 Research Article
Research Article
Evaluation of Methods of Denture Cleaning
Zeynep Yeşil Duymuş1,2 and Sebahat Findik Aydiner3*
1Atatürk University, Faculty of Dentistry, Department of Prosthodontics, Erzurum, Turkey
2Recep Tayyip Erdoğan University Faculty of Dentistry, Department of Prosthodontics, Rize, Turkey
3Dentist, Ministry of Health Yıldırım Beyazıt University Yenimahalle Training and Research Hospital-District Polyclinic, Ankara, Turkey
Sebahat Findik Aydiner, Dentist, Ministry of Health Yıldırım Beyazıt University Yenimahalle Training and Research Hospital-District Polyclinic, Ankara, Turkey.
Received Date: March 26, 2021; Published Date: April 14, 2021
Abstract
Methods: The study, in which 180 dentists living in different regions participated, was carried out through a survey on Google Drive.
Results: 179 dentists (99.4%) participating in the survey stated that they had informed their wearers on denture care, while 1 (0.6%) stated that they had not offer such information. Prosthesis cleaning with soap and toothbrush is the most recommended method (100 dentists). When the methods employed by wearers in denture cleaning are evaluated according to their frequency of use, it was determined that soaking was the most commonly applied method, followed by cleaning with toothpaste and a toothbrush and cleaning with soap and a toothbrush.
Keywords: Cleansers; Denture; Stomatitis
Introduction
In the context of the construction of removable dentures, microorganisms find suitable areas to attach to and multiply in with surface irregularities inherent in the materials used for this purpose, as well as with interdental areas, fixation elements such as clasps, and small scratches that may occur during levelling [1- 3]. The literature on bacterial plaques on dentures identified more than 2 million bacteria on a bacterial plaque of 1mg. The species observed among such bacteria included Streptococcus sanguis, Streptococcus mutans, Beta and Group D streptococci, Lactobacillus spp., Fusobacterium spp., alpha- and gamma-haemolytic Streptococci, Diphtheroids, Bacillus, Staphylococci, Escherichia coli, micrococcus spp., Klebsiella pneumoniae, Staphylococcus aureus, Pseudomonas stutzeri, Enterobacter cloacae, Neisseria, and Candida [2, 4, 5].
Dental plaques are known to cause severe staining and aesthetic problems [6]. Regular oral care is among the preconditions for the prevention and treatment of external staining [7]. Aesthetic concerns and halitosis aside, the elimination of any plaque accumulation on the internal surface is of consequence also for the well-being of the soft tissues in contact with and supporting the denture. Such accumulation may result in the symptom complex, commonly known as “denture stomatitis”, combining inflammatory papillary hyperplasia and chronic candidiasis. Any deterioration in oral health arising from a misfit of the denture surface or trauma will become more severe with poor dental cleaning. Denture plaque has been specified as the main cause of inflammation in palatal mucosa [8]. There is a known correlation of significance between severe inflammation and poor denture cleaning [6].
A case of denture stomatitis is treated with an antifungal to contain oral fungi, to relieve existing trauma and occlusal problems, and to secure denture and oral hygiene. The most important element in this course of treatment is represented by oral and denture hygiene [9, 10]. The treatment of denture stomatitis presenting without any trauma in aetiology also requires denture cleaning to eliminate Candida [10, 11]. Today, there are two methods available for denture cleaning, i.e., mechanical, and chemical cleaning [12- 14]. Mechanical cleaning employs brushing, ultrasonic devices, and microwave energy [13-15], while chemical methods are applied with alkaline peroxides, alkaline hypochlorites, diluted acids, disinfectants, and enzymes [10, 16, 17].
Brushing is a method easily accessible by denture wearers. However, care must be taken to choose a brush with synthetic and long bristles featuring rounded tips. Denture wearers generally combine such a brush with soap, toothpaste, zirconium produced for denture cleaning, or a paste or powder containing Ca-carbonate or Ca-phosphate. Fine-grained chemical agents must be combined with the right brush to alleviate abrasive effects of cleaning. The literature has reported that sufficient cleaning can be secured with two-minute brushing twice a day [18]. Microwave energy is rarely employed in denture cleaning. However, an increase is foreseen in the use of this method along with the current availability of microwave ovens in every household. A relevant study identified that a denture infected with Candida can be sterilised in 6 minutes under 350 Watts in a kitchen-type microwave oven. However, such successful sterilisation is undermined by the need for the mechanical elimination of debris with an ultrasonic device or through brushing [19].
Ultrasonic devices are quite effective [20] in the elimination of tartar on denture surfaces but are not deemed sufficient by themselves and are recommended to be used in combination with disinfecting solutions [21]. Effervescent tablets or liquid denture cleaning agents containing alkaline peroxide also feature sodium perborate, which contribute to micro-mechanical cleaning by providing for the release of percarbonate oxygen. On the other hand, trisodium phosphate in their content is an alkaline detergent that reduces surface tension [22]. For effective cleaning, dentures are recommended to be left in such solutions for a few hours or overnight [1, 22].
The use of alkaline hypochlorite in denture cleaning is known not to be effective in the elimination of tartar. Such cleaning agents inhibit the formation of tartar by eliminating the organic matrix on it. Various concentrations of Na hypochlorite solutions have been identified to be in common use [23, 24]. The present study was conducted with the aim of identifying the cleaning methods recommended by physicians around the country to the denture wearers and to determine whether there is a correlation between the sex, socioeconomic level, and age of denture wearers and their denture cleaning habits. The hypothesis behind the study is that there is a higher percentage of removable dentures among physicians and there will be differences in the level of cleaning by sex and age.
Materials and Methods
The present study was undertaken through the preparation of survey questions for dentists and specialist dentists employed in the public or private sector or at universities and the delivery of the same to the target audience on Google Drive. The survey questions are shaped around the products employed in denture cleaning; their recommended frequency of use; the manner of use for chemical agents; time required for cleaning; and the existence or absence of a correlation between the socioeconomic status, sex, and age of the denture wearers and their denture cleaning habits. The goals of the study also includes the identification of the percentages of the denture wearers with fixed dentures and those with removable dentures. The study received an approval from the Ethics Board of the Faculty of Dentistry under Atatürk University (2020/44).
Results
A total number of 180 dentists participated in the study. Of the dentists, 112 (62.20%) respondents were identified to be under the age of 35; 57 (31.7%) between the ages of 36-45; 10 (5.6%) between the ages of 46-65; and 1 (0.5%) over 66 years old; while 47 (26.1%) respondents lived in the Black Sea region; 37 (20.6%) in Central Anatolia; 27 (15.0%) in the Marmara region; 26 (14.4%) in the Eastern Anatolia region; 20 (11.1%) people in the Aegean region, 12 (6.7%) in the Mediterranean region; and 11 (6.1%) in the South-Eastern Anatolia region. Among the dentists participating in the study, 80 (44.4%) had working experience between 0-5 years; 35 (19.4%) between 6-10 years; 35 (19.4%) between 11-15 years; and 30 (16.8%) people over 16 years, while 110 (61.1%) worked at a university; 51 (28.3%) in a Public Hospital/Oral and Dental Health Centre; 15 (8.3%) in a private polyclinic; and 4 (2.3%) people in a private practice. Furthermore, 59 (32.8%) respondents did not have any specialisation; 113 (62.8%) specialised in prosthetic dental treatment; 2 (1.1%) in restorative dental treatment; 1 (0.6%) in orthodontics; 3 (1.7%) in paediatric dentistry; 1 (0.6%) in periodontology; and 1 (0.6%) in oral and maxillofacial surgery.
The ratio of the denture wearers treated was indicated as 51% and above for 111 (61.7%) dentists; 21-50% for 29 (16.1%) dentists; 11-20% for 12 (6.7%) dentists; 6-10% for 12 (6.7%) dentists; 0-5% for 16 (8.9%) dentists. The ratio of the ones using removable dentures to the total number of denture wearers was specified by 89 (49.4%) dentists as 21-50%; by 41 (22.8%) dentists as 11-20%; by 23 (12.8%) dentists as 51% and above; by 15 (8.3%) dentists as 0-5%; and 12 (6.7%) dentists as between 6-10%.
The ratio of denture wearers with knowledge of denture cleaning was indicated by 53 (29.4%) dentists as 6-10%; by 41 (22.8%) dentists as 11-20%; by 39 (21.7%) dentists as 29-50%; by 38 (21.1%) dentists as 0-5%; and by 9 (5.0%) dentists as 51% and above.
Among the participants of the survey, while 93 (51.7%) dentists think that women are better at denture cleaning, 86 (47.8%) dentists think that it is not related to gender, and 1 (0.6%) dentist thinks that men are better at denture cleaning. To the question of whether there is any correlation between prosthesis cleaning and age; 91 (50.6%) dentists answered that denture wearers of advanced age could not clean their dentures adequately, 87 (48.3%) dentists answered that denture cleaning was not related to age, and 2 (1.1%) dentists answered that the denture wearers of younger age could not clean their dentures adequately. The socio-economic status of the denture wearers with good prosthetic care was stated to be good by 121 (67.2%) dentists, to be moderate by 39 (21.7%), to be very good by 18 (10%), and to be poor by 2 (1.1%).
When the methods used by the wearers in denture cleaning are evaluated by frequency; it was determined that they most commonly washed their dentures in running water (47), followed by cleaning with toothpaste and a toothbrush (13) and cleaning with soap and a toothbrush (11) (Table 1).
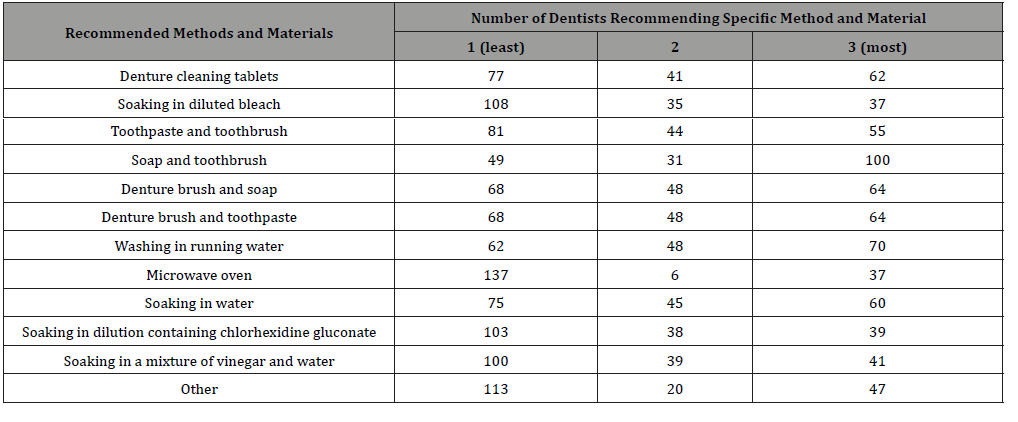
Denture cleaning tablets were among the most commonly recommended methods among the methods recommended for the denture wearers experiencing difficulties with denture cleaning, followed by soap and a toothbrush, denture brush, and cleaning with soap (Table 2). The use of soap and a toothbrush represents the most commonly recommended method among the first three methods recommended for the denture wearers from a low socioeconomic level (Table 3). 179 (99.4%) dentists responding to the survey stated that they informed their denture wearers about denture care, while 1 (0.6%) stated that they did not offer such information. The question as to the stage where the denture wearers should be informed on denture cleaning was answered by 159 (88.3%) dentists with the handover of dentures, by 20 (11.1%) with the initial examination, and by 1 (0.6%) with followup sessions.
Table 1: Frequency of use of methods employed in denture cleaning.
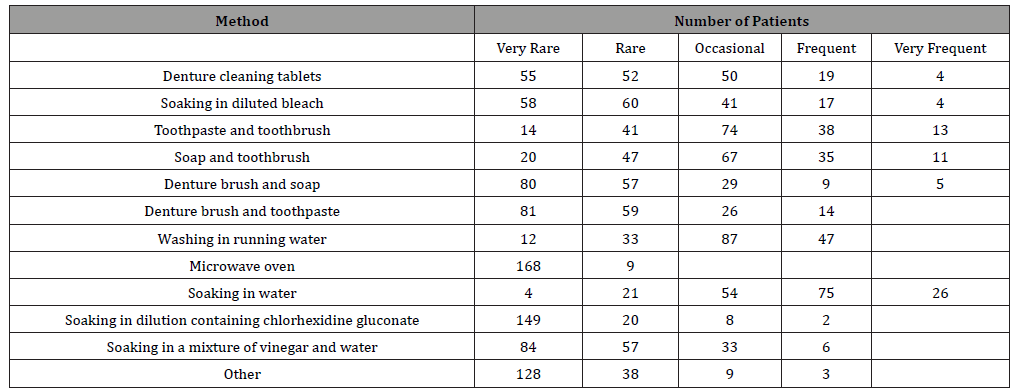
Table 2: First three methods most commonly recommended for patients experiencing difficulties with denture cleaning (marked as 1, 2, and 3).
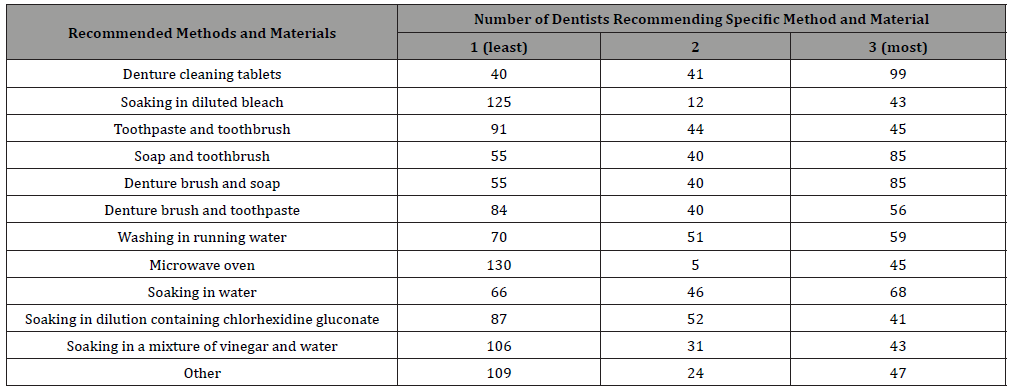
Table 3: First three methods most commonly recommended to patients from a low socio-economic level (marked as 1, 2, and 3).
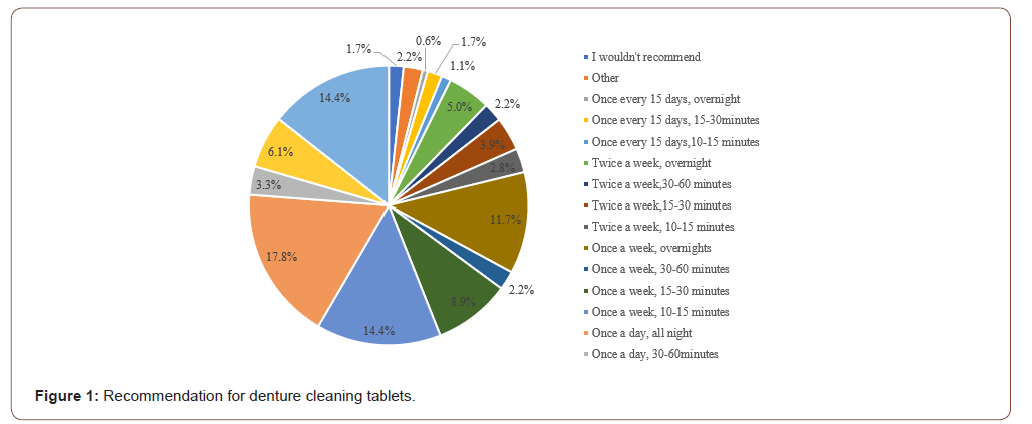
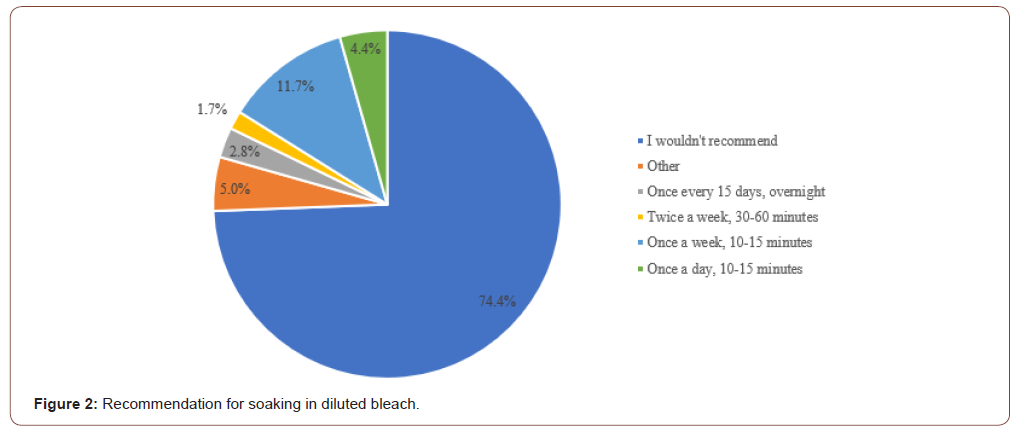
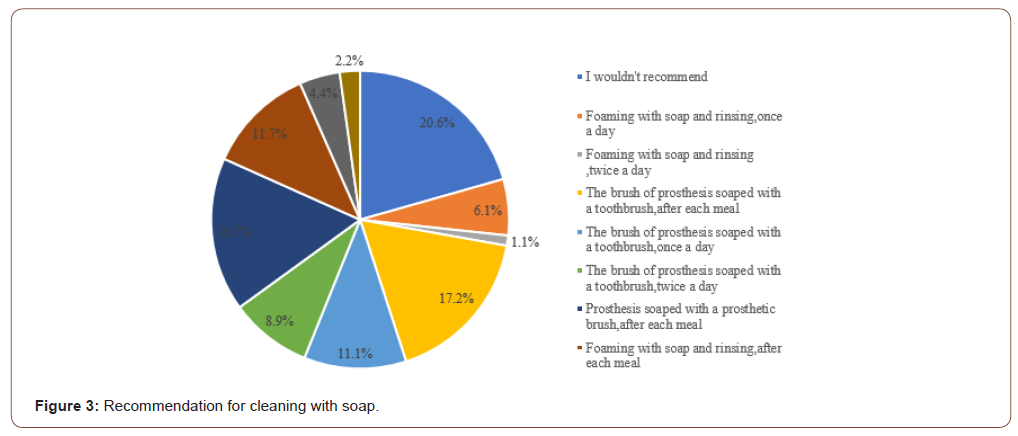
90 (50%) dentists stated that they allocated 1-2 minutes and 90 (50%) dentists 5 minutes to explain denture cleaning and relevant methods to the denture wearers who were not able to perform denture cleaning. The use of denture cleaning tablets once a day overnight was recommended by 32 (17.8%) dentists, while 26 (14.4%) recommended such use for 15 minutes once a day, and 26 (14.4%) recommended such use for 15 minutes once a day (Figure 1). 137 (74.4%) dentists indicated that they did not recommend soaking in diluted bleach (Figure 2). 37 (20.6%) dentists indicated that they did not recommend cleaning with soap (Figure 3).
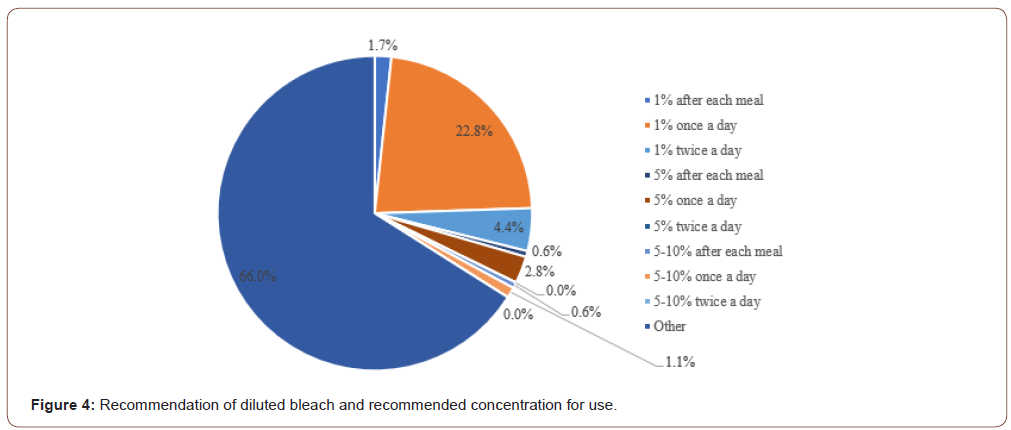
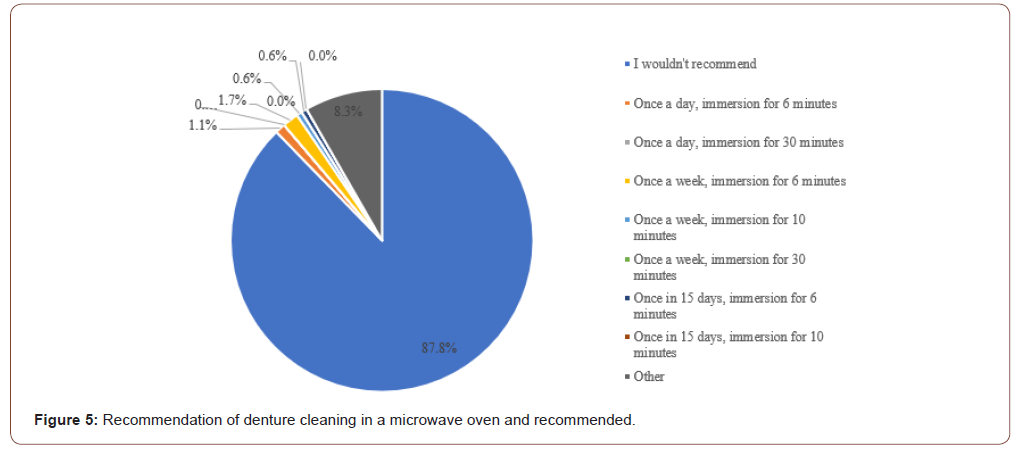
In response to the question as to which concentration and frequency they would recommend for diluted bleach, 158 (87.8%) dentists indicated that they did not recommend this method, while 15 (8.3%) stated that they recommended soaking for more than 30 minutes once a week; 3 (1.7%) dentists once a week for 6 minutes; 2 (1.1%) dentists once a day for 6 minutes; and 1 (0.6%) dentist once a week for 10 minutes with 15 (58.3) dentists marked other options (Figure 4). 158 (87.8%) dentists indicated that they did not recommend denture cleaning in a microwave oven (Figure 5).
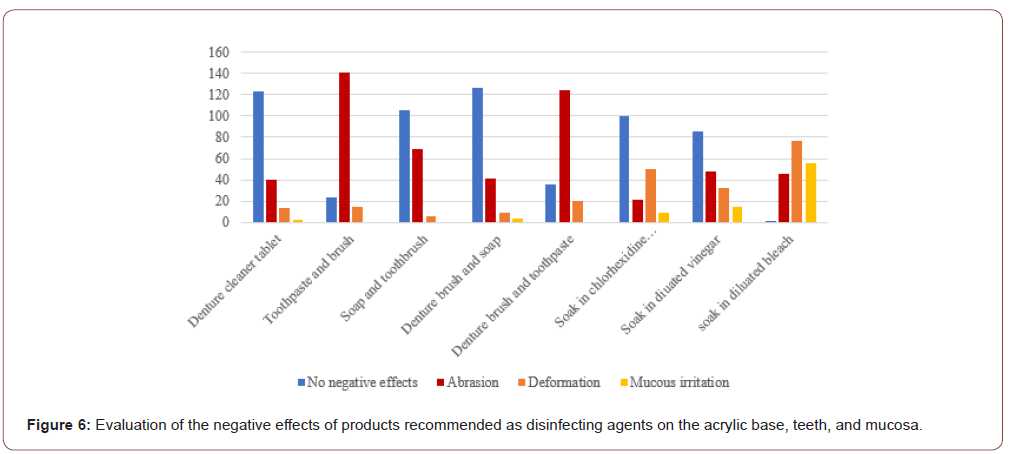
In response to the question as to which disinfection method they used before handing over dentures to a patient in the clinic, 39 (21.7%) dentists stated that they kept dentures in water containing chlorhexidine in gluconate; 29 (16.1%) that they washed dentures in running water; 15 (8.3%) that they cleaned dentures with a denture brush and soap; 7 (3.9%) that they cleaned dentures with soap and a toothbrush; 2 (1.1%) that they cleaned dentures with toothpaste and a toothbrush; 14 (7.8%) that they soaked dentures in diluted bleach; 11 (6.1%) that they used denture cleaning tablets; and 1 (0.6) that they kept dentures in a mixture of vinegar and water, while 54 (30%) dentists marked other. When the products recommended as disinfecting agents are evaluated according to their negative effects on the acrylic base, teeth, and mucosa; 123 dentists reported that denture cleaning tablets had no negative effect, while 56 dentists reported that soaking in diluted bleach caused mucosal irritation (Figure 6).
Discussion
The present study aimed to conduct a survey among dentists living in different geographical regions of the country and thus to identify the ratio of their patients using removable dentures to their total number of denture wearers and their recommendations to those with respect to methods of denture cleaning, as well as whether there are differences in the level of denture cleaning arising from all the denture wearers’ sex and age. The goal of identifying the ratio of the use of removable dentures was achieved with the ratio of the denture wearers using removable dentures to the total number of those with dentures being specified by 89 (49.4%) dentists as 21-50%; by 41 (22.8%) dentists as 11-20%; by 23 (12.8%) dentists as 51% and above; by 15 (8.3%) dentists as 0-5%; and 12 (6.7%) dentists as between 6-10%. Furthermore, the hypothesis of the study was confirmed with the finding that women were better at denture cleaning and denture wearers of advanced age could not clean their dentures adequately.
The method of brushing dentures with soap was determined to offer sufficient effectiveness in the elimination of bacterial plaque on the base plaque [25]. The standalone use of denture brushing was specified not to suffice for the denture wearers with advanced denture stomatitis and to require the additional brushing of soft tissues in contact with the denture [26]. The relevant literature points out to the common use of a toothbrush and toothpaste for denture cleaning among denture wearers [27-30]. In the present study, when the methods used by the denture wearers in denture cleaning are evaluated by frequency, it was determined that they most commonly washed their dentures in running water (47), followed by cleaning with toothpaste and a toothbrush (13) and cleaning with soap and a toothbrush (11). This conclusion is congruent with the aforementioned findings of the authors.
Denture cleaning tablets are produced for antimicrobial efficacy. Such effect is considered to result from the presence of hydrogen peroxide, peracetic acid, and oxygen radicals. Their content of surfactant provides for cleaning. They do not contain any abrasives. Producers of denture cleaning agents recommend that dentures be soaked in the solution at 40-50℃ for 15-20 minutes. However, some studies argue such application to offer inadequate cleaning and there is a need for further studies on the effects of overnight soaking on dentures and the antibacterial efficacy of such application [3].
In the present study, the use of denture cleaning tablets once a day overnight was recommended by 32 (17.8%) dentists, while 26 (14.4%) recommended such use for 15 minutes once a day, and 26 (14.4%) recommended such use for 15 minutes once a day in response to the question on the cleaning frequency and soaking duration with this method. One study evaluating Protefix denture cleaning agent reported that this agent was 100% effective on vegetative bacteria upon contact of 15 minutes. However, an antimicrobial efficacy between 88 and 95% in acrylic samples against B. subtilis, niger ATCC 9372. On the other hand, the percentage of such efficacy in Molloplat-B soft lining material was reported as 69% [13].
In a study conducted on geriatric denture wearers, denture cleaning tablets (Denture Brite, Polident, and Efferdent) were indicated not to offer any superior effectiveness against Candida spp. and S mutans strains [31]. In another study, the use of denture tablets was compared with mechanical cleaning, and it was reported that more effective results were obtained with the combination of these two methods [15]. Mechanical cleaning and chemical cleaning materials should be used together in order to ensure effective disinfection of dentures. The most effective of these chemical agents is sodium hypochlorite solutions diluted in different concentrations [2, 12, 32]. Sodium hypochlorite, although cheap and easily obtainable, is not preferred on grounds that it causes halitosis, has an unpleasant taste, leads to bleaching in dentures [33], and results in corrosion and tarnishing on removable dentures with a metallic base [1].
One study examining the effectiveness on four different disinfecting agents (5% Deconex, 3.5% Savlex, 2% and 5.25% diluted sodium hypochlorite) on soft lining materials (Tempo, Immediate, Flexacryl, Pure, and Ufi Gel P) reported similar effectiveness in reducing the number of microorganisms present and indicated that increased soaking durations would improve such effectiveness [13, 34]. Although sodium hypochlorite is a broadspectrum disinfectant in killing microorganisms, its effectiveness decreases in the presence of organic matter on the prosthesis [2]. The relevant literature established that sodium hypochlorite offered complete disinfection in as short a duration as 4 minutes [2], while Clorox, a sodium hypochlorite solution of 5.25%, was an effective bactericidal and fungicidal against all species of microorganisms when used for 5 minutes [24].
It has been reported that 0.2% chlorhexidine gluconate has sufficient efficacy on Candida Albicans and contributes to the healing of tissues [22]. Dentures kept in a diluted solution of chlorhexidine gluconate for only a few minutes were identified to enjoy a significant decrease in bacterial plaque and an improvement in soft tissue improvement with prosthetic stomatitis, whereas the condition relapsed at the end of such treatment [35]. The use of dentures upon being kept in a chlorhexidine solution of 0,2% did lead to improvements in denture stomatitis of the mucosa, but with an eventual result of severe discoloration [22, 35]. In the present study, 158 (87.8%) dentists did not recommend soaking in diluted bleach, while 15 (8.3%) dentists recommended keeping dentures in diluted beach for longer than 30 minutes once a week; 3 (1.7%) dentists for 6 minutes once a week; 2 (1.1%) dentists for 6 minutes once a day; 1 dentist (0.6%) for 10 minutes once a week; and 15 (58.3%) dentists marked other options. In one study, the condition of palatal mucosa in 58 of the denture wearers who used total prosthesis and developed stomatitis was compared with that of a control group with normal healthy palatal mucosa, and it was determined that denture cleaning fared much better in the control group than the group with stomatitis [36].
In the present study, the ratio of the denture wearers with knowledge of denture cleaning was indicated by 53 (29.4%) dentists as 6-10%; by 41 (22.8%) dentists as 11-20%; by 39 (21.7%) dentists as 29-50%; by 38 (21.1%) dentists as 0-5%; and by 9 (5.0%) dentists as 51% and above. The literature offers only a limited number of studies concerning denture cleaning techniques [22, 37] and dentists’ recommendations on the matter [22]. A correlation has been reported between the information provided to the denture wearers and the development of relevant conditions [38]. The literature points out to the claim that denture wearers are not informed on the matter by their physicians [39] and they need to apply a variety of methods to clean their dentures [40, 41].
In this study, 179 (99.4%) dentists who responded to the survey stated that they informed their patients about denture care, while 1 (0.6%) stated that they did not inform their patients as such; while in response to the question as to the stages at which denture wearers should be informed on denture cleaning, 159 (88.3%) dentists pointed out to the handover of the dentures, 20 (11,1) dentists at the initial examination, and 1 (0.6%) dentist at follow-up sessions. Toothpaste is a material that can be easily obtained and considered cheap. However, they are produced for the cleaning of natural teeth and thus contain abrasives. Acrylic resin dentures are softer than natural teeth. They are known to be exposed to abrasion on the surface, which leads to the formation of areas susceptible to bacterial attachment [42]. Kiesow, et al. [43], mentioned such abrasive effect in their study on the effects of material fit on treatment duration and efficacy in antimicrobial cleaning. Toothpaste is designed for antimicrobial efficacy. Toothpaste brings about its primary effects in mechanically assisted elimination of plaque [44], release of fluoride [45] resulting in protective and preventive action, and protection against gingivitis, whereas its secondary effect of antimicrobial action is considered to remain at a trace amount along with the addition of certain agents (sodium lauryl (dodecyl) sulphate in combination with triclosan, stannous fluoride, and zinc salt) [30].
Toothpaste containing calcium carbonate is rather abrasive as it does not dissolve with water. On the other hand, toothpaste free of sodium bicarbonate is not abrasive at all. The use of an unsuitable brush will create an abrasive effect on the base [22]. A relevant study indicated that immersion cleaning agents bring about a more abrasive effect on the surface roughness of the acrylic base when compared to pastes [46]. Certain studies reported that sodium hypochlorite and denture cleaning tablets containing alkaline peroxide caused bleaching on the acrylic surface [22, 33, 47]. However, immersion in a 1% sodium hypochlorite solution was reported not to lead to any discoloration on the acrylic base or teeth [48]. It was also reported that the use of microwave energy created non-negligible contraction and expansion on the acrylic surface upon 10-minute exposure at 604 W, while such changes might be considered negligible upon 6-minute exposure at 331 W [49].
In the present study, when the products recommended as disinfectants are evaluated according to their negative effects on the acrylic base, teeth, and mucosa, 123 dentists reported that denture cleaning tablets had no negative effect, while 56 dentists reported that soaking in diluted bleach caused mucosal irritation.
Women were identified to provide more effective denture cleaning when compared to men. In the present study, while 93 (51.7%) dentists think that women are better at denture cleaning, 86 (47.8%) dentists think that it is not related to gender, and 1 (0.6%) dentist thinks that men are better at denture cleaning. Despite myriad studies examining the efficacy of such methods, the determination of the preferences of physicians and the level of awareness of denture wearers on the matter is of paramount importance in shedding light on future studies.
Conclusion
There is no consensus among dentists on denture cleaning. The systemic lack of data plays an important role in the failure to secure such consensus. The data obtained through the present study may offer guidance to securing a consensus among physicians on this matter. Furthermore, a heightened level of awareness may be reached on the importance of denture cleaning.
Acknowledgement
The authors would like to thank to all the dentists who answered the survey questions.
Conflict of Interest
The authors declare no conflict of interest.
References
- Augsburger RH, Elahi JM (1982) Evaluation of seven proprietary denture cleansers. J Prosthet Dent 47(4): 356-359.
- Bell J, Brockmann SL, Feil P, Sackuvich DA (1989) The effectiveness of two disinfectants on denture base acrylic resin with an organic load. The Journal of Prosthetic Dentistry 61(5): 580-583.
- Dikbaş İ, Köksal T (2005) Materials and Methods Used for Denture Cleaning and Disinfecting (Materials and methods used in cleaning and disinfection of removable dentures). Hacettepe Dişhek Fak Derg 29: 16-27.
- Assery M, Sugrue PC, Graser GN, Eisenberg AD (1992) Control of microbial contamination with commercially available cleaning solutions. J Prosthet Dent 67(2): 275-277.
- Drake D, Wells J, Ettinger R (1992) Efficacy of denture cleansing agents in an in vitro bacteria-yeast colonization model. Int J Prosthodont 5(3): 214-220.
- Abelson DC (1981) Denture plaque and denture cleansers. J Prosthet Dent 45(4): 376-379.
- Eriksen HM, Nordbø H (1978) Extrinsic discoloration of teeth. J Clin Periodontol 5(4): 229-236.
- Theilade J (1975) Plaque development on the oral cavity. Community Dent Oral Epidemiol 3: 115.
- Moore T, Smith D, Kenny G (1984) Sanitization of dentures by several denture hygiene methods. J Prosthet Dent 52(2): 158-163.
- Yeşil Duymuş Z, Fındık Aydıner S (2020) Hareketli Protezlerin Temizlenmesinde Kullanılan Materyal ve Yöntemler In: Kesim B (Ed.), Güncel Protetik Diş Tedavisi Çalışmaları 12: 147-160.
- Tamamoto M, Hamada T, Miyake Y, Suginaka H (1985) Ability of enzymes to remove Candida. J Prosthet Dent 53(2): 214-216.
- Akgök V, Güzel K, and Gül K (1993) Isolation of bacteria from dentures and the effect of various disinfectant substances on these bacteria. Dentistry Magazine 17: 242-8.
- KS Akşit, Y Nakipoğlu, G Mandalı, G Günel, B Gürler (2015) An investigation of the bacteriological activity of denture cleansing products (Investigation of the bacteriological activities of dental prosthesis cleaning products). Journal of Atatürk University Faculty of Dentistry 25(1): 47-53.
- Akşit KS, Ünalan F, Gürler B, Beka H, Dikbaş İ (1995) Evaluation of various methods used in the disinfection of acrylic prophylactic base materials and Molloplast-B. Ankem Derg 9: 79-84.
- Oliveira Paranhos HF, Silva Lovato CH, De Souza RF, Cruz PC, De Freitas Pontes KM (2009) Effect of three methods for cleaning dentures on biofilms formed in vitro on acrylic resin. J Prosthodont 18(5): 427-431.
- Pavarina AC, Pizzolitto AC, Machado AL, Vergani CE, Giampaolo ET (2003) An infection control protocol: effectiveness of immersion solutions to reduce the microbial growth on dental prostheses. J Oral Rehabil 30(5): 532-536.
- Rohrer MD and Bulard RA (1985) Microwave sterilization. Journal of the American Dental Association 110(2): 194-198.
- Murray I, McCabe J, and Storer R (1986) The relationship between the abrasivity and cleaning power of the dentifrice-type denture cleaners. Br Dent J 161(6): 205-208.
- Webb BC, Thomas CJ, Harty DW, Willcox MD (1998) Effectiveness of two methods of denture sterilization. J Oral Rehabil 25(6): 416-423.
- Ghalichebaf M, Graser GN, Zander HA (1982) The efficacy of denture-cleansing agents. Journal of Prosthetic Dentistry 48(5): 515-520.
- Raab FJ, Taylor CA, Bucher JA, Mann BL (1991) Scanning electron microscopic examination of ultrasonic and effervescent methods of surface contaminant removal from complete dentures. J Prosthet Dent 65(2): 255-258.
- Budtz Jørgensen E (1979) Materials and methods for cleaning dentures. J Prosthet Dent 42(6): 619-623.
- Da Silva FC, Kimpara ET, Mancini MNG, Balducci I, Jorge AOC, et al. (2008) Effectiveness of six different disinfectants on removing five microbial species and effects on the topographic characteristics of acrylic resin. J Prosthodont 17(8): 627-633.
- Rudd RW, Senia ES, McCleskey FK, Adams ED (1984) Sterilization of complete dentures with sodium hypochlorite. J Prosthet Dent 51(3): 318-321.
- Hasanreisoğlu U, Aydın K (1984) Comparison of profitez cleansing systems. AU Faculty of Dentistry Journal 11: 189-207.
- Chamberlain BB, Bernier SH, Bloem TJ, Razzoog ME (1985) Denture plaque control and inflammation in the edentulous patient. J Prosthet Dent 54(1): 78-81.
- Apratim A, Shah SS, Sinha M, Agrawal M, Chhaparia N, et al. (2013) Denture hygiene habits among elderly patients wearing complete dentures. J Contemp Dent Pract14(6): 1161.
- Baran I, Nalçacı R (2009) Self-reported denture hygiene habits and oral tissue conditions of complete denture wearers. Arch Gerontol Geriatr 49(2): 237-241.
- Barreiro DM, Scheid PA, May LG, Unfer B, Braun KO (2009) Evaluation of procedures employed for the maintenance of removable dentures in elderly individuals. Oral Health Prev Dent 7(3): 243-249.
- Axe AS, Varghese R, Bosma M, Kitson N, Bradshaw DJ (2016) Dental health professional recommendation and consumer habits in denture cleansing. J Prosthet Dent 115(2): 183-188.
- Gornitsky M, ParadisI I, Landaverde G, Malo AM, Velly AM (2002) A clinical and microbiological evaluation of denture cleansers for geriatric patients in long-term care institutions. J Can Dent Assoc 68(1): 39-45.
- Lambert JP, Kolstad R (1986) Effect of a benzoic acid-detergent germicide on denture-borne Candida albicans. The Journal of prosthetic dentistry 55(6): 699-700.
- Ünlü A, Altay OT, and Sahmali S (1996) The role of denture cleansers on the whitening of acrylic resins. Int J Prosthodont 9(3): 266-70.
- Yilmaz H, Aydin C, Bal BT, Ozçelik B (2005) Effects of disinfectants on resilient denture-lining materials contaminated with Staphylococcus aureus, Streptococcus sobrinus, and Candida albicans. Quintessence Int 36(5): 373-381.
- Olsen I (1975) Relapse tendency and removal of acquired discolourations in long-term denture disinfection with chlorhexidine. Acta Odontologica Scandinavica 33(2): 111-114.
- Budtz Jörgensen E, Löe H (1972) Chlorhexidine as a denture disinfectant in the treatment of denture stomatitis. Scand J Dent Res 80(6): 457-464.
- Jagger R (2009) Lack of evidence about the effectiveness of the different denture cleaning methods. Evid Based Dent 10(4): 109-109.
- Marchini L, Tamashiro E, Nascimento DF, Cunha VP (2004) Self‐reported denture hygiene of a sample of edentulous attendees at a University dental clinic and the relationship to the condition of the oral tissues. Gerodontology 21(4): 226-228.
- Peracini A, Andrade IM, Paranhos Hde F, Silva CH, de Souza RF (2010) Behaviors and hygiene habits of complete denture wearers. Braz Dent J 21(3): 247-252.
- Jagger D, Harrison A (1995) Denture cleansing--the best approach. Br Dent J 178(11): 413-417.
- Maeda Y, Idoji S, Mori T, Naito K, Emura I, et al. (1990) Problems of denture wearers regarding denture cleaning. The Journal of Osaka University Dental School 30: 120-124.
- Verran J, Jackson S, Coulthwaite L, Scallan A, Loewy Z, et al. (2014) The effect of dentifrice abrasion on denture topography and the subsequent retention of microorganisms on abraded surfaces. J Prosthet Dent 112(6): 1513-1522.
- Kiesow A, Sarembe S, Pizzey RL, Axe AS, Bradshaw DJ (2016) Material compatibility and antimicrobial activity of consumer products commonly used to clean dentures. J Prosthet Dent 115(2): 189-198. e8.
- Wong MC, Clarkson J, Glenny AM, Lo EC, Marinho VC, et al. (2011) Cochrane reviews on the benefits/risks of fluoride toothpastes. J Dent Res 90(5): 573-579.
- Horowitz AM, Suomi JD, Peterson JK, Lyman BA (1977) Effects of supervised daily dental plaque removal by children: II. 24 months' results. J Public Health Dent 37(3): 180-188.
- Harrison Z, Johnson A, Douglas CW (2004) An in vitro study into the effect of a limited range of denture cleaners on surface roughness and removal of Candida albicans from conventional heat‐cured acrylic resin denture base material. J Oral Rehabil 31(5): 460-467.
- Robinson JG, McCabe JF, Storer R (1985) The whitening of acrylic dentures: the role of denture cleansers. British dental journal 159(8): 247-250.
- McNeme SJ, von Gonten AS, Woolsey GD (1991) Effects of laboratory disinfecting agents on color stability of denture acrylic resins. The Journal of prosthetic dentistry 66(1): 132-136.
- Thomas C, Webb B (1995) Microwaving of acrylic resin dentures. Eur J Prosthodont Restor Dent 3(4): 179-182.
-
Zeynep Yeşil Duymuş, Sebahat Findik Aydiner. Evaluation of Methods of Denture Cleaning. On J Dent & Oral Health. 4(3): 2021. OJDOH.MS.ID.000590.
-
Removable dentures, Oral health, Denture plaque, Oral hygiene, Denture wearers, Toothpaste, Zirconium, Dentists, Denture cleaning.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






