 Review Article
Review Article
Complications in Blepharoplasty and How to Resolve Them
Marcos Antonio Rodriguez Perales* and Francisco Javier Saynes Marin
1MD, ENT HNS, Hospital Español de México Mexico City, Mexico
2Hospital Angeles Metropolitano, Mexico City, Mexico
Marcos Antonio Rodriguez Perales, Hospital Español, Av. Ejército Nacional 617 Office 804 Old Consultation Tower “Rosario Guerrero”, Col. Granada. Mayor Miguel Hidalgo 11520, Mexico City Mexico, Mexico.
Received Date: March 19, 2021; Published Date: May 24, 2021
Abstract
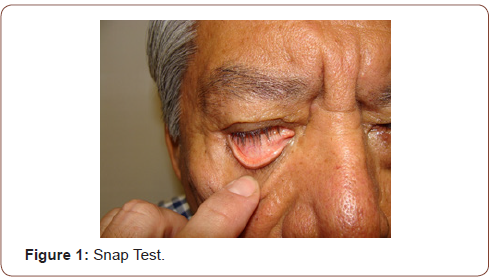
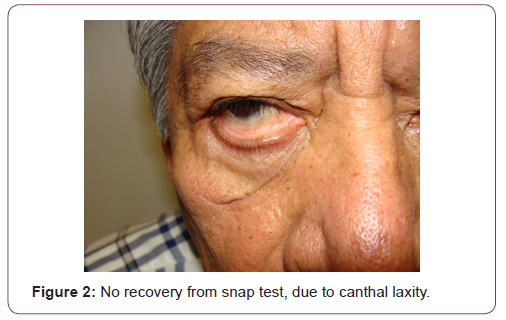
Any type of eyelid correction or postoperative blepharoplasty complication should be well managed and studied before attempting its correction, as it could lead to a worsening of the original alteration. Although postoperative scars in a blepharoplasty are relatively rare, they can generally be improved by massage and late with the application of topical corticosteroids, with the understanding that their best use is during the first twelve months. An early intervention should be avoided as this can worsen the result and rarely improve the final result, when there is a healing problem, remembering that stress is a determining factor in the final result. The laxity of the canthus tendons should always be evaluated either by directly pulling the eyelid down, with an eyelid glide test, the impingement test, and a poor eyelid position prior to surgery should always be documented. In these cases, the surgeon who operates blepharoplasty must have a perfect knowledge of the management of the canthal tendons and have within his surgical resources the realization of the canthal application or the repositioning of the palpebral canthal tendon.
Introduction
Blepharoplasty is the cosmetic surgery of the eyelids, aimed at reducing the apparent age and making them look younger, or is used to change characteristics that the patient does not like about their eyelids. All cosmetic surgeries are on the rise today, and an increasingly requested facial surgery is blepharoplasty. In the courses where aesthetic related topics are taught, cases of spectacular improvement are always seen, especially in the body, however in eyelid surgery complications are frequent and very visible, being a very frequent cause of instaisfaction. We will describe different ways of classifying complications, but we will focus on the severity of these, complications that can range from mild to very serious, we will also mention the problems common to both eyelids, as well as those of the upper and lower eyelids, what better way to do it. learn about these problems to understand the reasons for these complications that often happen inadvertently and many more inadvertently Being aware of these complications will make us better surgeons, especially if we can prevent or solve postoperative problems through the judicious use of medical judgment, since complications are not uncommon. We will not touch on congenital, traumatic, oncological or reconstructive problems, since those are a separate chapter [1-9]. Something that a patient will never forgive is the visible or noticeable asymmetry of their eyelids. We will not be repetitive in this fact. An article does not replace the experience and knowledge that can be obtained in the dissections of the cadavers, but it is a good start to document yourself on the subject. We will try to do a systematic handling of these problems.
Classification
There are many ways to classify complications: The conditions in blepharoplasty can be Anatomical, Functional or Involutive. If we classify the lesions by anatomical site to facilitate understanding and their solution could be simplified as follows:
• Anatomical Site Lack of Resection Excess of Resection
• Skin Bulging and Wrinkles Eyelid Retraction
• Muscle Muscle Bands Open Eye
• Grease Dark Circles Small Eye
• Cantal Ligaments Scleral Show Displaced Eyelid
• Elevator Aponeurosis Ptosis Scared Eye
In the Tarsus position, if we take into account only 2 palpebral sections can occur:
Excess posterior lamina//Excess anterior lamina
Ectropion//Entropion
Injuries from Other Sites
Oculars
Blindness
Corneal injury
Eye perforation
Injury to extraocular muscles, especially the lower oblique
Persistent chemosis
Of the Lagrimal Way
Epiphora
Dry Eye
Of the Skin
Edema
Persistent ecchymosis
Lymphedema
IN cases of unsuccessful external canthal modification any variant can occur from a “sad eye” to a “feline eye”.
If we classify the complications by the time of the procedure, the simplest thing is:
1. -Preoperative
2. -Transoperative
3. -Postoperative
-Preoperative: Most common mistakes
• Not evaluating the ocular function and the characteristics of the tear. (perhaps the most frequent complaint)
• Lack of correct oculopalpebral revision
• Consider any metabolic and healing conditions
• Ocular Malposition, unfavorable plane (“a bulging eye” or with exophthalmos should not be operated without experience)
• Cantal malposition
• Ligamentous Laxity
-Transoperative:
• Tissue Overesection: The tissues should never be thrown away before finishing the surgery, they can be used as free grafts, especially the skin.
• Vascular: Manual compression with gauze or soaked in a vasoconstrictor stops bleeding after several minutes and will allow its control with cautery or radio frequency preferably. Haemostasis must be meticulous at every step and at all times during surgery, bleeding must always be under control.
• Injury of Eye Structures: It is always necessary to have at hand the data of various ocular specialists, who can help us to solve injuries that would otherwise be catastrophic in cosmetic surgery, specialists in cornea, vitreous, strabismus in the case of transconjunctival surgery.
• Difficulty in Identifying the Surgical Planes: A clean and anatomical dissection should always be carried out, since the fineness of the palpebral tissues requires it, this allows us not to get lost in the surgical planes, but when this happens it is important to stop clean, check hemostasis, wash and orient yourself or think about the next step [9-16].
• A useful tip before continuing with the surgical procedure, in the event that it is a secondary blepharoplasty and the planes are not so clear, finding the levator aponeurosis and Whitnall’s ligament will be very useful since the fat will remain on top of these structures.
• Technical Complications: When things are not going well it is important to stop, wash, do hemostasis to try to re-orient oneself and go over the surgical technique mentally again, in the event that things are a bit complete for really one feel it diskin ability technique it is very important to always have someone to talk to so that they can guide you or help you solve the surgery. When things are not going well, it is important to stop, wash, do hemostasis to try to re-orient yourself and mentally review the technique again. Remember that if things are difficult we are not doing them well [16-19].
-Postoperative:
• Dry Eye: A problem This is a frequent problem for which the use of artificial tears every 3 or 4 hours is recommended in the postoperative period or even more frequently if warranted. There are artificial tear ointments.
• Keratitis by Exposure: The ocular opening of no more than 1mm is tolerable, however the use of ointments at night is very important in the first weeks of surgery since having difficulties to fully close the eye, the cornea can be exposed if there is no good bell phenomenon. That is why it is recommended to use a protective ointment at night to sleep [20-27].
• Hypercorrection or Hypocorrection of the Surface Skin: In the case of the excess skin, it is necessary to wait three months before making the decision to remove the excess skin, however sometimes the use of complementary chemical peels helps to retract the skin. In the case of overresection, it is necessary to think about the placement of a full thickness graft to try to solve this problem, this is very important in the case of the lower eyelid where it is evident that lagophthalmos or sclera show after an overresection of the skin, while in the upper eyelid this is less of a problem. One must be very cautious in skin resection when one is inexperienced. In the case of fat, you should always think about transposing or repositioning the fat before drying it.
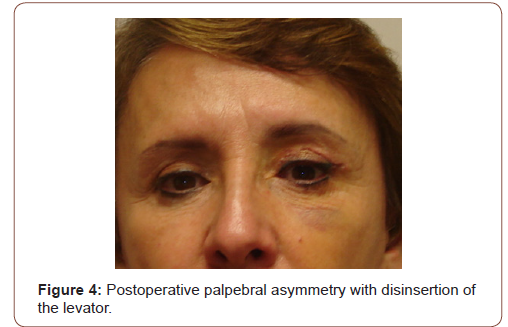
• Antiesthetic Palpebral Groove: either very high or very low, in both situations is unnatural, but the fact that they are asymmetrical is inexcusable by the patient [28-36].
• Preseptal, Orbitary Cellulitis or Infections: These respond very well to antibiotics and are generally caused by streptococcus or staphylococcus, fortunately they respond well to antibiotic management. Immunosuppressed patients may have other types of infections. very serious.
• Incision: Irregularities in granulomas, inclusion cysts and tunnels of epithelial sutures. The keloid scar practically does not exist on the eyelids, although the patient has it on other sides of the body.
• Eyelid Ptosis: Detachment of the upper eyelid.
• Diplopia: Oblique muscle injury.
• Excision of the Lagrimal Gland: Eventually it is confused with the upper external fat pack, which does not exist.
Other conditions that require the support of subspecialists in ophthalmology are:
Ischemia of the Optic Nerve
Eye Balloon Perforation
Occlusion of the Central Artery of the Retina
Finally, we would like to make a classification by the severity of the injury is that it occurs and is the following and we divide them into two types:
1. Major Complications are catastrophic, involving loss of visual acuity and permanent deformities of the eyelid anatomically and functionally
2. Minor Complications include bleeding, wound dehiscence, infection, corneal damage and minor eyelid position, extraocular muscle involvement, conjunctival and lacrimal duct injuries, as well as various inflammatory and scarring conditions [36-38].
Preoperative Assessment
It is important to take a careful medical history to determine the health and risk factors for these patients, we must evaluate the expectation, their aesthetic and functional goals, and what we can offer, as well as listen carefully to the patient, we must never forget to ask about all Previous surgical procedures and their complications, especially ocular, whether or not a trained person intervened, as well as chronic, psychiatric, cardiovascular diseases, brain disease and endocrine system as well as endocrine exophthalmos. The use of medicines, vitamins and other compounds is very important, as is the consumption of cigarettes and alcohol. The detailed physical examination will help us to determine the state of health of the tissues, consistency and elasticity, areas of fibrosis and inflammation. It is essential in the repair of complications NOT to perform a correction surgery before six months, the ideal is one year of the previous surgical procedure, although some small adjustments may be allowed [39,40].
Do not forget about other anatomical considerations such as the ocular plane, the strength of the canthal tendons, or canthal or ocular dystopias, without situations that will condemn us to failure. Some minor complications may improve with time, massages or anti-inflammatory or topical medications, so surgery should not be rushed. The pressure exerted by the patient for the correction of deformities is frequent. It is important to explain to the patient the need for patience, but above all the most patient should be the surgeon in not wanting to do something ahead of time. It should always be considered that the eyelid is suspended only from the canthal tendons, which is why it is very easy to alter the forces that maintain this balance, as well as to understand the concept of the anterior and posterior plates in order to analyze and solve the problems of bad palpebral positions.
Major or Catastrophic Complications
They occur in one of every 10,000 or 20,000 cases and can be during the surgical act or several days later, this may be due to inadequate control of bleeding, especially in the nasal fat compartments, also due to the eruption of deep vessels After manipulation of the eyelid fat, another possibility is the section of the eyelid vessels during the injection of local anesthetic, especially if there is hypertension, coagulopathy or the use of some drugs such as aspirin, anticoagulants or vitamin E, since they favor this kind of complications. It is ideal to stop any unnecessary drugs before surgery [40, 41].
The surgeon must be able to recognize the early signs of retrobulbar hemorrhage as sudden pupillary changes, proptosis, loss of visual acuity, altered eye movements, visual fields, or color disorders will occur.
Precautions: The patient’s eyes should never be blindfolded, since he will be the first to notice when experiencing loss of visual acuity, alteration of visual fields or changes in the perception of colors, the doctor must instruct the patient to evaluate your visual acuity frequently and it is the surgeon’s obligation to check it before discharge. The surgeon must be trained to follow the protocol for decompression of the eyeball and optic nerve through a canthotomy and cantolysis, which must be performed under conditions of true urgency, must be familiar with the systemic administration of mannitol and topical medications to help reduce intraocular pressure and prevent optic nerve ischemia. Steroids and carbonic monohydrase inhibitors help, this should be known to whoever performs a blepharoplasty. Anterior chamber paracentesis should only be performed by a trained ophthalmologist. Once the eyeball decompression protocol has been carried out, the patient must return to the operating room in order to corroborate hemostasis and repair decompressive canthal surgery [42-44].
Types of Injury:
1. Loss of visual acuity
This can occur from inadvertent penetration of the eyeball, retrobulbar hemorrhage, glaucoma, or corneal injury. Eyeball perforation, although rare, is devastating, so a corneal protector should always be worn and care should be taken when handling instruments that may fall into the eye area. Lesions of the extraocular musculature can be precipitated during infiltration of local anesthesia, although it is more frequent that they are damaged during surgical dissection, especially the lesion of the inferior oblique muscle since it originates in the anterior part of the orbit and is located between the central and middle pad of the lower eyelid, while in upper blepharoplasty the lesions, although infrequent, involve the upper obliques, in the trochlear region.
2. Corneal injury is one of the most frequent problems, although although they heal spontaneously, they are the cause of very significant discomfort and are usually due to injury with instruments or sutures on the cornea where there was repeated trauma. The treatment is to use a lubricant or a corneal protector with an antibiotic ointment, although it is better to refer it to the specialist. The use of topical anesthetics to reduce discomfort considerably delays healing, which is why it is not recommended.
3. -Permanent deformities of the eyelid
This may imply not only a bad eyelid position but also injuries to the lacrimal system. Ptosis in the upper eyelid and retraction in the lower eyelid [45-48].
Minor Complications
Minor complications can consist of a large number of problems such as bleeding, infection, corneal or tear duct injuries, inflammatory deformities, as well as of the eyelids such as epicantal folds, scars, dermal cysts, sclera show, ectropion or entropion [49]. The dehiscences of the acute or subacute wound occur days or weeks even after the same either due to inadequate closure of the suture, formation of a hematoma, seroma or even by the use of drugs such as steroids that delay healing used in large doses in the perioperative.
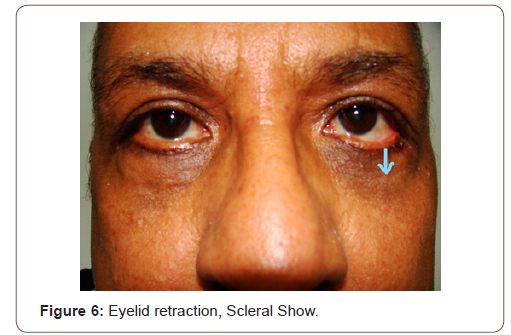
Alterations in The Position of the Eyelid: Eyelid alterations are very frequent and can occur in both eyelids, the most frequent being an eyelid retraction due to poor management of the middle lamina, where the recommendation is not to manipulate or suture in the orbital septum. In the case of ectropion: it is due to an overresection of the anterior lamina where this force predominates over that of the posterior lamina and causes the eyelid to turn outward, the patient becoming very symptomatic due to ocular dryness and discomfort from exposure conjunctival.
In the case of entropion: they are due to a contraction of the posterior lamina due to an elongation of the anterior lamina or even an excess of cauterization on the conjunctiva and the palpebral retractors. By turning in the free edge of the eyelid, the eyelashes will end up eroding the cornea. The correction of these alterations in the position of the eyelid is based on the theory of the three plates, where the balance of the anterior and posterior plates are the logical essence for the treatment of these problems. It is worth mentioning that an upper eyelid problem in palpebral ptosis which can occur as a consequence of the same blepharoplasty or as a consequence of other types of ocular procedures such as cataract or correction of strabismus, and its management is carried out based on the tendon of the aponeurosis of the elevated. Some patients, especially elderly patients, have a certain degree of muscle weakness or disinsertion presenting an involutive ptosis. To avoid this, gentle tissue handling is recommended and blepharostat avoidance as much as possible [50, 51].
Infection is very rare due to the great vascularity of the face, however conjunctivitis and dacryocystitis can predispose the appearance of these. The loss of eyelashes occurs when the incision is made very close to the eyelid edge, injuring the hair follicles and causing their loss in the postoperative period. It should be mentioned that eyelid retractions are frequent in endocrine exophthalmos, so eyelid surgery should be avoided if you do not have experience and are not trained to manage this type of patient. Retraction of the lower eyelid or “scleral show” is a frequent problem and very annoying for the patient, being one of the most common causes of complaint in the postoperative period of blepharoplasty, in the lower eyelid skin resection should be very conservative [52].
Alterations Caused by the Surgery Itself: These alterations are the most frequent and may consist of over-drying or underdrying of skin, fat, or other tissues. In relation to the skin in the upper eyelid, it can be a more generous one, while in the lower one, overresection is very serious, where it must be conservative and think that the transposition of fat should occupy a preponderant place [53-58]. Care should be taken when reversing the lacrimal point as this will cause constant epiphora, so it is not recommended that the incisions exceed the lacrimal point. When there are these types of problems, patience is important and do not undergo surgery before a year since many of these malformations will improve considerably with the use of massages in the affected area and with ointments, since this will improve fibrosis.
Sunscreen and the use of artificial tears are beneficial in the first months. Insufficient skin or fat resection must be evaluated intraoperatively with the various maneuvers that have been devised to evaluate and avoid this type of problem, the correction of which avoids secondary surgery. During the first days and tearing can be frequent and in later weeks dry eyes can occur, here artificial tears work correctly, this due to the same inflammatory phenomenon [59].
Conclusion
Although simple in appearance, eyelid surgery can frequently present complications and is a frequent cause of demand towards doctors dedicated to performing facial plastic surgery, although skill, anatomical knowledge and experience are essential to avoid complications These can occur even to experienced surgeons. The affective part and psychological management are important in these patients.
Most complications are avoidable if a correct medical history is carried out, adequate instruments are used and a refined surgical technique is used, where anatomical knowledge is essential, as well as understanding the orbital and lacrimal physiology and how the correct balance of the eyelid is in your muscular aponeurotic and ligamentous system, they will help to have consistent and uncomplicated results. It never hurts to reiterate that patience can be decisive to resolve complications and that no type of tissue should ever be thrown during surgery, since sometimes in case of over resection this tissue can be used as a free graft in various situations.
Recommendations When there are Complications in Blepharoplasty
1. IF YOU DO NOT KNOW HOW TO SOLVE A COMPLICATION OR YOU DO NOT HAVE EXPERIENCE… DO NOT OPERATE IT. IT WILL SURE YOU CAUSE MORE HARM THAN BENEFIT. Refer experienced people.
2. Blepharoplasty may not be the best option for everyone.
3. The incisions are important, some people have more tissue on the eyelids and therefore a greater healing surface; in some cases a small visible scar line may remain. This type of surgery like all can cause permanent scars. Remind the patient.
4. Dark circles are NOT removed with blepharoplasty and this is also true for most external canthal wrinkles or crow’s feet. This surgery will improve and strengthen the appearance of the upper and lower area of the eye, however it will eliminate any problem with sunken or droopy eyes or bags. That is why it is important to know the expectations of patients, many confuse the need for surgery with a problem that does not require it.
5. Each method is intended to remove any excess tissue causing the drop, including fat and muscle. But there are also multiple problems apart from fat and redundant skin related to the eyelid. It requires being trained to recognize them and avoid complications.
6. The final choice of what to do will depend on several factors. These factors include the surgeon who performs the intervention, the severity of the sagging skin, and various types of procedures, techniques and methods can be combined.
7. Complications can range from mild to severe or even life threatening. THE patient must ALWAYS be informed and sign the consent. Keep complications in mind, not to be nervous but to avoid committing them.
8. In any surgery, however minimal it may seem, there is always the risk of complications.
9. In all respects…. If you are not trained to perform a blepharoplasty... do not do it.
10. If you are not able to recognize a complication, it is most likely that you cannot solve it, then... do not try.
Appendix1


Appendix2
Informed Consent for Blepharoplasty
(“Eyelid Surgery”)
1. What can be the reason for an eyelid surgery?
With age, the skin and muscles of the eyelid can loosen and sag. Also, the fat that surrounds and protects the eyeball can leak forward through the skin of the upper and lower eyelids. Excess skin, muscle, and fat can pull down the upper eyelid and, in some cases, obstruct vision. This can lead to fatigue, eye strain, skin irritation, and loss of peripheral vision. Excess skin, muscle, and fat also create what many consider to be an unattractive aging appearance, especially on the lower eyelids (“bags under the eyes”).
2. What is blepharoplasty?
A blepharoplasty is the removal or repositioning of tissue that may include skin, muscle, and fat from the upper and/or lower eyelids. In the upper eyelid, the incision is made in the natural lid crease to hide it. In the lower eyelid, an incision can be made along the skin just below the eyelashes, or along the moist inner surface of the eyelid, known as the conjunctiva.
3. How will this eyelid surgery affect my vision or appearance?
The results of blepharoplasty depend on the symptoms of each patient, their unique anatomy, what is expected to be obtained in terms of appearance and the ability to adapt to changes. Blepharoplasty only corrects vision loss due to excess skin, muscle, and fat blocking the eye. By removing this excess skin, muscle, and fat that is blocking the eye, upper eyelid blepharoplasty can allow more light in and can improve peripheral vision. Blepharoplasty does not improve blurred vision caused by problems inside the eye or visual loss due to age, most patients consider that blepharoplasty improves their appearance and makes them look younger. However, some patients have unrealistic expectations about the impact that the change in appearance can have on their lives. Others may find it difficult to adjust to changes in their appearance. You will need to make a careful assessment of your goals and your ability to cope with changes in your appearance before agreeing to undergo this surgery.
4. What are the main risks associated with blepharoplasty?
Risks of blepharoplasty include, but are not limited to: bleeding, infection, asymmetrical or unbalanced appearance, scarring, difficulty closing the eyelids (which can damage the underlying corneal surface), double vision, tearing or dry eye problems, inability to wearing contact lenses, numbness and/or tingling near the eye or on the face, and, in rare cases, loss of vision. You may need additional treatment or surgery to treat these complications; the cost of additional treatment or surgery is NOT included in the cost of this surgery. Due to individual anatomical differences, differences in response to surgery, and differences in healing, no guarantees can be made as to final results. For some patients, changes in appearance can lead to feelings of anger, anxiety, depression, or other emotional reactions.
5. What are the alternatives?
You may be willing to live with the symptoms and the appearance of extra skin, muscle, and fat around your eyes, and you may decide not to have eyelid surgery for now. In some cases, the appearance of excess skin and oil on the lower eyelids can be improved with a treatment to renew the skin’s surface (with the use of lasers, known as dermabrasion, or chemical peeling) and/or fillers, injectables.
6. What type of anesthesia is used? What are the main risks?
Most blepharoplasties are performed under “local” anesthesia, that is, injections that are given around the eye to numb the area. You may also receive sedation through a needle placed into a vein in your arm or given as pills that are taken before surgery. Risks of anesthesia include but are not limited to: damage to the eye and surrounding tissues and structures, loss of vision, breathing problems, and in very rare circumstances, stroke or death.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Hester TR, Douglas T (2009) Szczerba Decreasing complications in lower lid and midface rejuvenation: the importance of orbital morphology, horizontal lower lid laxity, history of previous surgery, and minimizing trauma to the orbital septum: a critical review of 269 consecutive cases. Plast Reconstr Surg 123(3): 1037-1049.
- John P Fezza (2008) Nonsurgical treatment of cicatricial ectropion with hyaluronic acid filler. Plast Reconstr Surg 121(3): 1009-1014.
- Krastinova D, Jasinski M (2004) Aesthetic blepharoplasties, complications and treatment. Ann Chir Plast Esthet 49(6): 569-585.
- Glavas IP (2005) The diagnosis and management of blepharoplasty complications. Otolaryngol Clin North Am 38(5): 1009-1021.
- Pak J, Putterman AM (2005) Revisional eyelid surgery: treatment of severe postblepharoplasty lower eyelid retraction. Facial Plast Surg Clin North Am 13(4): 561-569.
- Lyon DB, Raphtis CS (1997) Management of complications of blepharoplasty. Int Ophthalmol Clin 37(3): 205-216.
- Black J (1998) Complications following blepharoplasty. Plast Surg Nurs 18(2): 78.
- Keyes GR, Singer R, Iverson RE, McGuire M, Yates J, et al. (2008) Mortality in outpatient surgery. Plast Reconstr Surg 122: 245-250.
- Hoefflin SM, Bornstein JB, Gordon M (2001) General anesthesia in an office-based plastic surgical facility: a report on more than 23,000 consecutive office-based procedures under general anesthesia with no significant anesthetic complications. Plast Reconstr Surg 107: 243-251.
- Whippey A, Kostandoff G, Paul J, Ma J, Thabane L, et al. (2013) Predictors of unanticipated admission following ambulatory surgery: a retrospective case-control study. Can J Anaesth 60: 675-683.
- Oestreicher J, Mehta S (2012) Complications of Blepharoplasty: Prevention and Management. Plast Surg Int 252368.
- Holds JB, Anderson RL, Thiese SM (1990) Lower eyelid retraction: a minimal incision surgical approach to retractor lysis. Ophthalmic Surg 21(11): 767-771.
- Patipa M (2000) The evaluation and management of lower eyelid retraction following cosmetic surgery. Plast Reconstr Surg 106(2): 438-440.
- Patel BCK, Patipa M, Anderson RL, McLeish W (1997) Management of postblepharoplasty lower eyelid retraction with hard palate grafts and lateral tarsal strip. Plast Reconstr Surg 99(5): 1251-1260.
- Ferri M, Oestreicher JH (2002) Treatment of post-blepharoplasty lower lid retraction by free tarsoconjunctival grafting. Orbit 21(4): 281-288.
- Hawes MJ, Jamell GA (1996) Complications of tarsoconjunctival grafts. Ophthalmic Plast Reconstr Surg 12(1): 45-50.
- Leone CR, Van Gemert JV (1989) Lower lid reconstruction using tarsoconjunctival grafts and bipedicle skin-muscle flap. Arch Ophthalmol 107(5): 758-760.
- Stephenson CM, Brown BZ (1985) The use of tarsus as a free autogenous graft in eyelid surgery. Ophthalmic Plast Reconstr Surg 1: 43-50.
- Hester TR (1998) The trans-blepharoplasty approach to lower lid and midfacial rejuvenation revisted: the role and technique of canthoplasty. Aesthet Surg J 18(5): 372-376.
- Anderson RL, Gordy DD (1979) The tarsal strip procedure. Arch Ophthalmol 97(11): 2192-2196.
- Jordan DR, Anderson RL (1989) The lateral tarsal strip revisited: the enhanced tarsal strip. Arch Ophthalmol 107(4): 604-606.
- Oestreicher JH, Pang NK, Liao W (2008) Treatment of lower eyelid retraction by retractor release and posterior lamellar grafting: an analysis of 659 eyelids in 400 patients. Ophthalmic Plast Reconstr Surg 24(3): 207-212.
- Edgerton MT (1972) Causes and prevention of lower lid ectropion following blepharoplasty. Plast Reconstr Surg 49(4): 367-373.
- Shaw GY, Khan J (1996) The management of ectropion using the tarsoconjunctival composite graft. Arch Otolaryngol Head Neck Surg 122(1): 51-55.
- Anderson RD, Lo MW (1998) Endoscopic malar/midface suspension procedure. Plast Reconstr Surg 102(6): 2196-2208.
- Gunter JP, Hackney FL (1999) A simplified transblepharoplasty subperiosteal cheek lift. Plast Reconstr Surg 103(7): 2029-2041.
- Hass AN, Penne RB, Stefanyszyn MA, Flanagan JC (2004) Incidence of postblepharoplasty orbital hemorrhage and associated visual loss. Ophthalmic Plast Reconstr Surg 20(6): 426-432.
- Goldberg RA, Marmor MF, Shorr N, Christenbury JD (1990) Blindness following blepharoplasty: two case reports, and a discussion of management. Ophthalmic Surgery 21(2): 85-89.
- Goldberg RA, Li TG (2002) Postoperative infection with group A beta-hemolytic Streptococcus after blepharoplasty. Am J Ophthalmol 134(6): 908-910.
- Rao J, Golden TA, Fitzpatrick RE (2002) Atypical mycobacterial infection following blepharoplasty and fullface skin resurfacing with CO2 laser. Dermatol Surg 28(8): 768-771.
- Safranek TJ, Jarvis WR, Carson LA (1987) Mycobacterium chelonae wound infections after plastic surgery employing contaminated gentian violet skin-marking solution. N Engl J Med 317: 197-201.
- Schendel SA, Stephanides M (1996) Treatment of periorbital edema with human corticotropin-releasing factor after blepharoplasty. J Am Coll Surg 182(3): 226-232.
- Glavas IP (2005) The diagnosis and management of blepharoplasty complications. Otolaryngol Clin North Am 38(5): 1009-1021.
- Yachouh J, Arnaud D, Psomas C, Arnaud S, Goudot P (2006) Amaurosis after lower eyelid laser blepharoplasty. Ophthalmic Plast Reconstr Surg 22(3): 214-215.
- Goldbeg RA, Marmor MF, Shorr N, Christenbury JD (1990) Blindness following blepharoplasty: two case reports and a discussion of management. Ophthalmic Surg 21: 85-89.
- Good CD, Cassidy LM, Moseley IF, Sanders MD (1999) Posterior opitc nerve infarction after lower lid blepharoplasty. J Neuroophthalmol 19(3): 176-179.
- Kelly PW, May DR (1980) Central retinal artey occlusion following cosmetic blepharoplasty. Br J Ophthalmol 64: 918-922.
- Enzer YR, Shorr N (1994) Medical and surgical management of chemosis after blepharoplasty. Ophthalmic Plast Reconstr Surg 10(1): 57-63.
- Cheng JH, Lu DW (2007) Perilimbal needle manipulation of conjuctival chemosis after cosmetic lower eyelid blepharoplasty. Ophthalmic Plast Reconsr Surg 23(2): 167-169.
- McKinney P, Byun M (1999) The value of tear film breakup and Schirmer´s tests in preoperative blepharoplasty evaluation. Plast Reconstr Surg 104(2): 566-569.
- De Lima CB, Siqueira GB, Cardoso IH (2006) Evaluation of dry eye in the preoperative and postoperative period of blepharoplasty. Arq Brs Oftalmol 96(3): 377-382.
- Ghabrial R, Lisman RD, Kane MA (1998) Diplopia following transconjuncival blepharoplasty. Plast Reconstr Surg 102(4): 1219-1225.
- Putterman AM (2004) Acquired strabismus following cosmetic blepharoplasty. Plast Reconstr Surg 113(3): 1069-1070.
- Schlenker JD, Slavin SA (2006) Proptosis immediately following blepharoplasty due to an inferior rectus intramuscular hematoma. Ann Plast Surg 56(4): 437-438.
- Patipa M, Wilkins RB (1994) Acquired ptosis in patients undergoing upper eyelid blepharoplasty. Ann Ophthalmol 16: 266-270.
- Petrelli RL (1988) The treatment of lacrimal gland prolapse in blepharoplsty. Ophthalmic Plast Reconstr Surg 4: 139.
- Lyon DB, Raphtis CS (1997) Management of complications of blepharoplasty. Int Ophthalmol Clin 37(3): 205-216.
- Morax S, Touitou V (2006) Complications of blepharoplasty. Orbit 25(4): 303-318.
- Nerad JA (2001) Periorbital involutional alterations: dermatochalasia and ptosis of the eyebrows. In: Nerad JA. Ophthalmology requirements. Oculoplastic surgery. Madrid: Harcourt 141-146.
- Fulton JE (1999) The complications of blepharoplasty: their identification and management. Dermatol Surg 25(7): 549-558.
- Rosenberg DB, Lattman J, Shah AR (2007) Prevention of lower eyelid malposition after blepharoplasty: anatomy and technical considerations of the inside-out blepharoplasty. Arch Facial Plast Surg 9(6): 434-438.
- Pak J, Putterman AM (2005) Revisional eyelid surgery: treatment of severe postblepharoplasty lower eyelid retraction. Facial Plast Surg Clin North Am 13(4): 561-569.
- Patel BC, Patipa M, Anderson RL, McLeish W (1997) Management of postblepharoplasty low eyelid retraction with hard palate grafts and lateral tarsal strip. Plast Reconstr Surg 99(5): 1251-1260.
- Darlington JD, Lee WB, Schwab IR (2006) Corneal perforation durng laser blepharoplasty. Ophthalmic Surg Lasers Imaging 37(4): 327-329.
- Suñer IJ, Meldrum ML, Johnson TE, Tse DT (1999) Necrotizing fascitis after cosmetic blepharoplasty. Am J Ophthalmol 128(3): 367-368.
- Ogata H, Kurosaka D, Nakajima T, Sasaki K, Oshiro T (2005) Myopic change after transconjuctival blepharoplasty using carbon dioxide laser: case report. Aesthetic Plast Surg 29(4): 313-316.
- Schiller JD, Lin S, Neigel JM (2004) Deepening of the superior sulcus after isolated lower transconjuctival blepharoplasty. Ophthalmic Plast Reconstr Surg 20(6): 433-435.
- Rosenthal EL, Baker SR (1999) Development of Graves orbitopathy after blepharoplasty. A rare complication. Arch Facial Plast Surg 1(2): 127-129.
- Toledano Fernández N, García Sáenz S, Sánchez Cruz J (2005) Labial combustion burn during blepharoplasty. Arch Soc Esp Oftalmol 80(5): 297-300.
-
Marcos Antonio Rodriguez Perales, Francisco Javier Saynes Marin. Complications in Blepharoplasty and How to Resolve Them. On J Otolaryngol & Rhinol. 4(5): 2021. OJOR.MS.ID.000597.
-
Blepharoplasty complication, Cosmetic surgeries, Facial surgery, Reconstructive problems, Lymphedema, Inflammatory phenomenon, Facial plastic surgery, Breathing problems, transconjunctival surgery.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






