete recovery.
Case report: We report the case of a 35 year old farmer brought with alleged history of self inflicted cut throat injury. The patient had a lacerated wound anterior neck with multiple hesitation cuts, the laryngeal inlet was exposed and thyrohyoid membrane breached. Emergency tracheostomy with neck exploration and wound closure was done successfully but swallowing difficulty with cough in the post operative period was disturbing. Meticulous evaluation with video laryngoscopy and FEES helped diagnose aspiration of saliva which was corrected with compensatory maneuvers and dietary modifications.
Conclusion: Cut throat injury is an emergency that requires not only airway and voice restoration but also swallowing assessment. Dysphagia with or without aspiration deserves meticulous evaluation, use of appropriate investigations followed by tailor made rehabilitation ensuring improved quality of life
Keywords:Cut throat injuries; Dysphagia; Laryngeal nerve injury
Introduction
Cut throat injuries are one among the emergencies that an otolaryngologist is called to manage. Open or incised injuries or those resembling incised injuries in the neck inflicted by sharp objects such as razor, knives, or broken bottle pieces or glasses that may be superficial or penetrating in nature may be described as ‘cut-throat injuries’ (CTIs) [1]. They may result from accident, homicide or suicide attempt.
According to the WHO, almost one million people commit suicide and 20 times more people attempt suicide every year. The global mortality rate is 16 per 100, 000 [2]. An Indian study showed that the highest suicide rate was in the 15-29 years age group (38 per 100,000 population) followed by the 30-44 years group (34 per 100,000 population) [3]. Cut throat injury cases definitely increased during COVID19 pandemic with most common mode of injury being suicidal attempt, which may be due to economical and psychological imbalance during COVID-19 pandemic, due to loss of job, fear of COVID-19 disease, anxiety, loss of hope of living, detached from near to dears and social stigma [4]. Cut throat injuries are potentially life threatening because of the many vital structures in the neck which may be affected leading to severe haemorrhage, air embolism or respiratory obstruction and death. Prompt management with securing air way, maintaining haemostasis and proper post operative care helps decrease morbidity and mortality. However the morbidities following CTI need special mention as they must be managed efficiently to ensure good quality of life post treatment. Laryngeal nerve injuries following cut throat injury results in swallowing difficulties and complications like increased risk of aspiration, aspiration induced pneumonia, delayed resumption of oral intake/malnutrition, decreased quality of life. Postoperative nutrition is an important area to be considered for deep neck wounds with nerve injuries due to delayed tolerance to oral feeding till the regeneration of sensory nerves [5]. The purpose of this case report is to emphasise the importance of rehabilitation of patients with laryngeal nerve injuries following cut throat injury.
Case Report
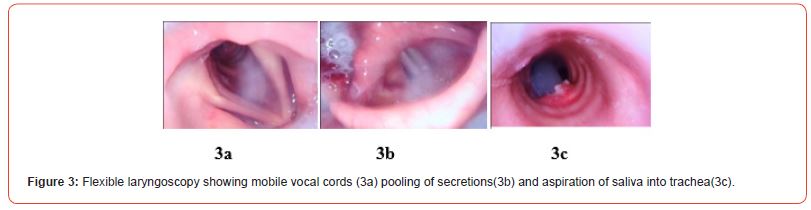
A 35 year old male farmer was bought with alleged history of self-inflicted cut throat injury. Patient was on psychiatric treatment for depression for one year. On examination patient was conscious and responding to commands. He had a lacerated wound on the neck of approximately 10*4*2 cms with multiple hesitation cuts as seen in Figure 1. The laryngeal inlet was exposed with the airway exteriorised owing to the defect in the thyrohyoid membrane. On inspection there was no evidence of contusion or swellings in the neck. Both carotids were well felt and thyroid cartilage was found divided at the level of thyroid prominence along with the petiole of epiglottis exposed. The patient was immediately shifted to the operation theatre for emergency tracheostomy and neck exploration. Tracheostomy was done followed by neck exploration with wound closure under general anaesthesia. The wound was explored with no evidence of any major vascular injury, the cricoid cartilage and its perichondrium was preserved. The defect in the thyrohyoid membrane was visualized; edges freshened and defect closed using 3-0 vicryl. The defect in the thyroid cartilage was closed using non absorbable sutures with care such that the approximation is effective without the suture material giving way. The wound was closed in layers. The challenge during closure is in meticulous approximation with laryngeal inlet and vocal cord alignment maintained and laryngeal mucosa preserved. The nasogastric tube (Ryle’s tube no. 12) was passed intra-operatively following wound repair. Figure 2 Postoperative period was uneventful. However in view of decreased sleep and restlessness psychiatric consultation was done and appropriate medications started. However the patient had difficulty in swallowing with cough even while swallowing saliva. Owing to the persistence of this flexible laryngoscopy was done which revealed normal mobile bilateral vocal cords with aspiration of saliva during swallowing as seen in Figure 3. Functional endoscopic evaluation of swallowing (FEES) showed a PAS score of 7. In view of this patient was asked to continue ryle’s tube feeds and rehabilitaion exercises were taught with feeding under supervision for a week. He was discharged with tracheostomy tube and nasogastric tube and advised regular follow up. The larynx was monitored with flexible laryngoscopy and FEES for improvement in aspiration of fluids into trachea which showed an improvement of PAS score to 2 in 8 weeks. The patient was decannulated after 12 weeks with re-establishment of phonation, swallowing and breathing.

Discussion
Cut throat injuries are usually homicidal. Suicidal cut throat injuries with penetrating airway injuries in the neck are relatively uncommon [6]. Review of literature shows suicidal injuries are common in male than female [7]. Mental illness associated with suicide may be schizophrenia, anxiety disorder, posttraumatic stress disorder, delirium, dementia, and substance abuse. A positive family history is also regarded as a precipitating factor. More violent and deeper cut injuries were noticed in patients of psychosis and schizophrenia [8]. In our case report the patient was a known case of depression with substance abuse. As per the relatives he had committed suicide by slitting his throat with a kitchen knife which is a very uncommon mode because of it being extremely painful. Suicidal incised neck wounds are classically numerous, being characterised by a number of cuts at the superior end of the wound known as tentative cuts/hesitation marks. Their presence suggests self-infliction, indicating repeated attempted cuts being stopped because of pain or hesitancy before finally cutting through the skin. Tailing of the wound and absence of defensive wounds are also features of suicidal cut throat injury. The multiple hesitation wounds in the neck of our patient helped in the diagnosis.
Injuries of the neck are divided into three anatomic zones according to Roon and Christensen’s classification [9]. Zone I injuries occur at the thoracic outlet, which extends from the level of the cricoid cartilage to the clavicles. Zone II is superior to zone I injuries and occurs in the area between the cricoid and the angle of the mandible. Injuries here are the easiest to expose and evaluate. Zone III injuries are between the angle of the mandible and the base of the skull. The predominance of Zone II injuries is attributable to the fact that it is not protected by bony structures making it more vulnerable to injuries. Our patient too had the CTI in Zone II. The common morbidity following CTI is secondary wound infection (23.52%), persistent dysphagia (23.54%) and ugly scar (17.64%) as in the study by Sharma K, et al. The persistent difficulty in swallowing with cough was cause of concern in our patient in the post operative period.
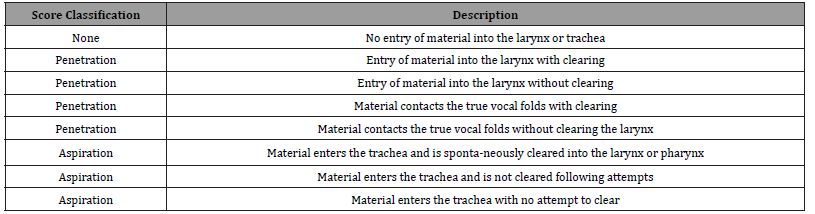
The dysphagia following CTI can be distressing with need for early evaluation and appropriate treatment. Instrumental tests such as flexible endoscopic evaluation of swallowing (FEES) or the video fluoroscopic swallowing study (VFSS) may be regarded as the gold standard of dysphagia assessment in critically ill patients [9]. FEES utilizes the fiberoptic nasopharyngolaryngoscope to evaluate the anatomy and physiology of the pharynx and larynx and certain aspects of pharyngeal swallowing function. The endoscopic evaluation of swallowing has two basic parts. The first is an examination of the structures and function of the pharynx and larynx, including assessment of the patient’s ability to manage secretions. The second part involves presentation of food and a liquid as the swallow is assessed. Further, sensation testing can be performed using short blasts of air to the supraglottic mucous membrane for assessment of vocal cord adduction, a technique known as flexible endoscopic evaluation of swallowing with sensory testing (FEESST). Swallowing function parameters evaluated include pharyngeal pooling of secretions, premature spillage, laryngeal penetration, aspiration, residue, vocal fold mobility, gag reflex, and laryngeal adductor reflex. In FEES, severity of penetration or aspiration is assessed using a penetration and aspiration (PAS) scale 1 indicating no penetration and 8 indicating aspiration without coughing, i.e., silent aspiration as in Table 1 [10].
The treatment of dysphagia in critically ill patients is challenging. Generally three major therapeutic pillars for dysphagia treatment include: dietary texture modifications, postural changes/compensatory maneuvers and interventions aiming to improve swallowing function [11]. Special swallowing techniques, e.g. supraglottic swallowing, may support patients with delayed swallowing reflex or incomplete laryngeal closure. The patient would then be trained to hold the breath before and during swallowing and forced to cough immediately afterwards to optimize glottic/throat clearance. For patients with impaired laryngeal elevation, reduced tongue force or dysfunctional opening of the upper esophageal sphincter (UES), the Mendelsohn maneuver can be applied. In this maneuver, during oral preparatory stage, the patient presses the bolus as forcefully as possible against the hard palate for up to 3sec. This elevates the larynx and improves UES opening and clearance of food residuals. Postural change “chin down” reduces the distance between the tongue base and pharyngeal dorsal wall, hence narrowing the airway and therefore reducing the risk for leaking (bolus enters prematurely the pharynx) or aspiration within patients known for a delayed swallowing reflex. Moreover, the epiglottic vallecula gets distended, facilitating esophageal bolus passage [9]. The appropriate swallowing maneuvers under endoscopic guidance helped our patient to understand its use and motivated him to be compliant with treatment. The client was counselled about the hazards of substance abuse and silent aspiration. The need to monitor postoperative nutrition with appropriate feeds through Ryle’s tube is not only important but also imperative in improvement of the quality of life. The appropriate head movement was useful in facilitating passage of the food bolus via the healthy pyriform recess and an intensive therapy approach with adequate training and supervision was effective in the acute stage of dysphagia dysfunction. The final result is to have a patient successfully decannulated with ability to consume feeds orally which may take time as in our patient.
Table 1:The Penetration-Aspiration Scale Rosenbek, et al. 1996 [12].
Conclusion
Cut throat injury (CTI) is an emergency that requires a multidisciplinary approach for effective management. It requires the close collaboration of the Otolaryngologist, anaesthesiologist and psychiatrist. The aim of the treatment is not only to save a life but restore airway, voice and swallowing successfully. Patients with cut-throat injuries need psychological support to overcome the trauma to their psyche, which may linger long after the neck wounds have healed. Dysphagia with or without aspiration in patients with CTI requires high index of suspicion with systematic screening protocols so that appropriate measures may be instituted timely for improved quality of life. The airway, swallowing and phonation of patents following CTI must be restored for successful final outcome.
Consent
The patient provided consent held in the electronic medical record. Approval of IRC & IEC obtained: IRC/2023/Protocol/204 dated 15/07/2023 & IEC No GMC/KKD/RP 2023/ IEC/285 dated 15/09/2023.
Acknowledgement
None.
Conflicts of Interest
The authors declare that there is no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- Beigh Z, Ahmad R (2014) Management of cut-throat injuries. Egypt J Otolaryngol 30: 268-271
- R Radhakrishnan, C Andrade (2012) Suicide: An Indian perspective. Indian J Psychiatry 54(4): 304-319.
- Gururaj, MK Isaac (2001) Epidemiology of suicides in Bangalore, National Institute of Mental Health and Neuro Sciences, Bangalore.
- Acharya S, Dash R, Das A (2022) An Epidemiological Study of Cut Throat Injury During COVID-19 Pandemic in a Tertiary Care Centre. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2): 2764–2769.
- Darlong lM, Shunyu NB, Das R (2009) Cut throat zone ii neck injury and advantage of a feeding jejunostomy. J Emerg Trauma Shock 2(3): 213-215.
- Naqvi Sayyed EH, Sadik A, Beg MH, Azam H, Nadeem R, et al. (2017) Successful management of suicidal cut throat injury with internal jugular, tracheal and esophageal transection: A case report. Trauma Case Rep 13: 30-34.
- Fukube S, Hayashi T, Ishida Y, Kamon H, Kawaguchi M, Kimura A, et al. (2008) Retrospective study on suicidal cases by sharp force injuries. J Forensic Leg Med 15: 163-167.
- Shama K, Kakati K, Goswami SC, Bhagawati D, Krishnatreya M (2013) A study on behaviour and management of suicidal cut throat patients. J Laryngol Voice 3: 57-60.
- Zuercher P, Moret CS, Dziewas R (2019) Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Crit Care 23: 103.
- Suman S Penwal (2021) “Swallowing Management in Self-Inflicted Cutthroat Injury and Longstanding Substance Abuse: A Case Study". Acta Scientific Otolaryngology 11-14.
- Rassameehiran S, Klomjit S, Mankongpaisarnrung C, Rakvit A (2015) Post extubation dysphagia. Proc (Bayl Univ Med Cent) 28(1): 18-20.
- Daniels SK, Schroeder MF, DeGeorge PC, Corey DM, Rosenbek JC (2007) Effects of verbal cue on bolus flow during swallowing. Am J Speech Lang Pathol 16(2): 140-147.
-
Akhila Albert, Nambiar Sapna S*, Susmitha VP and Nigil Sreedharan. Management of Suicidal Cut Throat Injury: Lessons Learnt. On J Otolaryngol & Rhinol. 6(4): 2023. OJOR.MS.ID.000642.
-
Throat injury, Emergency tracheostomy, Neck, Laryngeal nerve, General anaesthesia, Laryngeal mucosa, Swallowing saliva, Mental illness, Throat, Dysphagia.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






