 Research Article
Research Article
Bond Strength Between A Hard Chairside Reline and A Printed Denture Base Compared to A Conventional Heat Polymerized Denture Base: An In Vitro Study
Ghazal Pazooki1, Tian Fang Zhang2, Sara Palladino3, Diego Mantovani4 and Ghassan Al Dika5*
1Faculty of Dentistry, Laval University, Canada
2Faculty of Dentistry, Laval University, Canada
3Faculty of Science and Engineering, Laval University, Canada
4Faculty of Science and Engineering, Laval University, Canada
5Faculty of Dentistry, Laval University, Canada
Dr Ghassan Al Dika, Faculty of Dentistry, Laval University, 2420 Rue de la Terrasse, local 4519, G1V 0A6, Quebec, Quebec, Canada.
Received Date: June 20, 2022; Published Date: September 19, 2022
Abstract
Introduction: The aim of this study was to test the shear and tensile bond strengths (MPa) of a hard chairside reline to a 3D printed denture base and compare it to a conventional heat polymerized denture base.
Material and methods: Sixty (n=15/test) blocks (70mm x 9mm x 9mm) of a printed polymethyl methacrylate (P-PMMA) (DENTCA 3D Printed Dentures) were provided by the manufacturer, while sixty (n=15 per test) blocks (70mm x 9mm x 9mm) of thermopolymerizable polymethyl methacrylate (T-PMMA) (Diamond D. Keystone) were prepared. Three millimeters of hard liner (Tokuso-Tokuyama America Inc.) was applied between two blocks. All the tests were conducted with an INSTRON Universal Testing machine.
Results: Statistically significant differences were found in the bond strength for the shear (p<0.003) and the tensile (p<0.0001) tests between the materials. In both instances, the bond strength of the hard liner with the P-PMMA was weaker compared to the T-PMMA with 6.22MPa±0.78SE and 9.82MPa±0.78SE respectively in the shear test, and 3.61MPa±0.42SE and 6.68±0.42SE respectively in the tensile test. The force of rupture was also significantly lower in the P-PMMA 101.99MPa±12.04SE versus the T-PMMA with 143.64MPa±12.04SE during the shear test (p<0.021) and the tensile test (p<0.0002) with 360.96MPa±41.97SE versus 611.18MPa±41.97SE respectively.
Conclusion: In the context of this study, the bond between the hard liner and the printed polymethyl methacrylate was shown to be weaker when compared to the thermopolymerizable polymethyl methacrylate. Further investigation of the surface properties of CAD/CAM denture bases such as surface chemistry and the clinical impact of these results are suggested. As the use of CAD/CAM technology gains in popularity, more materials developed for traditional dentures should be studied for compatibility.
Keywords: CAD/CAM; Printed denture; Polymethyl methacrylate; Hard reline; Tensile bond strength; Shear bond strength
Abbreviations: CAD/CAM: Computer-aided design and computer-aided manufacturing; P-PMMA: Printed polymethyl methacrylate; T-PMMA: Thermopolymerizable polymethyl methacrylate; MPa: Megapascal; SE: Standard error
Introduction
Computer-aided design and computer-aided manufacturing (CAD/CAM) technology is increasingly used for different applications in dentistry such as fixed prostheses and more recently, removable dentures [1]. This is a promising avenue that could reduce the error accumulation in data collection and avoid the dimensional changes during the laboratory steps such as acrylic polymerization shrinkage, since the final product is printed or milled from prepolymerized blocks [2-4]. This newer approach is attractive for both clinicians and patients since it translates into two or three appointments completion, permits digital archiving, and demonstrates an improved denture base adaptation [1, 3, 5].
However, as the oral condition of patients evolves over time [6- 7], continuous residual ridge resorption may lead to denture failure and consequently, the removable dentures will require adjustments regardless of the selected approach [8]. Several methods exist to adapt the removable prosthesis to the gradual changes in residual alveolar ridge contours, thus avoiding the continuous substitution, and relining is one of them. In this study, we are particularly interested in chairside hard relining, a practice that may be indicated when a lack of retention, due to missing material (acrylic), is present in patients with stable oral conditions and no expected significant changes. If a denture was prepared with CAD/ CAM technology and relining was required, it would be crucial to ensure that the existing relining materials are compatible and can adequately be bonded to the denture base.
This study compares the shear and tensile bond strengths of a hard chairside reline material [9] (Tokuso-Tokuyama America Inc.) with printed polymethyl methacrylate (P-PMMA) (DENTCA 3D Printed Dentures) as used in the fabrication of prostheses with the CAD/CAM technique versus strength of the same relining material with the thermopolymerizable polymethyl methacrylate (T-PMMA) (Diamond D. Keystone) as used in the fabrication of prostheses with the conventional technique.
Materials and Methods
Preparation of the specimens
Sixty blocks of P-PMMA (70mm x 9mm x 9mm) were provided by DENTCA 3D Printed Dentures. Sixty blocks of T-PMMA (Diamond D. - Keystone Industries, USA) of equal dimensions to the P-PMMA blocks were prepared using the conventional method with the lost wax technique in a denture flask (Hanau, Whip Mix, USA) (Figure 1). The flasks were polymerized overnight according to the manufacturer’s recommendations in a 165℉ water bath for 10 hours.

The work surface of each block was unpolished with a carbide bur (H72E.11.060, Brasseler, USA). The adhesive was applied, and pairs of blocks were stabilized at 3mm distance from each other (Figure 2). The autopolymerizing hard denture liner (Tokuso-Tokuyama America Inc.) was prepared according to the manufacturer’s recommendations which is composed of a polyethyl methacylate acrylic (PEMA) powder and a β-methacryloyl oxyethyl propionate (MAOP) liquid. The relining material was then injected with a syringe between the two work surfaces and compacted with a spatula.
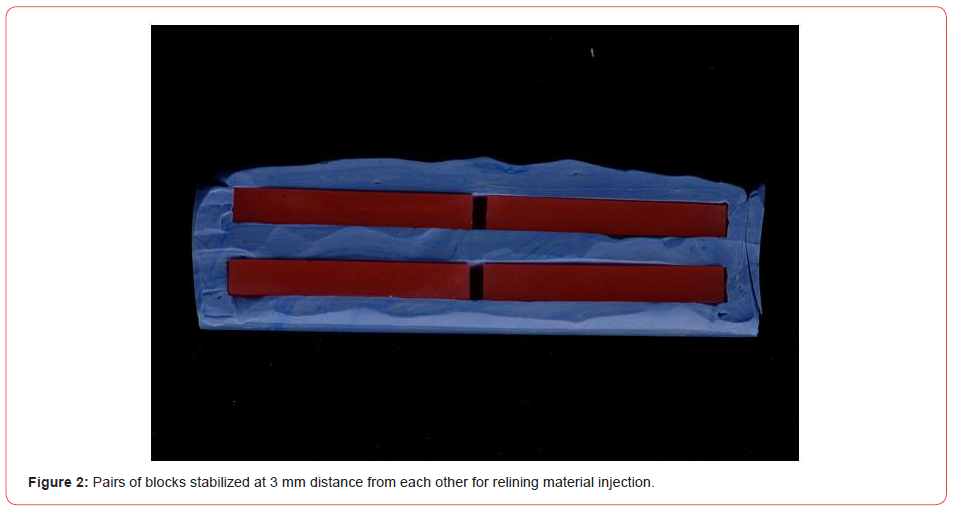
A total of sixty specimens were prepared and divided into four groups of 15 specimens each (Table 1). Each specimen is composed of two blocks of the same material (Figure 3). All the tests were conducted with an INSTRON Universal Testing machine (Model 5944, Instron Corporation, Norwood, MA, USA).

Table 1: Test groups.
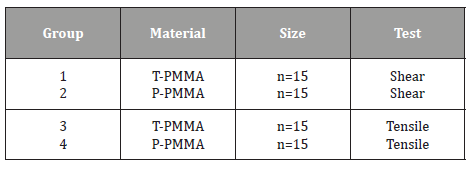
Abbreviations: P-PMMA: Printed polymethyl methacrylate; T-PMMA: Thermopolymerizable polymethyl methacrylate.
Shear stress and tensile strength tests
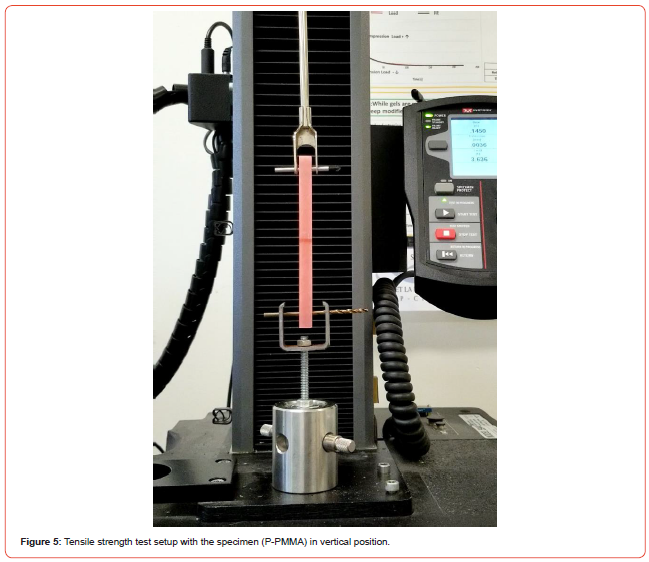
For the shear stress test, the uniaxial force was applied vertically from the top on a horizontally placed specimen, at 1cm distance from the fixed section, with a head speed of 1mm/min until failure (Figure 4). Load and extension, in Newton and mm respectively, were recorded with an acquisition rate of 100ms. For the tensile strength test, the uniaxial force was applied was applied vertically from the top on a vertically mounted specimen with a head speed of 5mm/min until failure (Figure 5). Load and extension, in Newton and mm respectively, were recorded with an acquisition rate of 100ms.

Fracture analysis
For all the tested specimens, the fracture was considered adhesive when failure occurred between the relining material and the acrylic resin, cohesive when a fracture was inside the relining material, or mixed when both occurrences were observed in the same fracture. The mode of fracture was determined visually.
Statistical analysis
The statistical package SAS software, version 9.4 (SAS Institute Inc., Cary NC) was used for all the analyzed data with respect to the different tests. The average tensile and shear strengths and standard deviation (SD) were calculated for each group. Student’s T test was used to analyze the statistical difference among the tested groups with a power of 80% and a significance threshold of 5%.
Results
Shear stress test
For shear bond strength, P-PMMA specimens exhibited significantly lower (p<0.003) mean values compared to the conventional specimens with a mean and standard error of 6.22MPa±0.78SE versus 9.82MPa±0.78SE from the T-PMMA specimens (Table 2). The force at rupture of P-PMMA specimens were also significantly lower (p<0.02) than those of the T-PMMA specimens with 143.64MPa±12.04SE and 101.99MPa±12.04SE respectively (Table 3). Fisher’s Exact test was used to compare the proportion of fractures of each type according to the group. There was a significant difference (p<0.006) with 100% adhesive fracture rate for the P-PMMA method against 53% in the T-PMMA (Table 4) where the rest was mixed.
Table 2: Shear bond strength of specimens.
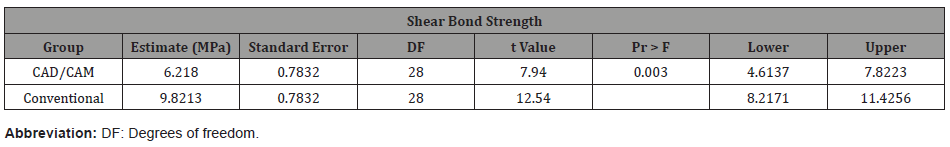
Table 3: Force of rupture of specimens for shear test.
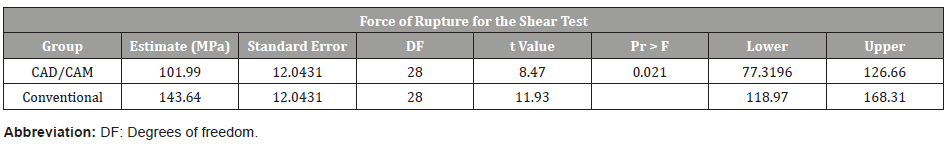
Table 4: Type of fracture of specimens for shear test.
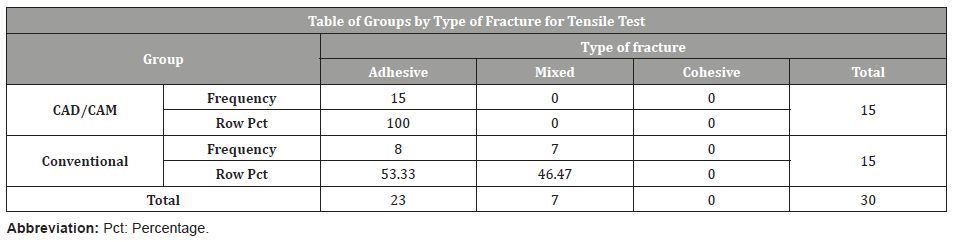
Tensile stress test
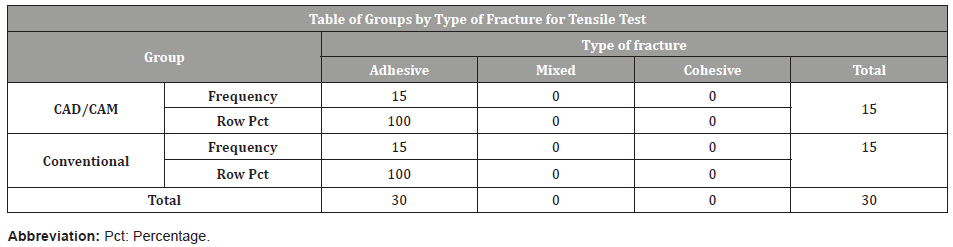
For the tensile bond strength, the adhesive strength of P-PMMA was found to be significantly lower (p<0.0001) than that of the T-PMMA with 3.61MPa±0.42SE and 6.68±0.42SE respectively (Table 5). The breaking force of the P-PMMA specimens were significantly lower (p < 0.0002) than those of the T-PMMA with 380.96MPa±41.97SE versus 611.18MPa±41.97SE respectively (Table 6). The Fisher analysis was not done for the fractures caused by tensile stress, since all the fractures in both trial groups were adhesive (Table 7).
Table 5: Tensile bond strength of specimens.
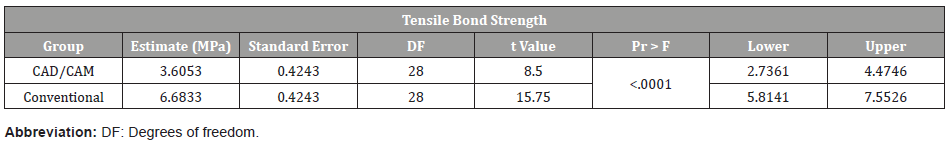
Table 6: Force of rupture for tensile test.
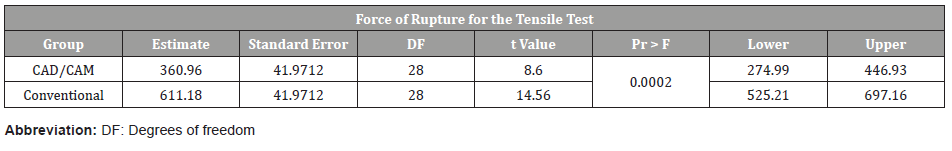
Table 7: Type of fracture of specimens for tensile test.
Discussion
The bond strength between a denture base and its relining material is used to indicate the durability and failure rate of the liner [10]. Shear and tensile stress tests are common strategies for the evaluation of the bond between denture bases and liners in literature [8, 11-14], and thus chosen for this study. The bonding between the liner and denture base is mainly provided by the diffusion, the penetration, and the polymerization of the reline monomers across the interface, thus forming interpenetrating polymer networks [15]. A recent study indicates a reduction of monomer content on the surface of CAD/CAM denture bases due to its method of preparation [16]. It is the same release of residual methyl methacrylate monomer (MMA) that affects the dimensional stability of conventional dentures. Although this presents many advantages clinically, like restrict polymerization shrinkage, enhanced mechanical properties, and decrease surface deterioration, it can also create a weaker bond when the application of a relining material is needed, since the interpenetration will not be optimal. However, this still requires more investigation. As surface finishing, chemical composition, topography, and roughness have been suggested to influence the adhesion between the acrylic and the relining material [17], the surface properties of the selected acrylics could explain the lower shear and tensile bond strengths of the CAD/CAM samples compared to the conventional ones [15, 18, 19]. In order to validate this hypothesis, a surface analysis should be included in future studies including the use of X-ray Photoelectron Spectroscopy (XPS) [20] for the surface chemical composition and Atomic Force Microscopy (AFM) [21] for the surface topography and roughness.
Since this study is preliminary, the used methodology lacks in recreating the patient’s mouth environment. To conduct the tests in a physiologically relevant ambient, part of the samples could be subjected to water immersion or thermocycling to stimulate water aging [8] and the results could then be compared to untreated control samples. Immersion of resin liners in water results in water absorption between the polymeric chains, which forces them apart and decreases bonding between the surfaces, thus providing more clinically accurate results [13, 22, 23].
Conclusion
Within the limitations of this in vitro study, our results suggest that the bond between the printed polymethyl methacrylate denture base and the hard liner is weaker when compared to the bond of thermopolymerizable polymethyl methacrylate denture base and the hard liner. More research is needed to study the properties of CAD/CAM denture bases (such as surface finishing, chemical composition, topography, and roughness) and to understand the clinical impact of these results.
Acknowledgement
The authors would like to thank Manon Clavette, from the Faculty of Dentistry at Laval University, for her participation and her guidance in the preparation of the specimens. They would also like to thank Bernard Drouin from the lab for Biomaterials and Bioengineering, at the Faculty of Science and Engineering at Laval University, for their participation, assistance and reportings.
Conflict of interest
No Conflict of Interest.
References
- Goodacre CJ, Garbacea A, Naylor WP, Daher T, Marchack CB, et al. (2012) CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent 107(1): 34-46.
- Steinmassl O, Dumfahrt H, Grunert I, Steinmassl PA (2018) CAD/CAM produces dentures with improved fit. Clin Oral Invest 22(8): 2829-2835.
- Bilgin MS, Baytaroğlu EN, Erdem A, Dilber E (2016) A review of computer-aided design/computer-aided manufacture techniques for removable denture fabrication. Eur J Dent 10(2): 286-291.
- Janeva NM, Kovacevska G, Elencevski S, Panchevska S, Mijoska A, et al. (2018) Advantages of CAD/CAM versus Conventional Complete Dentures-A Review. Maced J Med Sci 6(8): 1498-1502.
- Goodacre BJ, Goodacre CJ, Baba NZ, Kattadiyil MT (2016) Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J Prosthet Dent 116(2): 249-256.
- Klemetti E (1996) A review of residual ridge resorption and bone density. J Prosthet Dent 75(5): 512-514.
- Tallgren A (2003) The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent 89(5): 427-435.
- Choi JE, Ng TE, Leong CKY, Kim H, Li P, et al. (2018) Adhesive evaluation of three types of resilient denture liners bonded to heat-polymerized, autopolymerized, or CAD-CAM acrylic resin denture bases. J Prosthet Dent 120(5): 699-705.
- Matsumura H, Tanoue N, Kawasaki K, Atsuta M (2001) Clinical evaluation of a chemically cured hard denture relining material. J Oral Rehabil 28 (7): 640-644.
- Ozdemir, H, Ozdogan, A (2018) Bond strength of resilient lining materials to denture base resin: a systematic review and meta-analysis: bond strength of resilient lining to denture base. J Prosthodont 27(9): 828-841.
- Mutluay MM, Ruyter IE (2005) Evaluation of adhesion of chairside hard relining materials to denture base polymers. J Prosthet Dent 94(5): 445-452.
- Surapaneni H, Ariga P, Haribabu R, Ravi Shankar Y, Kumar VH, et al. (2013) Comparative Evaluation of Tensile Bond Strength between Silicon Soft Liners and Processed Denture Base Resin Conditioned by Three Modes of Surface Treatment: An Invitro Study. J Indian Prosthodont Soc 13(3): 274-280.
- Azevedo A, Machado AL, Giampaolo ET, Pavarina AC, Vergani CE (2007) The Effect of Water Immersion on the Shear Bond Strength Between Chairside Reline and Denture Base Acrylic Resins. J Prosthodont 16(4): 255-262.
- Leles CR, Machado AL, Vergani CE, Giampaolo ET, Pavarina AC (2001) Bonding strength between a hard chairside reline resin and a denture base material as influenced by surface treatment. J Oral Rehabil 28(12): 1153-1157.
- Steinmassl PA, Wiedemair V, Huck C, Klaunzer F, Steinmassl O, et al. (2016) Do CAD/CAM dentures really release less monomer than conventional dentures? Clin Oral Investig 21(5): 1697-1705.
- Ayman AD (2017) The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins. Electron Physician 9(7): 4766-4772.
- Al‐Dwairi ZN, Tahboub KY, Baba NZ, Goodacre CJ (2018) A Comparison of the Flexural and Impact Strengths and Flexural Modulus of CAD/CAM and Conventional Heat‐Cured Polymethyl Methacrylate (PMMA). J Prosthodont 29(4): 341-349.
- Al‐Dwairi ZN, Tahboub KY, Baba NZ, Goodacre CJ, Özcan M (2019) A Comparison of the Surface Properties of CAD/CAM and Conventional Polymethylmethacrylate (PMMA). J Prosthodont 28(4): 452-457.
- Engler ML, Güth JF, Keul C, Erdelt K, Edelhoff D, et al. (2019) Residual monomer elution from different conventional and CAD/CAM dental polymers during artificial aging. Clin Oral Invest 24(1): 277-284.
- Heide P (2012) X-ray photoelectron spectroscopy: an introduction to principles and practices. Wiley, Hoboken, NJ, USA.
- Haugstad G (2012) Atomic force microscopy: understanding basic modes and advanced applications. Princeton University Press, Princeton, NJ, USA.
- Khaledi AAR, Fatemi FS, Vojdani M, Mohammadi S (2019) Bond strength of hard direct reline materials to heat-cured acrylic denture base after immersion in denture cleansers. Indian J Dent Res 30(6): 920-926.
- Arima T, Murata H, Hamada T (1995) Properties of highly cross-linked autopolymerizing reline acrylic resins. J Prosthet Dent 73(1): 55-59.
-
Ghazal Pazooki, Tian Fang Zhang, Sara Palladino, Diego Mantovani, Ghassan Al Dika. Bond Strength Between A Hard Chairside Reline and A Printed Denture Base Compared to A Conventional Heat Polymerized Denture Base: An In Vitro Study. On J Dent & Oral Health. 6(2): 2022. OJDOH.MS.ID.000633. DOI: 10.33552/OJDOH.2022.06.000633.
-
Denture bases, Printed dentures, CAD/CAM, Dentistry, 3D printed dentures, X-ray photoelectron spectroscopy, Mouth environment, Topography, Roughness, Thermopolymerizable polymethyl
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






