 Case Report
Case Report
Dissecting Subperiosteal Abscess After Surgical Removal of Mandibular Third Molar
Myint Wei1 and Haydar Majeed Mahdey2*
1Department of Oral Surgery, Senior Lecturer, SEGi University, Malaysia
2Department of Oral Surgery, Lecturer, SEGi University, Malaysia
Haydar Majeed Mahdey, Department of Oral Surgery, Lecturer, Faculty of dentistry, SEGi University, Malaysia.
Received Date: December 03, 2018; Published Date: January 23, 2019
Abstract
Impacted Third molar surgery is one of the most common procedures performed in oral and maxillofacial surgery offices. Dissecting subperiosteal abscess, a certain type of subperiosteal infection after surgical removal of mandibular third molar, may occur several weeks after an apparently uneventful healing of a mandibular third molar wound. It can be managed and prevent further complication if diagnosed early and give proper treatment.
Introduction
Impacted Third molar surgery is one of the most common
procedures performed in oral and maxillofacial surgery offices.1-6
Impaction is defined as failure of teeth to erupt into the dental arch
within the expected time [1,2]. The reasons for tooth impaction
include several factors subdivided into a local and general factor
such as position and size of adjacent teeth, dense overlying bone,
excessive soft tissue or a genetic abnormality including abnormal
eruption path, dental arch length and space in which to erupt [3-
6] Nevertheless, this procedure requires accurate planning and
surgical skills. With surgical procedures in general, complications
can always arise. The reported frequencies of complications after
third molar removal are reported between 2.6 percent and 30.9
percent. The spectrum of complications ranges from minor expected
sequelae of post-operative pain and swelling, to permanent nerve
damage, mandibular fractures, and life-threatening infections. A
certain type of subperiosteal infection may occur several weeks
after an apparently uneventful healing of a mandibular third
molar wound. Dissecting subperiosteal abscess, a certain type of
subperiosteal infection after surgical removal of mandibular third
molar, may occur several weeks after an apparently uneventful
healing of a mandibular third molar wound. This may present
itself primarily as an indurated swelling in the mucoperiosteal
tissue as far forward as the first molar or second bicuspid. It
may become progressively edematous and indurated and finally
develop into a fluctuant, palpable, and visible subperiosteal abscess
that has migrated from the original third molar wound beneath
the periosteum to the point of fluctuance. When the diagnosis is
made, antibiotic therapy should be initiated, and as soon as the
fluctuance is palpable, the abscess should be incised and drained.
This condition may be externally visible and palpable as a swelling
of the cheek in this region./p>
Objective
Objective of this report is to awareness of the incidence of this subperiosteal infection after surgery and prevent from the further complications secondary space odontogenic infection.
Case Report
Yee Pei Ying 20yrs (F) from 7060 Seremban, Negeri Sembilam, Malaysia came with the complaint of pain at the right lower region for 1week, to oral health clinic of SEGi university KD.
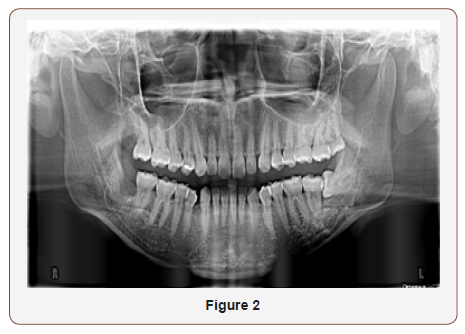
On examination extra orally, no swelling of the face and no regional lymph node involvement. Intraorally generalized marginal gingivitis with supragingival calculus deposition was seen. Scaling was done on the date of 1/4/2014. She was sent to oral surgeon for assessment of last molar teeth. 4/4/2014 OPG was taken. Review of the OPG, PG class IIB mesio-angular 48, 38 distally inclined 18 and 28. So decided to do surgical removal of 48 along with 18 on the date of 30/4/2014 (Figure 1).

Surgical Procedure
Preoperatively Amoxicillin 1G+ Metronidazole200mg +Paracetamol 1G ,1hour before surgery was given. 48 was anaesthetized by given Inferior dental block, using lignocaine2% +Adrenaline 1:80,000-4 cartridges. Modified triangular flap was made from the mesial of 47 to 48 distal. Flap was reflected from the area and bone around 48 was removed with dental surgical drill using burs under ample amount of water spray. Also sectioned the tooth48 into 3 pieces using round and fissure burs under water spray. Elevate out the tooth in 3 pieces. Toilet the operated area with antiseptic solution (chlorhexidine 0.12%) and 0.09% namal saline after smoothening the bone edges of the 48 area. Flap was repositioned and sutured with 3/0vicryl in 5 interrupted sutures.
Under LA, 18 was also elevate out and sutured the area with 3/0 vicryl suture. The areas were put pressure pack to stop bleeding.
Continued the medication Amoxicillin 500mg +Flagyl (metronidazole)200mg TDS for 5days along with analgesic (Ponstan 500mg+Paracetamol 500mg).
Let the mouth to wash with hexipro (chlorhexidine 0.12%) after 24 hours of operation. Review on 9/5/2014, no pain, no swelling was seen. Suture were removed on that day.
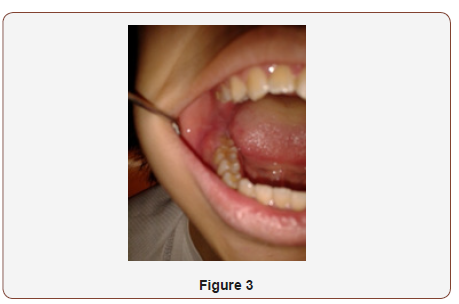
On The date of 3/6/2014 patient complaint of swelling and pain around the post-operative area 48. On examination right side of the face was swollen extra orally. Intra orally swelling at 48 area of buccal site to mesial of 47 (Figures 2 & 3).
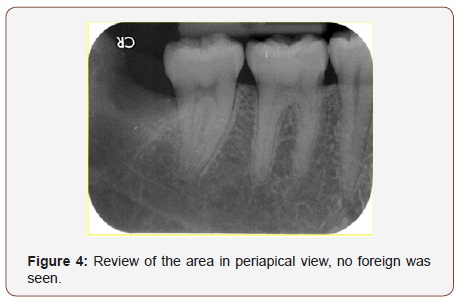
So did assessment of the area by taking Digital Peri-apical view of the 48,47 area (Figure 4). Review of the area in periapical view, no foreign was seen.
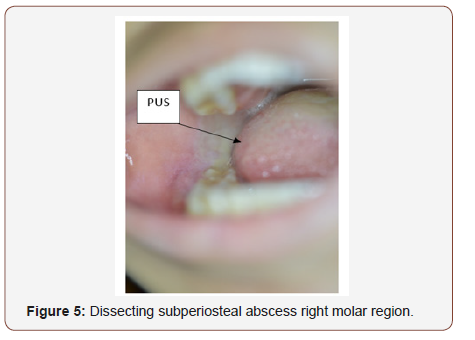
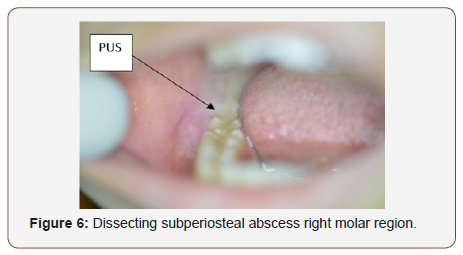
Intraorally, spontaneous pus discharged from the distal of 47 on pressure under topical anesthesia (Figures 5 & 6).
Diagnosed as “Dissecting subperiosteal abscess right molar region”
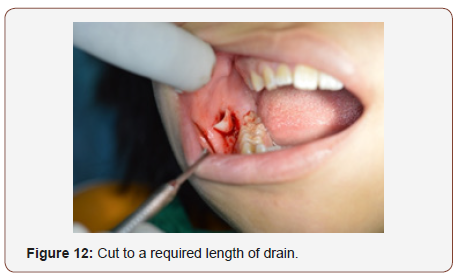
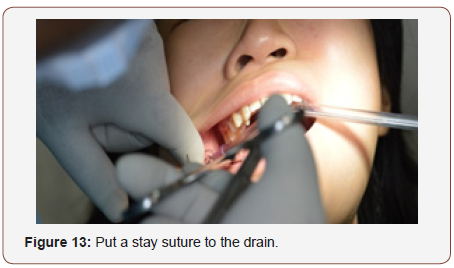
Decided to give incision and drainage under topical anesthesia along with antibiotic therapeutic dosage (Figures 7-14).






After 3 days I &D area and drain was checked.
No more pus discharging from the drain. So, decided to remove the drain.
After removal of drain a small clog pus came out to the orifice of the drain. So, removed that pus clog and let the remaining exudates drained out (Figure 15).
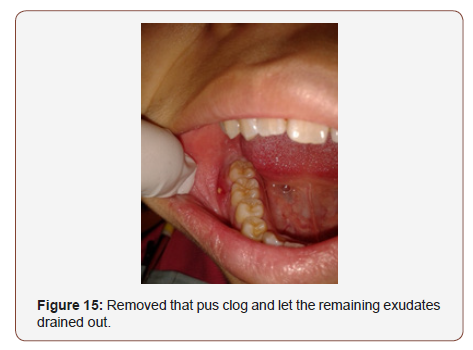
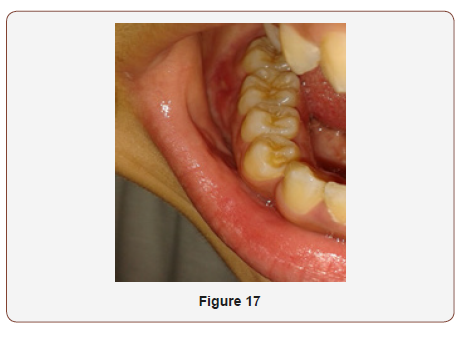
Prescribed to continue antibiotic for another 3 days and antiseptic mouth wash for another two weeks. After 2 weeks, the following is the follow up and the area was healed uneventfully (Figures 16&17).

Discussion
A certain type of subperiosteal infection may occur several weeks after an apparently uneventful healing of a mandibular third molar wound. This may present itself primarily as an indurated swelling in the mucoperiosteal tissue as far forward as the first molar or second bicuspid. It may become progressively edematous and indurated and finally develop into a fluctuant, palpable, and visible subperiosteal abscess that has migrated from the original third molar wound beneath the periosteum to the point of fluctuance [7-9]. When the diagnosis is made, antibiotic therapy should be initiated, and as soon as the fluctuance is palpable, the abscess should be incised and drained. This condition may be externally visible and palpable as a swelling of the cheek in this region. The drainage incision should start from the point of origin, which is the third molar region deep in the buccal vestibule and extend anteriorly to the point of fluctuance. The incision should be made through the mucoperiosteal down to the bone. Tissues on either side of the incision should then be expanded with a hemostat to pus drained out from the under of periosteum, put rubber drain permitting the purulent material to drain out around it. It should be observed at 48-hour intervals. If no more purulent material comes out, the rubber drain should remove. After that the wound will heal by granulating from the depth of the wound. Early diagnosis and drainage of the area with appropriate antibiotic can prevent further spread of infection and promote of the healing.
Acknowledgement
None.
Conflict of Interest
The author deny any conflicts of interest related to this study.
References
- Jojić B, Perović JV (1990) Oralna hirurgija (4th edn). Naučna knjiga, Serbia.
- James Hupp, Edward Ellis, Myron Tucker (2008) Contemporary oral and maxillofacial surgery (5th edn). Mosby Elsevier, St. Louis, US, pp. 1-718.
- Alling CC, Helfrick JF, Alling RD (1993) Impacted Teeth. European Journal of Orthodontics 18(3): 310.
- Gustav O Kruger (1979) Textbook of Oral and Maxillofacial Surgery 5th edn. In: ed B John Melloni, Chapter11: Acute infections of the oral cavity. The CV Mosby Company, St Louis, Toronto, London, pp. 6.
- Kim IK, Kim JR, Jang KS, Moon YS, Park SW (2007) Orbital abscess from an odontogenic infection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103(1): e1-e6.
- Kim JC, Choi SS, Wang SJ, Kim SG (2006) Minor complications after mandibular third molar surgery: type, incidence, and possible prevention. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102(2): e4-e11.
- Sakkas N, Schoen R, Schmelzeisen R (2007) Orbital abscess after extraction of a maxillary wisdom tooth. Br J Oral Maxillofac Surg 45(3): 245-246.
- Muñoz-Guerra MF, González-García R, Capote AL, Escorial V, Gías LN (2006) Subperiosteal abscess of the orbit: an unusual complication of the third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102(5): e9-e13.
- de Boer MP, Raghoebar GM, Stegenga B, Schoen PJ, Boering G(1995) Complications after mandibular third molar extraction. Quintessence Int 26(11): 779-84.
-
Myint Wei, Haydar Majeed Mahdey. Dissecting Subperiosteal Abscess After Surgical Removal of Mandibular Third Molar. On J Dent & Oral Health. 1(4): 2019. OJDOH.MS.ID.000518.
-
Oral surgery, Maxillofacial surgery, Dental arch, Adjacent teeth, Odontogenic infection, Dental health, Dental treatments, Tooth brushing, Teeth, Dental school, Ceramics, Gingivitis, Supragingival calculus
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






