 Mini Review
Mini Review
Ear, Nose and Throat Approach in Autoimmune Blistering Diseases
Ismail Cem Temel1, Asli Bilgic-Temel2* and Dedee Frances Murrell2,3
1Sydney ENT Clinic, Sydney, Australia
2Department of Dermatology, St George Hospital, UNSW, Australia
3Faculty of Medicine, University of New South Wales, Australia
Asli Bilgic-Temel Department of Dermatology, St George Hospital, UNSW, Australia.
Received Date: October 08, 2018; Published Date: October 30, 2018
Abstract
Autoimmune blistering diseases (AIBD) are a group of rare blistering disorders of the skin and mucous membranes due to autoantibodies directed against specific proteins. Involvement of mucosal areas in AIBD significantly increases patient morbidity and mortality. Ear, nose and throat (ENT) examination should be a routine procedure to evaluate mucosal involvement in every AIBD. Patients should be asked whether they had oropharyngeal, ear, nose and throat symptoms and all patients should be evaluated for ENT manifestations by direct and endoscopic examination even in patients without symptoms.
Keywords: Autoimmune blistering diseases; Ear; Nose; Throat; Mucosal involvement
Abbreviations: AIBD: Autoimmune Blistering Diseases; IEBD: Intraepidermal Blistering Diseases; SEBD: Subepidermal Blistering Diseases; PV: Pemphigus Vulgaris; PF: Pemphigus Foliaceus; PNP: Paraneoplastic Pemphigus; BP: Bullous Pemphigoid; MMP: Mucous Membrane Pemphigoid; ENT: Ear, Nose and Throat; PDAI:Pemphigus Disease Area Index; ABSIS: Autoimmune Bullous Skin Disorder Intensity Score; DIF: Direct Immunofluorescence Microscopy; ELISA: Enzyme-linked Immunosorbent Assay
Introduction
Autoimmune blistering diseases (AIBD) are a group of rare blistering disorders of the skin and mucous membranes due to autoantibodies directed against specific proteins. However, they cause significant morbidity and mortality. AIBD could be divided into 2 subgroups: 1. Intraepidermal blistering diseases (IEBD), 2. Subepidermal blistering diseases (SEBD) [1].
IEBD encompasses pemphigus vulgaris (PV), pemphigus foliaceus (PF) and paraneoplastic pemphigus (PNP) as the main subtypes. PV is the major type and it is most commonly seen between the ages of 40 and 50 years. It usually starts as erosions in the oral mucosa, and then continues with blistering and erosive skin lesions. Other commonly involved areas include the pharynx, larynx, nasal mucosa and oesophagus. Its incidence is estimated to be two new patients per 1 million inhabitants per year in Central and Western Europe. However, it is more commonly seen in Mediterranean and Middle Eastern countries. PNP is a paraneoplastic blistering disease characterized by cheilitis and/or ulcerative stomatitis, persisting painful erosions of mucosa and cutaneous polymorphic involvement (graft-versus-host disease-like, erythema multiformelike, bullous pemphigoid- like or pemphigus vulgaris-like eruption). It usually presents with severe mucosal involvement including the pharyngeal, laryngeal, ocular and genital mucosal surfaces. Its prognosis is poor because of concomitant malignancy. On the other hand, PF does not affect the mucosal surfaces [2].
Bullous pemphigoid is the main AIBD of the subepidermal blistering group. It is the most common AIBD in developed countries and typically seen in people over 70 years old. Although it might affect mucosal areas, it is not as common as seen with PV [3]. On the other hand, mucous membrane pemphigoid (MMP) mainly affects the mucosal surfaces of oropharynx, larynx, nose, eyes, oesophagus and genitals. It usually results in tissue destruction (airway loss, blindness, etc.) and functional limitations (malnutrition, loss of teeth, etc.) because of chronic mucosal inflammation and scarring [4].
We aimed to summarise general recommendations and approaches to ENT examination and procedures in AIBD.
Ear, nose and throat involvement
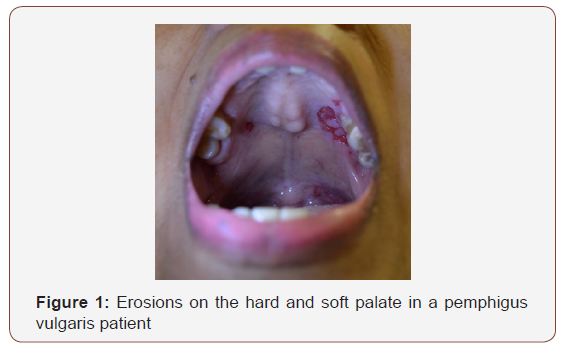
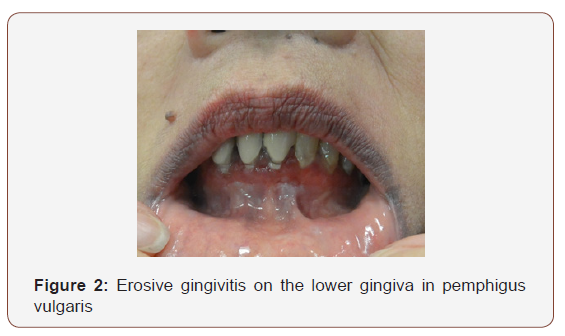
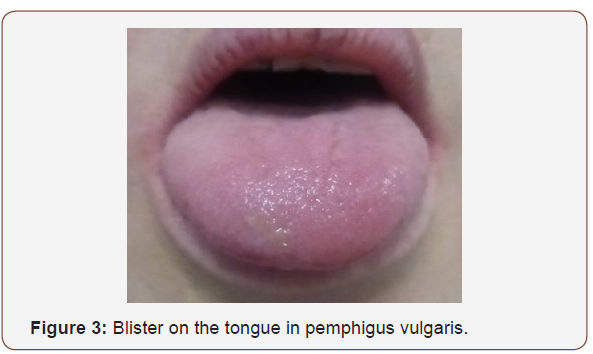
Involvement of mucosal areas in AIBD significantly increases patient morbidity and mortality. PV in the IEBD group and MMP in the SEBD are the most prominent and common ones affecting the mucosal surfaces (Figure 1-3). However, others might also cause mucosal lesions. Ear, nose and throat (ENT) examination should be a routine procedure to evaluate mucosal involvement in every AIBD. Patients should be asked whether they have oropharyngeal, ear, nose and throat symptoms and all patients should also be evaluated for ENT manifestations by direct and endoscopic examination, even if they do not have any symptoms [5].
The frequency of ENT involvement was studied and found to be more frequent than expected, especially in PV, by several groups [5-11]. Our recent study involving 50 patients with PV additionally suggested that the severity of ENT involvement in PV was significantly associated with ENT symptoms and endoscopic findings, especially in cases of severe disease (Pemphigus Disease Area Index (PDAI) ≥15 and/or Autoimmune Bullous Skin Disorder Intensity Score (ABSIS)≥17] [5]. However, apart from severe and scarring forms of AIBD, even mild mucosal involvement can cause discomfort, bleeding and erosions on the mucosae.
Thus, ENT surgeons should apply a specific examination and procedural approach in the care of these patients.
Procedural approach
Patients with AIBD are ideally followed in specific clinics where a multidisciplinary approach is available. However, patients with AIBD are often first seen by an ENT specialist in a local hospital. Thus, every ENT surgeon should be aware of the essential steps in the diagnosis and management of such patients.
Diagnosis
Biopsy
Clinical features, compatible light microscopy findings and positive direct immunofluorescence microscopy (DIF) findings and/ or positive specific Enzyme-linked Immunosorbent Assay (ELISA) autoantibodies are necessary for the diagnosis of AIBD [2-3]. Specimens for light microscopy studies should be taken from early bullae arising (from the edge of the lesion, including the lesional mucosa and the normal mucosa around it) on erythematous/ normal mucosa or skin and placed in formalin solution with care not to leave the epidermis from the dermis [12].
The most critical test in the diagnosis of AIBD is DIF. Its positivity is essential for the diagnosis of AIBD according to wellestablished guidelines [2,3]. The biopsy specimen for DIF should be obtained from perilesional mucosa (avoid the blistered mucosa or erosion), and for transportation, skin biopsy specimens for DIF studies should be put into Michel’s fixative or simply 0.9% NaCl solution [2,13].
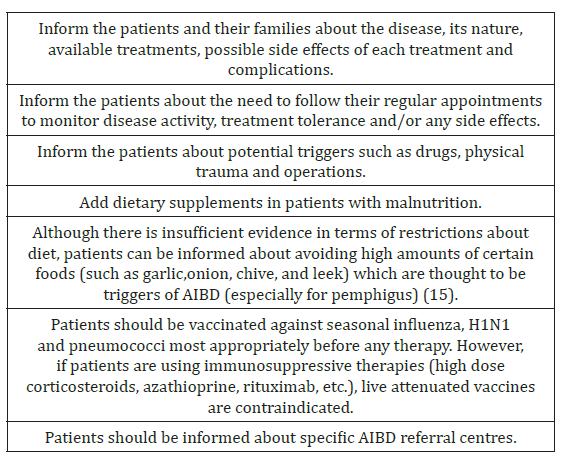
General recommendations
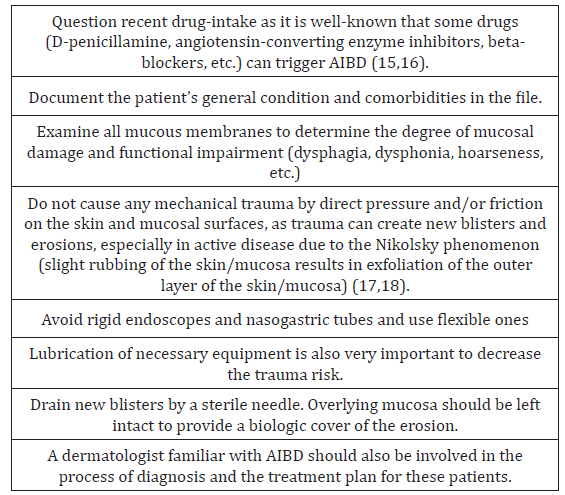
There are some recommendations suggested in the management of patients with AIBD, established in the guidelines and in expert opinions [2,3,14,15] (Table 1).
Table 1: summarises these recommendations.
ENT examination and clinical approach
There are certain steps that can be taken by practitioners to optimise the ENT examination. These steps are summarised in [2,3,14-18] (Table 2).
Table 2: Recommendations for ENT examination and clinical approach.
During ENT operations
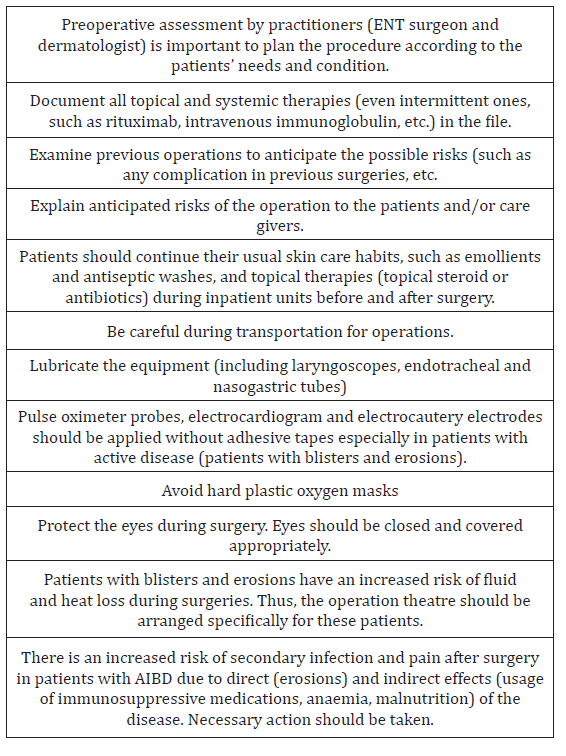
Moreover, there are important points to consider before, during and after the ENT operations. These bullet points are lined up in [2,3,14] (Table 3).
Table 3: Recommendations for ENT operations.
Monitoring the disease
Patients should be monitored in specialised AIBD centres according to several measures such as clinical condition, the severity and disease progress during treatment and the therapeutic choice (monitoring, tolerance, adverse-effects) [2,3].
Conclusion
Every ENT specialist should be aware of AIBD as they can be the first practitioner evaluating these patients. Thus, awareness can provide early diagnosis which results in better control of the disease and reduces morbidity and mortality. Skin and mucous membrane fragility of these patients need a safe and effective procedural approach during ENT mucosal examination and/or procedures.
Acknowledgements
Dr. Ismail Cem Temel is a consultant ENT surgeon at Seydisehir State Hospital, Konya, Turkey. He is currently working as an Observer at Sydney ENT Clinic, Sydney, Australia.
Dr. Asli Bilgic-Temel is a consultant Dermatologist and now working as a Visiting Dermatology Fellow at St. George Hospital, UNSW, Sydney, Australia. She is the recipient of the Turkish Dermatology Society – Prof. Dr. Hulusi Behcet (Long-term Research) Scholarship in 2018.
Conflict of Interest
None.
References
- Schmidt E, Borradori L, Joly P (2015) Epidemiology of Autoimmune Bullous Diseases. Blistering Diseases: Clinical Features, Pathogenesis, Treatment. Dédée F (Ed.), Murrell First Edition. Springer-Verlag Berlin Heidelberg, Netherlands, pp. 251-263.
- Hertl M, Jedlickova H, Karpati S, Marinovic B, Uzun S, et al. (2015) Pemphigus. S2 Guideline for diagnosis and treatment--guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV). J Eur Acad Dermatol Venereol 29(3): 405-414.
- Feliciani C, Joly P, Jonkman MF, Zambruno G, Zillikens D, et al. (2015) Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol 172(4): 867-877.
- Amber KT, Murrell DF, Schmidt E, Joly P, Borradori L. (2018) Autoimmune Subepidermal Bullous Diseases of the Skin and Mucosae: Clinical Features, Diagnosis, and Management. Clin Rev Allergy Immunol 54(1): 26-51.
- Bilgiç Temel A, Temel I.C, Bostancı Toptaş A, Turhan M, Bozkurt S, et al. (2016) The effect of endoscopic ear, nose and throat examination on pemphigus severity scoring systems (poster presentation). Pathogenesis of Pemphigus and Pemphigoid, Munich, Germany.
- Fawzy MM, Hegazy RA, Abdel Fattah AF. (2013) Ear, nose, and throat involvement in Egyptian patients with pemphigus vulgaris: a step towards a better management. Int J Dermatol 52 (10): 1268-1273.
- Robati RM, Rahmati-Roodsari M, Dabir-Moghaddam P, Farnaghi A, Mahboobi-rad F, et al. (2012) Mucosal manifestations of pemphigus vulgaris in ear, nose, and throat; before and after treatment. J Am Acad Dermatol 67 (6): 249-252.
- Fernández S, España A, Navedo M, Barona L (2012) Study of oral, ear, nose and throat involvement in pemphigus vulgaris by endoscopic examination. Br J Dermatol. 167: 1011-1016.
- Kavala M, Altıntaş S, Kocatürk E, Zindancı I, Can B, et al. (2011) Ear, nose and throat involvement in patients with pemphigus vulgaris: correlation with severity, phenotype and disease activity. J Eur Acad Dermatol Venereol. 25 (11): 1324-1327.
- España A, Fernández S, del Olmo J, Marquina M, Pretel M, et al. (2007) Ear, nose and throat manifestations in pemphigus vulgaris. Br J Dermatol156 (4): 733-737.
- Hale EK, Bystryn JC. (2001) Laryngeal and nasal involvement in pemphigus vulgaris. J Am Acad Dermatol 44 (4): 609-611
- Erkin G (2011) The Histopathological Diagnosis of Autoimmune Bullous Diseases. Turkderm. 45 Suppl 1: 26-30.
- Uzun S (2011) Immunofluoresecence Findings in the Diagnosis of Autoimmune Bullous Diseases. Turkderm. 45 Suppl 1: 31-5.
- Uzun S (2012) Current Management of Pemphigus. Turk J Dermatol 6: 91-101.
- Tavakolpour S (2018 ) Pemphigus trigger factors: special focus on pemphigus vulgaris and pemphigus foliaceus. Arch Dermatol Res 310(2): 95-106.
- Stavropoulos PG, Soura E, Antoniou C (2014) Drug-induced pemphigoid: a review of the literature. J Eur Acad Dermatol Venereol 28(9): 1133- 1140.
- Urbano FL. (2001) Nikolsky’s sign in autoimmune skin disorders. Hosp Physician 37: 23-4.
- Uzun S, Durdu M (2006) The specificity and sensitivity of Nikolskiy sign in the diagnosis of pemphigus. J Am Acad Dermatol 54(3): 411-415.
-
Ismail Cem Temel, Asli Bilgic-Temel, Dedee Frances Murrell. Ear, Nose and Throat Approach in Autoimmune Blistering Diseases. On J Otolaryngol & Rhinol. 1(1): 2018. OJOR.MS.ID.000504.
-
Autoimmune blistering diseases (AIBD) are a group of rare blistering disorders of the skin and mucous membranes due to autoantibodies directed against specific proteins. Involvement of mucosal areas in AIBD significantly increases patient morbidity and mortality. Ear, nose and throat (ENT) examination should be a routine procedure to evaluate mucosal involvement in every AIBD.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






