 Research Article
Research Article
Evolution of Joint Pain in Patients Treated with Discopexy: Retrospective Study of a Series of Cases
Killian Evandro Cristoff1*, Alice Helena de Lima Santos Cardoso2, Marina Pereira Silva3, Wagner Humming4, Flávio Magno Gonçalves5, Rosane Sampaio Santos6, Thiago Lobianco Viana7 and José Stechman Neto8
1Professor at Universidade Tuiuti do Paraná, Head of the Maxillofacial Service at Hospital do Pilar, Curitiba/PR, Brazil
2Faculty of Dentistry of Ribeirão Preto, University of São Paulo, Department of Basic and Oral Biology-Ribeirão Preto-SP, Brazil
3Undergraduate student at the Tuiuti University of Paraná, Dentistry College, Curitiba/PR, Brazil
4Msc, Dr. INC/PR, Brazil
5Msc, UTP, Curitiba/PR, Brazil
6Adjunct Professor Master’s Program in Communication Disorders-Universidade Tuiuti do Paraná, Brazil
7Coordinator of the Medicine Course at Rondônia Faculty of Education and Culture-UNESC, Brazil
8Teacher at Tuiuti University of Paraná, Curitiba/PR, Brazil
Killian Evandro Cristoff, Professor at Universidade Tuiuti do Paraná, Head of the Maxillofacial Service at Hospital do Pilar, Curitiba/PR, Brazil
Received Date: September 01, 2021; Published Date: September 17, 2021
Abstract
Dysopexy is a surgical method for repositioning the articular disc. The main objectives of articular disc repositioning surgery are to relieve symptoms, long-term stability and maintain disc position.
Objective: The objective of this study is to perform a retrospective analysis of a series of cases, in a group of patients diagnosed with Temporomandibular Disorder (TMD) of joint origin, with surgical indication and understand the response of the surgical treatment of the anchoring of the disc.
Methods: This was a retrospective study of a series of cases, the sample consisted of 34 patients, from individuals aged 23 to 67 years old, 31 women and 3 men diagnosed with exclusively joint pain and limited mouth opening. These patients were examined and treated between 2014 and 2018.
Results: For the analyzed parameters related to pre and post-surgical pain improvement, there were statistically significant differences (p <0.05) in relation to the assessment of pain improvement before and after surgery. Regarding the mouth opening limitation before and after surgical treatment, it was possible to observe an increase in mouth opening in the two-year postoperative period, obtaining a statistically significant difference (p <0.05).
Conclusion: Surgically treated patients could see good results in the short and medium term. Therefore, we can conclude that the operative technique is safe and effective, when correctly indicated.
Keywords: Discopexy; Disc anchoring; Repositioning of the articular disc; Joint dysfunctions
Introduction
The main objectives of discopexy are to promote stability and maintain the position of the articular disc, restore jaw movements, relief pain and improve the patient’s quality of life [1, 2]. The surgical technique consists of a perforation in the posterolateral portion of the mandible head, attaching to it an anchor or resorbable screw, which will serve as a support for the fixation of the disc to it, restoring the normal physiological and anatomical relationship between the disc and the condyle [3, 4]. Discopexy has its indication mainly for cases of displacement of the articular disc without reduction, this is a clinical condition in which the disc is displaced anteriorly in relation to the condyle, promoting reduced condylar movement [5]. Anterior disc displacement is one of the most common pathologies found in patients with temporomandibular disorder (TMD) [5-8].
The classification of the anterior displacement of the articular disc can be with or without reduction. In cases of displacement with reduction, the mouth opening is within the normal range, in which case the patient can or can’t have painful symptoms. As the evolution of the displacement of the disc with reduction, displacement without reduction occurs, in this case, during the translation of the condyle, the disc is forced to an anteromedial position, compressing the retrodiscal tissues, which can generate pain, therefore, functional limitation occurs, from difficulty in mouth opening and/or a deflection of the mandible to the ipsilateral side [4].
The primary treatment of TMD consists of conservative, less invasive techniques. Such as medication, physiotherapy, intraoral devices (DIO), manipulation and intra-articular injections (hyaluronic acid prolotherapy, corticosteroids or saline irrigation). Surgical treatment is indicated in cases where conservative treatments have not abstained from the symptoms of the patient with joint TMD [1, 5]. The objective of this study is to perform a retrospective analysis of a series of cases, in a group of patients diagnosed with Temporomandibular Disorder (TMD) of joint origin, with surgical indication and to understand the response of the surgical treatment of the anchoring of the disc.
Materials and Methods
It is a retrospective study of a series of cases, constituted the sample of this study, 34 individuals, of both sexes. For the composition of the sample for this study was conducted monitoring of patients who underwent the treatment of joint pain in the period 2014 to 2018. The individuals were attended by the Temporomandibular Joint Diagnosis and Treatment Center (CDATM) of the Tuiuti University of Paraná, and diagnosed with unimpaired disc displacement, presenting joint pain unresponsive to conservative clinical treatment. This study was approved by opinion 2432451 of the Research Ethics Committee of the Tuiuti University of Paraná, Curitiba-PR, protocol CAAE 77215717.7.0000.8040. The patients were informed and agreed to participate in this research with the acceptance of the free and informed consent term. The information collected was guaranteed the secrecy that ensures the privacy and anonymity of the subjects regarding the confidential data involved in the research.
The individuals were examined according to the protocols established in the criteria according to the questionnaire Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). All patients underwent conservative treatment first, these patients remained in clinical treatment for approximately one year, with persistent symptoms. Thus, all patients underwent arthrocentesis, but there was still persistent pain, so it was decided to perform surgical discopexy in the open field. All patients had surgical indication. The patient’s symptomatology was assessed according to the visual analog scale (VAS), which ranges from a degree of pain from 0 to 10, with 0 meaning that the patient has no pain, and 10 being the maximum pain level by the patient. The surgeries were performed at Nossa Senhora do Pilar Hospital- Curitiba, PR, Brazil through the Buco-maxillofacial Surgery and Traumatology Service, under the management of Dr. Killian Evandro Cristoff. All patients underwent postoperative physiotherapy not happening no serious complications.
Inclusion criteria for surgical treatment were:
1. Patients who had unilateral or bilateral internal disorder, diagnosed with disc displacement without reduction and exclusively articular pain, according to the questionnaire Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) and Nuclear magnetic resonance (RNM);
2. Persistent pain to conservative treatments;
3. Limitation of mandibular movement, persistent pain
when treated with arthrocentesis;
4. Disc displacement based on magnetic resonance and clinical examination;
5. No previous TMD surgery;
6. Subject to replacement articular disc.
The exclusion criteria for surgical treatment were:
1. Patients with muscle pain according to RDC/TMD;
2. Patients who responded positively to conservative clinical treatment or arthrocentesis with viscosupplementation;
3. Patients with degenerative/autoimmune disease.
Initially, statistical data were described considering the mean, standard deviation, minimum, maximum and quartiles for quantitative variables and frequency tables for qualitative variables. Graphical analyzes were made to facilitate the interpretation of descriptive results. The variables VAS after clinical treatment and VAS after surgical treatment, over time, were compared using Friedman’s nonparametric test. The Wilcoxon nonparametric test, with Bonferroni correction, was used to compare pairs of Friedman’s analysis. The parametric ANOVA test was used to verify the effect of treatment on mouth opening at different times of the study (pre-treatment, post-treatment, 3 months, 6 months, 1 year and 2 years). The comparison of the pairs was performed by the tests Paired T-Student, with Bonferroni correction. The normality of the variables was assessed using the Shapiro Wilks test. All tests were evaluated considering the significance level of 5%; except for those performed with Bonferroni correction. The Bonferroni test aims to adjust the significance value of the test based on the number of comparisons (m) to decrease the chance of type I error.
Results
The study sample consisted of 34 patients, 31 of whom were female (91.2%) and three were male (8.8%), ranging from 23 to 67 years old. All patients had been submitted to conservative treatment first, the 34 studied patients used the intraoral device (DIO), 13 patients (38.2%) underwent psychological treatment with a qualified professional and the same 13 patients (38.2%) underwent treatment with a speech therapist with orofacial motricity with a qualified professional; 26 patients (76.5%) underwent drugs, including corticosteroids, aines, opioids, antidepressants, anxiolytics, anticonvulsants. We can see in Table 1, the relationship of the categorical variable between patients’ gender and conservative treatments (Table 1).
According to the visual analog scale (VAS), joint pain after clinical treatment ranged from 2 to 8, with an average of pain 4,38. These patients remained in clinical treatment for one year, with persistent symptoms. Thus, all patients underwent arthrocentesis, but there was no significant improvement, with persistent pain after clinical treatment, so it was decided to perform surgical discopexy in the open field.
There was a statistically significant improvement (p <0.05) in relation to joint pain after clinical treatment compared to after surgical treatment (Table 2). After two years 32 patients reported pain 0, but two patients were symptomatic, within one year of the postoperative period, they had pain according to the VAS 6 and 7 pain scale (Table 2).
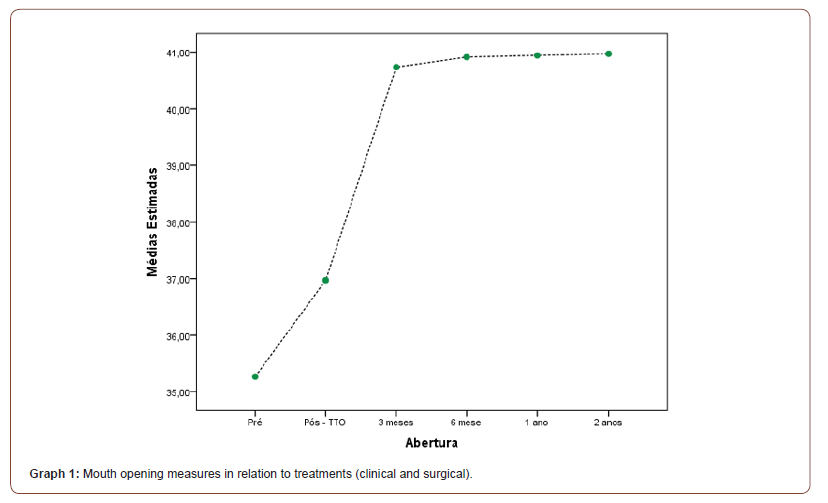
With regard to mouth opening, we can see in Table 3, there was a statistically significant difference (p <0.05) in relation to mouth opening after clinical treatment, with mouth opening in relation to post-surgery (3, 6 months, 1 and 2 years) (Table 3).
Table 1: Relationship between categorical variables.
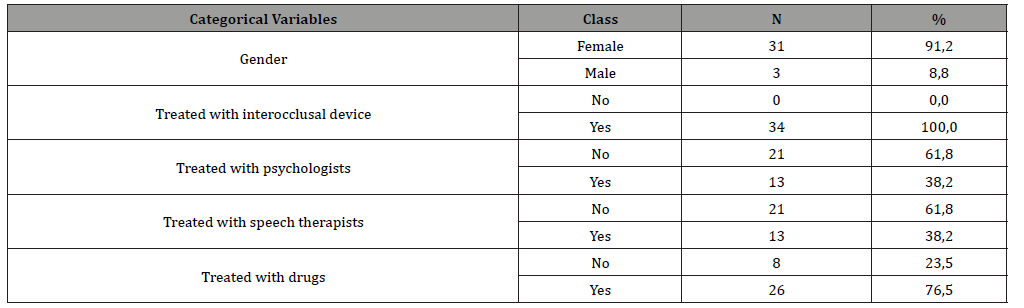
Table 2: Comparison of joint pain according to VAS after clinical treatment and after surgical treatment.

Table 3: Comparison of mouth opening after clinical treatment with postoperative.

Still, in Graph 1 we can observe the mouth opening measures before clinical treatment (pre), after clinical treatment (Post-TTO) and 3, 6 months, 1 and 2 years after surgery (3 months, 6 months, 1 year and 2 years) in which it is observed that after clinical treatment there was a slight increase in mouth opening, but the patient remained symptomatic and opted to undergo discopexy, after surgery, monitoring showed us a significant increase in mouth opening, as shown in the graph below (Graph 1).
Discussion
Dysopexy is promising in restoring the physiological and anatomical relationship of the disc and condyle, in ATMs with internal disorders and allowing a good functional movement of the jaw, eliminating the symptoms and restoring the patient’s quality of life [6, 9]. The treatment of ATM dysfunction is widely discussed in the literature, with good results reported for open surgery techniques [6, 8, 10, 11]. However, this type of treatment isn’t consensual, with many discussions [12]. According to some authors, the goals for using the open surgical technique can be achieved by trying to restore the position of the physiological disk, while others believe that the repositioning of the disk isn’t so important, as our organism has the ability to adapt the system stomatognathic [13].
The indication for surgical treatment is irreversible damage to the ATM, in which the clinical method wasn’t successful [6,10,12,14]. Open ATM surgery can offer excellent results in patients with disc displacement without reduction, subject to replacement, that is, without perforations and large adhesions. Unfortunately, the success rate decreases as the disease becomes more serious [15]. Therefore, early identification of disc displacement and immediate surgical repositioning can stop the progression of osteoarthritis and disc degeneration, as long as there aren’t other predisposing factors, such as connective tissue or autoimmune diseases or infectious agents that affect the joints [2, 3].
The findings of our study coincide with those reported by others in terms of gender. In the present study, of the 34 patients, 91.2% were female and 8.8% male, with a higher incidence in women, which is observed in other studies such as Capan, et al. [1], in which 96.8% of the patients were female. This predilection for the female sex is also found in the study by Spallaccia, et al. [6], in which there were 30 patients in which 29 were female and one male.
Regarding the improvement of joint pain, Mehra e Wolford [2], obtained results in which there was a significant difference in relation to the preoperative and postoperative VAS (p <0.05) and complete absence of ATM pain in the postoperative period of one year. Which corresponds to our study, in which we can observe that there was a significant difference comparing the VAS after clinical treatment and VAS after two years postoperatively. We can see that after 15 days postoperatively the patient has already reported an improvement in joint pain. After two years, the mean pain of the 34 patients ranged from 0,47. Of the 34 patients, 32 are asymptomatic according to VAS the patient had pain 0, but three patients are still symptomatic, presenting joint pain, according to VAS 6 and 7, these two patients in the clinical post-treatment and surgical pre treatment had a joint pain, according to VAS 8 and 9, respectively, with a slight improvement in joint pain.
All patients remain in follow-up and continue to use the DIO, and the two symptomatic patients are still undergoing physical therapy, psychological and pharmacological treatment, in addition to using the DIO.
In the study by Spallaccia, et al. [6], in a reference according to the visual analog scale (VAS) from 0 to 10, there was an average of the preoperative TMJ pain value score, which was 7,3 and the average postoperative joint pain score 1,8. In which coincides with the findings of our study, according to the visual analogue scale (VAS) from 0 to 10, the VAS of joint pain before clinical treatment was 6,94, after clinical treatment the average pain according to the VAS was 4,38, after the seven day surgical treatment, we obtained a VAS of 2,38, remembering that there could still be pain due to the recent surgery, but after two years postoperatively, the mean VAS was 0,47.
On the other hand, the randomized clinical trial carried out by Schiffman, et al. [16], in which they compared therapy with an interocclusal device with other treatment options, including conservative and surgical approaches, and concluded that all of them are efficient in the treatment of intra-articular ATM disorders.
Regarding the mouth opening, Spallaccia, et al. [6], in their study, they obtained a mean mouth opening before surgery of 31.73mm and the mean value after surgery was 38,73mm, showing a statistically significant difference (p<0,05). In our study, we obtained similar results, statistically significant (p <0.05), in which the mean mouth opening after clinical treatment was 36,97mm, and after the surgical treatment we obtained a mouth opening of 40,97mm, thus returning an improvement in the patient’s quality of life.
Mehra e Wolford2, studied 105 patients (89 women and 16 men) underwent joint disc repositioning, and concluded that only two patients, after surgical treatment, had a jaw opening 35mm. However, in all patients, ATM pain or interincisary opening improved after surgery. Corroborating with our results. Although conservative and minimally invasive treatments offer symptomatic relief in many patients, disease progression remains unchanged, that is, not necessarily conservative treatment improves the position and deformity of the disc [7,10, 14, 17]. Disc repositioning surgery can mitigate degeneration caused by internal disorders, eliminating mechanical interference and facilitating the movement of coordinated joints, in addition to improving pain [6, 7, 9].
Conclusion
Surgically treated patients were able to see good results in the short and medium term. Therefore, we can conclude that the operative technique is safe and effective, when correctly indicated, and preceded by conservative clinical treatment, respecting the treatment hierarchy. Decreasing the patient’s pain, increasing the patient’s mandibular kinematics and returning, significantly, an improvement in the function of the stomatognathic system and quality of life for patients with joint TMD.
Acknowledgement
None.
Conflict of Interest
No conflicts of interest.
References
- Capan N, Esmaeilzadeh S, Karan A, Dirakoglu D, Emekli U, et al. (2017) Effect of an early supervised rehabilitation programme compared with home-based exercise after temporomandibular joint condylar discopexy: a randomized controlled trial. Int J Oral Maxillofac Surg 46(3): 314-321.
- Mehra P, Wolford LM (2021) The mitek mini anchor for TMJ disc repositioning: surgical technique and results. Int J Oral Maxillofac Surg 30(6): 497-503.
- Mehra P, Wolford LM (2021) Use of the mitek anchor in temporomandibular joint disc-repositioning surgery. Proc (Bayl Univ Med Cent) 14(1): 22-26.
- Manganello LCS, Silveira ME, Silva AAF (2014) Cirurgia da articulação temporomandibular. São Paulo: Santos, Brazil, p: 2-4.
- McCain JP, Hossameldin RH, Srouji S, Maher A (2015) Arthroscopic discopexy is effective in managing temporomandibular joint internal derangement in patients with Wilkes stage II and III. J Oral Maxillofac Surg 73(3): 391-401.
- Spallaccia F, Rivaroli A, Basile E, Cascone P (2013) Disk repositioning surgery of the temporomandibular joint with bioabsorbable anchor. J Craniofac Surg 24(5): 1792-1795.
- Rajkumar K, Mukhopadhyay P, Sinha R (2016) Temporomandibular joint disc repositioning using an orthopedic suture anchor: a modified disc anchoring technique. J Maxillofac Oral Surg 15(3): 404-407.
- Gonçalves JR, Cassano DS, Rezende L, Wolford LM (2015) Disc repositioning: does it really work? Oral Maxillofac Surg Clin North Am 27(1): 85-107.
- Stephen E, Smilack MS (1987) Technique of functional disc depositioning in Internal derangements of the temporomandibular joint. J Oral Maxillofac Surg 45: 825-827.
- Ohnuki T, Fukuda M, Nakata A, Nagai H, Takahashi T, et al. (2006) Evaluation of the position, mobility, and morphology of the disc by MRI before and after four different treatments for temporomandibular joint disorders. Dentomaxillofac Radiol 35(2): 103-109.
- Undt G, Murakami KI, Rasse M, Ewers R (2006) Open versus arthroscopic surgery for internal derangement of the temporomandibular joint: a retrospective study comparing two centres’ results using the Jaw Pain and Function Questionnaire. J Craniomaxillofac Surg 34(4): 234-241.
- Potier J, Maes JM, Nicot R, Dumousseau T, Cotelle M, et al. (2016) Chirurgie discale de l’articulation temporo-mandibulaire Temporomandibular joint disc surgery. Revue de Stomatologie, de Chirurgie Maxillo-faciale et de Chirurgie Orale 117(4): 280-284.
- Greene CS, Obrez A (2015) Treating temporomandibular disorders with permanent mandibular repositioning: is it medically necessary? Oral Surg Oral Med Oral Pathol Oral Radiol 119(5): 489-498.
- Hosgor H, Bas B, Celenk C (2017) A comparison of the outcomes of four minimally invasive treatment methods for anterior disc displacement of the temporomandibular joint. Int J Oral Maxillofac Surg 46(11): 1403-1410.
- Tzanidakis K, Sidebottom AJ (2013) Outcomes of open temporomandibular joint surgery following failure to improve after arthroscopy: is there an algorithm for success. Br J Oral Maxillofac Surg 51(8): 818-821.
- Schiffman EL, Velly AM, Look JO, Hodges JS, Swift JQ, et al. (2014) Effects of four treatment strategies for temporomandibular joint closed lock. Int J Oral Maxillofac Surg 43(2): 217-226.
- Foletti JM, Cheynet F, Graillon N, Guyot L, Chossegros C (2016) Arthroscopie de l’articulation temporo-mandibulaire. mise au point TMJ arthroscopy a review. Rev Stomatol Chir Maxillofac Chir Orale 117(4): 273-279.
-
Killian Evandro Cristoff, Alice Helena de Lima Santos Cardoso, Marina Pereira Silva, Wagner Humming, Flávio Magno Gonçalves, Rosane Sampaio Santos, Thiago Lobianco Viana and José Stechman Neto. Evolution of Joint Pain in Patients Treated with Discopexy: Retrospective Study of a Series of Cases. On J Otolaryngol & Rhinol. 5(1): 2021. OJOR.MS.ID.000604.
-
Temporomandibular disorder, Head, Autoimmune disease, Internal disorders, Retrodiscal tissues, Physiotherapy, Traumatology service, TMD surgery, Osteoarthritis, ATM surgery.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






