 Research Article
Research Article
Long Term Survival after TAVR in Western Denmark: A Multicentre Observational Study
Mads P Kronby1*, Lytfi Krasniqi2 and Lars PS Riber 3
1Department of Intensive Care And Aneastesiology, OUH Svendborg Hospital, Denmark
2Department of Thoracic Surgery, University Hospital Of Odense, Denmark
3Department of Thoracic Surgery, University Hospital Of Odense, Denmark
Mads P Kronby, Department of Intensive Care And Aneastesiology, Ouh Svendborg Hospital, Denmark.
Received Date:April 25, 2022; Published Date:May 09, 2022
Summary
Background: Transcatheter aortic valve replacement (TAVR) has proven a favorable treatment for patients with aortic stenosis for both lowand high-risk patients regarding complications and mortality associated with the procedure. All though clinical in-hospital outcomes seem favorable, the long lasting durability and the associated mortality is still debatable. In Denmark, we implanted the first TAVR in 2007 with all cardiac procedures registered in a large database, why we decided to look into the long-term results of TAVR in Denmark.
Method: A register based retrospective follow-up study, based on data from the Western Danish Heart Registry, which includes all TAVR-treated patients in the western part of Denmark. The primary outcome was all-cause mortality, while secondary endpoint were evaluations whether other factors as procedure-year, type of valve, and access-route had an impact on long-term outcomes.
Result: One-thousand-six-hundred-and-seventy-five patients were included. Lower age as well as transfemoral access resulted in a significantly better survival. Thirty-day survival has increased from 93.7% to 97.1% when treated between 2007-2011 and 2012-2016, respectively. Type of valve and valve size had no impact on survival or re-operation. Male gender, diabetes and smoking had an impact on risk of reoperation.
Conclusion: This study has shown that different factors have an impact on survival. Longer follow-up is warranted, to see if TAVR will give consistent good clinical data comparable, better or worse than SAVR.
Keywords:Age; Male gender; Diabetes; Smoking; Accessroute have an impact on long term survival
Introduction
Aortic stenosis (AS) is the most common valvular heart disease in the western world [1,2]. Degenerative aortic valve disease is the predominant etiology affecting 2-7% of people older than 65 years of age1,2. The risk of obtaining AS increases with increasing age, as it occurs due to mechanical wear and tear due to turbulence in the bloodstream. It is therefore expected that the population developing AS will increase in the future since the general rise in health status increases lifespan [1,2]. For decades surgical aortic valve replacement (SAVR) was the standard treatment for AS. Transcatheter aortic valve implantation (TAVR) was implemented in 2002 (2007 in Denmark) and in the beginning solely for patients as a last resort. It emerged as an alternative to optimal medical care and has shown its superiority in high surgical risk patients not suitable for SAVR [3,4]. Later studies have shown promising clinical outcomes in low to intermediate-risk patients [5-8].
Studies have found, that high-risk patients older than 70 years with severe symptomatic AS, treated with TAVR have a good overall survival rate [9-12]. One study found a relative survival for all consecutive TAVR-patients between 2007-2014 in the UK of 95.4%, 90.2% and 83.8% compared to the general population after 30 days, 1 and 3 years, respectively, in a cohort with a mean logistic Euroscore of 21.9 (1.51–93.6) [13]. Another study found that compared to an age- and sex-matched control group, TAVRpatients had a higher 90-day mortality (HR: 3.90; 95%-CI: 2.82- 5.39; P<0.01), while late mortality was in-different between the TAVR-group and the background population (HR: 1.16; 95%- CI: 0.96-1.40, P=0.13). Suggesting that TAVR reduces the risk of cardiac death, though some in the background population probably have non-treated AS. Further, patients referred to TAVR are also examined for other diseases prior to their treatment, why other comorbidities likely will be addressed as well [14].
In the beginning of the era, TAVR-procedures had different problems, like increased risk of paravalvular leakage (PVL) and need of pacemaker implantation. As valves and equipment have been developed and TAVR-implanters have become better at choosing the optimal valve and placement of this, the increased risk seems to be largely minimized over time [4]. This likewise complies to the risk of stroke and TIA [3-5,15-19]. TAVR has proven to reduce the amount of symptoms in comparison to medical treated patients [3,17]. The majority of patients are still alive and in NYHAclass I-II five to six years after the procedure, which is clearly an improvement to most patients preoperative status of NYHA class III-IV. TAVR have shown both better all-cause and cardiovascular survival compared to the optimal medical treatment [3,9,10].
Results differ which access route results in lowest mortality and least complications, although most studies seem to find most favorable outcomes with transfemoral technique [9-12,18,20,21]. The objective of this study is to evaluate all-cause mortality and describe risk factors with an impact on patient survival and the risk of re-operation. Furthermore, we aim to determine incidence of different post procedural clinical outcomes, and their impact on risk of death.
Patient and Method
This is a register-based observational study approved by the Region Southern Denmark Data Protection Agency, Odense, Denmark, and the study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. We conducted a population-based retrospective cohort study included patients undergoing TAVR-treatment in the Western Denmark from the beginning of the era in June 2007 up until 2016, Patients were eligible if they were older than the age of 60 years and had received TAVR-treatment in Western Denmark. Only the type of valves implanted in more than 50 patients were included. Some valves were only implanted in a limited number of times with no documentation for the reason for this. These valves were excluded in order not to act as confounders when evaluating data on Self- and Balloon-expandable valve outcomes.
We compared Self- and Balloon-expandable valves according to the primary outcome; survival, and secondary outcomes; postprocedural atrial fibrillation (POAF) or post-procedural events of stroke or Trans Ischemic Attack (TIA), new permanent pacemaker etc. Survival was also assessed both comparing access route for valve implantation. The secondary outcomes evaluated within 30 days after the procedure to evaluate on the surgical related events. All data was collected from the Western Danish Heart Registry (WDHR) and The National Danish Patient Registry with a followup to July 2018 for survival and clinical outcomes, respectively. The WDHR is a multicenter prospective registry, including all patients treated with TAVR in the western part of Denmark, and is the most comprehensive registry regarding TAVR in Denmark. Since this is a register-based study, we were not able to prevent reporting bias, which can have an impact on the amount of missing data in some variables, specifically in baseline data.
Statistical Analysis
Baseline characteristics were described using means and range for continuous variables, and proportions for categorical variables. Time to death was calculated in years from the date of TAVR to date of death from all-cause. Survival was performed graphically by Kaplan-Meier estimates. Log-rank test was performed to compare equality of survivor function of groups. We performed a COX regression analysis to evaluate risk factors for death and reported hazard ratios (HR) with 95% confidence intervals (CI). The age between 75-85 was set as reference for age related cox analysis. The same applies to prosthesis size 25-26 in respect to valve size related cox analysis. Multivariate COX regression was performed on age and other binary variables evaluated on known predisposing risk factor. A P-value of <0.05 was considered significant. All statistical analysis was performed with the use of Stata software Version [15].
Result
A total of 1785 patients consecutively underwent TAVR in the western part of Denmark between 2007 and 2016 both years included. Thirty-eight excluded due to missing data on date of procedure, 16 excluded due to age under 60 years at the time of the procedure, and 56 excluded due to having implanted a rarely used type of valve (3, 11) or missing (42 patients). The remaining 1675 patients were included in the study (Figure 1). The baseline characteristics of these patients can be seen in (Table 1).
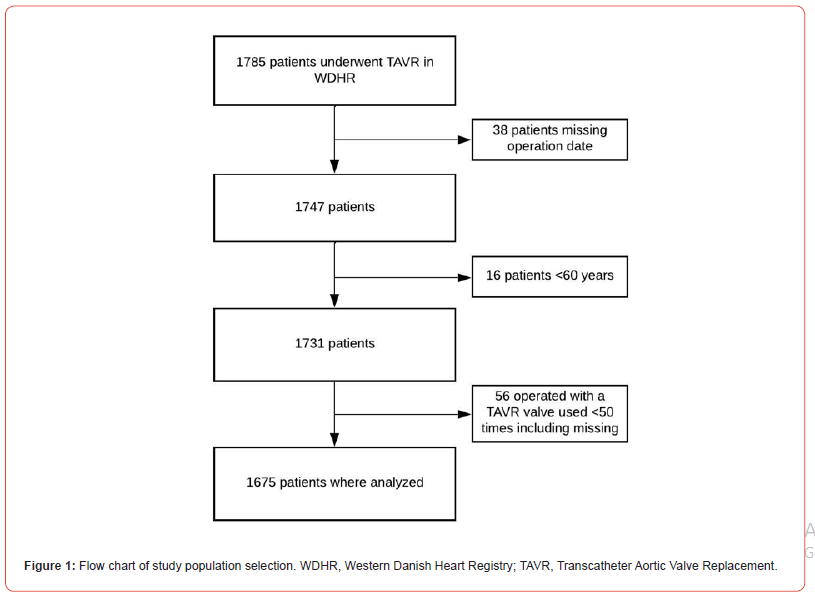
Table 1: Baseline and periprocedural characteristics of the population.
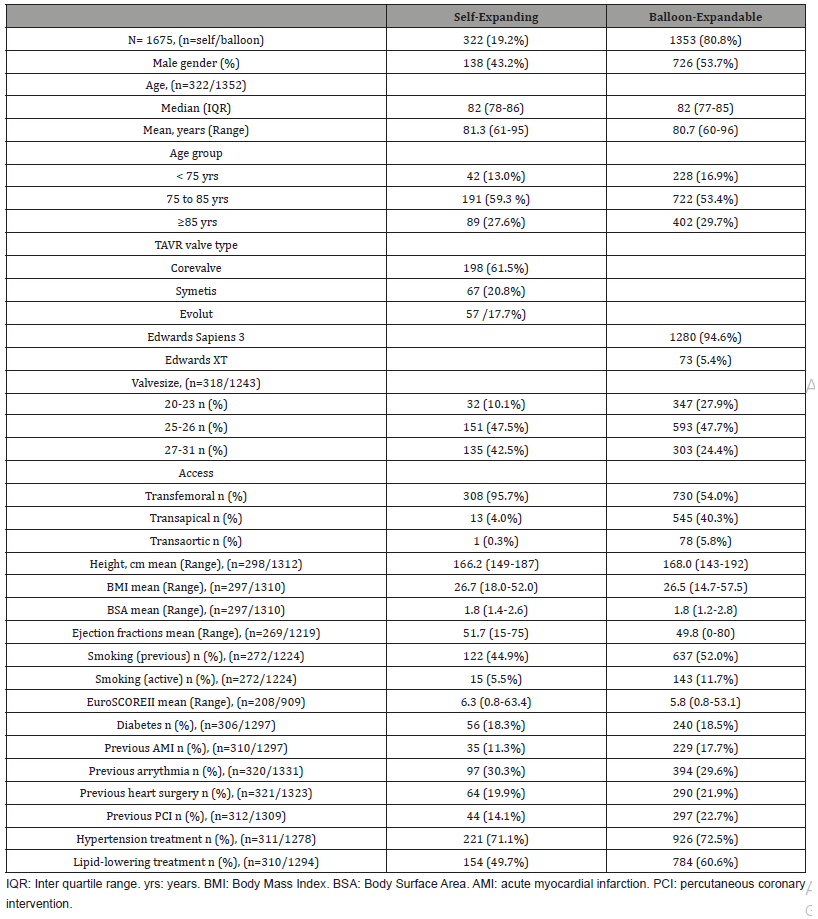
Baseline
Baseline characteristics of the patients can be seen in (Table 1). Most patients received a balloon-expandable valve (80.8%). We found a mean age of 81.3 years in the self-expanding group versus 80.7 in the balloon-expandable group, with more than 50% in each group between 75-85 years. In the self-expanding group 50.4% were either active or previous smokers versus 63.7 % in the balloon-expandable group. In the self-expandable group 34% had previous heart surgery compared to 44.6 % in the balloonexpandable group. Mean EuroSCOREII 6.3 and 5.8, respectively.
Survival
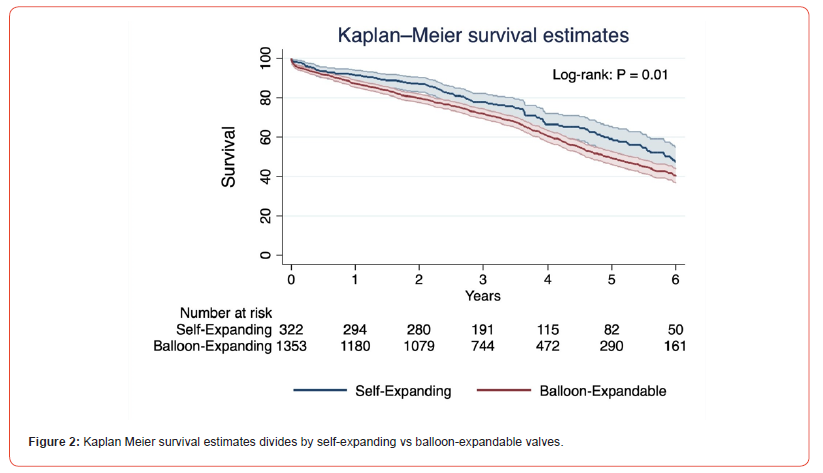
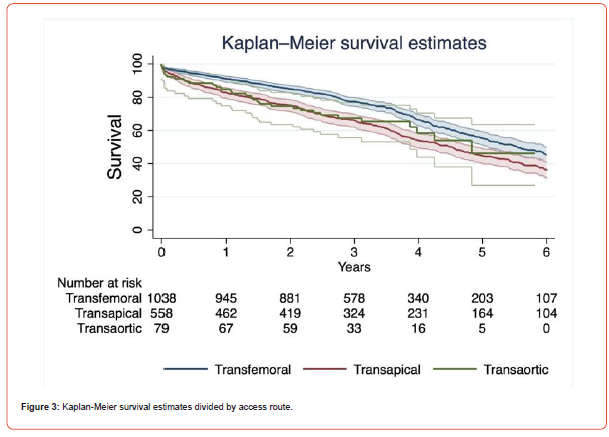
Survival by valve type shown in (Figure 2), while (Figure 3) shows survival related to access route. Patients with a selfexpanding valve had a survival of 98.2% (95%-CI: 95.9-99.2%), 91.3% (95%-CI: 87.7-93.9%), 77.9% (95%-CI: 72.7-82.1%), 59.1% (95%-CI: 52.1-65.5%) and 47.5% (95%-CI: 39.6-55.0%) after 30 days, 1, 3, 5 and 6 years respectively. In the patient with a balloonexpandable valve it was 95.9% (95%-CI: 94.7-96.8%), 87.2% (95%-CI: 85.3-88.9%), 71.9% (95%-CI: 69.4-74.3%), 49.6% (95%- CI: 46.2-52.8%) and 40.1 (95%-CI: 36.5-43.7%) after 30 days, 1, 3, 5 and 6 years. Years of survival is significantly increased in self-expandable TAVR in comparison to balloon-expandable TAVR (P=0.01). Regarding access route a 30-day survival of 97.2% (95%- CI: 96.0-98.1%), 95,2% (95%-CI: 93.0-96.7%) and 92.4 (95%- CI: 83.9-96.5%) in the transfemoral, transapical and transaortic groups was found. Further, 6-year survival was 45.3% (95%-CI: 40.6-49.9%) in transfemoral group, 35.7% (95%-CI: 31.1-40.4%) in the transapical and 46.2% (95%-CI: 26.9-63.6%) in the transaortic group. Though, these groups were not fully comparable with EuroSCORE2 showing 5.3, 7.3 and 6.6 in the tree arms respectively. The curves in (Figure 3), a significant difference in survival between transfemoral and transapical group (log-rank P <0.05). Transaortic is not significantly different in survival compared to other access routes at any time.
We also compared survival in different age groups and observed a survival of 95.6% (95%-CI: 92.3-97.5%), 72.2% (95%- CI: 66.3-77.3%) and 41.5% (95%-CI: 32.8-49.9%) after 30 days, 3 and 6 years in patients younger than 75 years of age. In patients of 75-85 years, these numbers were 96.5% (95%-CI: 95.1-97.5%), 73.9% (95%-CI:70.3-76.6%) and 44.8% (95%-CI:40.4-49.1%). In the oldest patients (older than 85 years) survival after 30 days was 96.3% (95%-CI: 94.2-97.7%), 72.3% (95%-CI: 68.8-76.1%) after 3 years and 35.6% (95%-CI: 29.6-41.7%) after 6 years. There was no significant difference in survival based on age. Overall survival was compared in all procedures of TAVR from 2007-2011 (both years included, n=383) with 2012-2016 (both years included, n=1292). Log-rank analysis was non-significant (P=0.14) even though mortality after 30 days was 6.3% and 2.9%, respectively. Mortality after 5 years was 48.3% and 50.9%, respectively. Cox-regression was also non-significant while presenting a 12% reduction in risk of death in between 2012-2016 with 2007-2011 (HR 0.88, 95%-CI: 0.75-1.04, P=0.14).
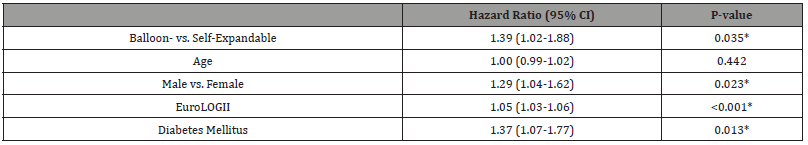
Table 2 is a univariate Cox-regression on different factors which might have an impact on survival. Male gender showed an increased risk of death with a hazard ratio (HR) of 1.59 (1.13-2.25) P: 0.009 in self-expanding and 1.2 (1.03-1.41) P: 0.019 in balloonexpandable. Increasing age was significant for increased mortality in the balloon-expandable group; HR: 1.01 (95%-CI: 1.0-1.03) P: 0.034, but not in the self-expanding group (P: 0.344). Diabetes was significant for early mortality in the balloon-expandable group, HR: 1.3 (1.07-1.58) P: 0.009. Active smoking was associated with higher risk of early mortality in both groups, while previous smoking was only significant in the self-expanding group. In (Table 3) we have a multivariate cox-regression. This shows that when age is increased with 1, the hazard risk is increasing with 2 % in the balloonexpandable group when covariates are adjusted for. Diabetes in the balloon-expandable group, and male gender and previous AMI in both groups were also significant for early mortality (Table 4).
Table 2: Univariate COX-regression.
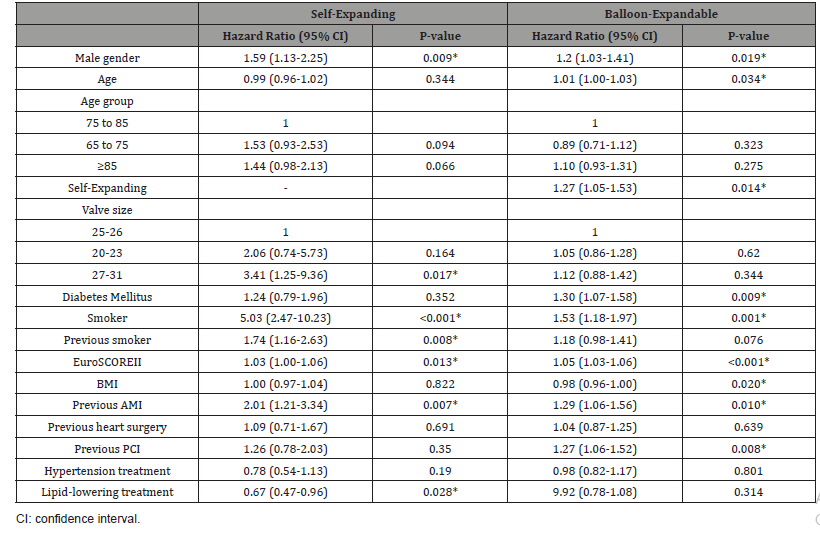
Table 3: Multivariate COX-regression.
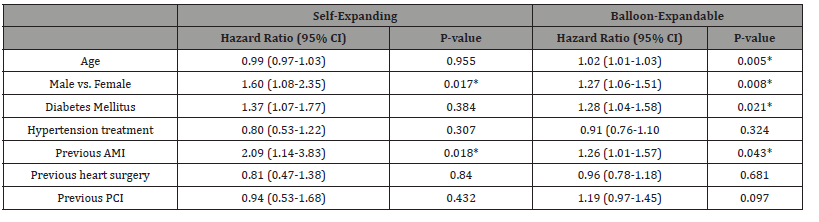
Table 4: Univariate COX-regression on entire TAVR cohort.
Clinical outcomes
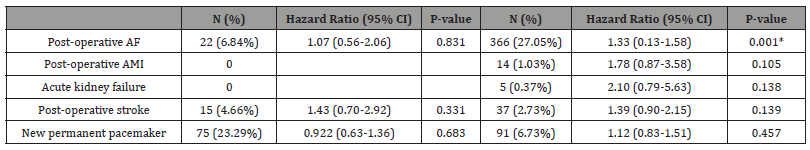
We evaluated patients on different clinical outcomes within the first 30-days post procedure. These data are shown in (Table 5). Postoperative atrial fibrillation (POAF) was registered in only 6.9% of patients with a self-expanding valve, compared to 27.1% in patients with a balloon-expandable valve. In both groups POAF had no significant impact on risk of mortality. A new permanent pacemaker was implanted in 23.3% of patients with a selfexpanding valve, while this was only performed in 6.7% of patients with a balloon-expandable valve. None of these had a significant impact on the risk of mortality. No other differences found between the two groups in any of the other clinical outcomes.
Table 5: Univariate COX-regression on clinical outcomes.
Discussion
This comprehensive study regarding 14 years of TAVRimplementation in Denmark gives an excellent opportunity to investigate the long-term survival and morbidity. It is crucial to investigate the long-term data to make the right decision for the next patient in line with severe aortic stenosis. This study included patients from the beginning of the TAVR-era in Denmark up until the end of 2016 to secure long-term follow-up data. In this timespan, the approach to TAVR-treatment and the patient criteria has changed from only including inoperable patients, moving towards including lower risk patients as well16. This is expected to have an impact on long term survival, why it would have been optimal to have equal follow-up in all patients. Another confounder, as mentioned earlier, that in the beginning of the era, only high-risk patients received TAVR treatment. This complies well with our finding that the EuroSCOREII has been decreasing over time from 19 in patients who received their treatment in 2008, the year after introducing in Denmark, to 15.6 in 2016. This in consistent with another study investigating changes in baseline characteristics in TAVR patients over time found the same [22]. However, the difference in survival between the first 5 years and the last 5 years was non-significant. Therefore, a randomized or a prospective observational study of patients included today and an onwards, probably will be more representative, though the result of this trial probably already would be non-representative when the data is obtained due to new valves and changed patient category.
Another work focused on low-intermediate patients found an increased early mortality compared to an age and gender matched background population, but after 90 days there was no significant difference in mortality, which suggest that these patient has higher early mortality due to procedure complications, while the treatment resolves them for an increased risk of early heartdeath [14]. Studies comparing SAVR to TAVR are not conclusive whether one treatment is better than the other when it comes to low-risk after 1 year [5], like long-term studies implies that SAVR is significantly better than TAVR after 5 years [23].
In this retrospective study, we found that different factors had an impact on long-term survival. Firstly, our data showed that age had a significant impact on survival when adjusted for covariates in balloon-expandable valves, this is seen both in uni- and multivariate Cox regressions analysis. The lack of significance in the other group might just be a type 2 error due to small sample size. Regarding access routes, transfemoral (TF) had the best outcome regarding survival. However, one should notice that TF was the primarily chosen access route, and other routes were only used, when TF was not an option due to excessive arteriosclerosis, which made the risk of TF too high. Therefore, patients treated through transapical or transaortic is expected to have a higher procedure related risk and with this an increased mortality, as shown in (Table 2).
Short-term clinical outcomes and their impact on survival are important too. We found that only patients with POAF had a significantly increased HR, and only in the balloon-expandable valves. Post-operative AMI, Acute kidney failure and stroke, and implantation of new permanent pacemaker had no significant impact on risk of death. Apart from POAF none of the shortterm clinical outcomes had a negative impact on survival, which could be due to sample-size and therefore likewise type 2 error. Receiving a pacemaker within 30 days after TAVR, did not result in a significantly higher risk of mortality. Patients receiving a pacemaker are no longer in risk of dying due to heart rhythm failure, and so this was an expected result that correlates well with findings in another study, where they also didn’t find any correlation (6).
These outcomes are evaluated overall. We expected that the results might not be directly representative, because of the evolvement of both surgeons and equipment over the years. One study found a significantly decrease in procedural time, length of hospitalization and 30-day all-cause mortality with increasing experience of the surgeon and development of the equipment [22]. However, this cohort presented that survival in the last five years (2012-2016) was not significantly higher than the first 5 years (2007-2011). A sample size of 383 versus 1292 patients was not enough to find a significant difference, even though the procedure has become standard practice in a population with a decreasing risk compared to the beginning of the era. This study has evaluated survival and different clinical outcomes after TAVR-treatment. Further research is needed to evaluate these more in depth.
Conclusion
We found long term survival with an overall survival after 6 years of 47,5% in the self-expanding group and 40,1% in the balloon-expandable group. Clinical outcomes within 30 days had a low incidence which is promising. Further work is needed to directly compare these results to SAVR-patients.
Limitations
1. Unfortunately, we do not have the same length of followup for all patients in the population, why some patients have only been followed for 2 years.
2. Another limitation is the difference in sample size when patients are compared on valve type, access route and subgroups with a type 2 error. As described earlier we selected valves with a minimum of 50 patients to minimize sampling bias. Furthermore, by the register-based study design, and the data collection was not made specifically for this study.
3. The TAVR population is a very selected population because they are not suitable for surgery or have reduced life expectancy, why we included every patient to try to minimize selection bias within the TAVR group. Furthermore, the indication for TAVR has evolved greatly compared to the early stages of the era moving from only high-risk patients to also include low-risk patients.
4. Finally, this study focused solely on TAVR treatment and makes no comparison to SAVR. The big question, whether TAVR is inferior, superior, or equal to SAVR when it comes to longterm outcomes in low-risk patients still remains.
Perspective Statement
Transcatheter aortic valve replacement is increasingly used treatment for aortic stenosis. This study evaluates mortality and different clinical outcomes after the procedure in a Danish population. Different factors that has an impact on outcomes is also evaluated.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Bärwolf C, et al. (2003) A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 24(13): 1231-1243.
- Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, et al. (2006) Burden of valvular heart diseases: a population-based study. Lancet 368(9540): 1005-1011.
- Kapadia SR, Leon MB, Makkar RR, Tuzcu EM, Svensson LG, et al. (2015) 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385(9986): 2485-2491.
- Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, (2015) 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385(9986): 2477-2484.
- Thyregod HGH, Steinbrüchel DA, Ihlemann N, Nissen H, Kjeldsen BJ, (2015) Transcatheter Versus Surgical Aortic Valve Replacement in Patients with Severe Aortic Valve Stenosis: 1-Year Results From the All-Comers NOTION Randomized Clinical Trial. J Am Coll Cardiol 65(20): 2184-2194.
- Søndergaard L, Steinbrüchel DA, Ihlemann N, Nissen H, Kjeldsen BJ, et al. (2016) Two-Year Outcomes in Patients with Severe Aortic Valve Stenosis Randomized to Transcatheter Versus Surgical Aortic Valve Replacement: The All-Comers Nordic Aortic Valve Intervention Randomized Clinical Trial. Circ Cardiovasc Interv 9(6): e003665.
- Wenaweser P, Stortecky S, Schwander S, Heg D, Huber C, et al. (2013) Clinical outcomes of patients with estimated low or intermediate surgical risk undergoing transcatheter aortic valve implantation. Eur Heart J 34(25): 1894-1905.
- Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, et al. (2016) Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 374(17): 1609-1620.
- Bouleti C, Himbert D, Iung B, Alos B, Kerneis C, et al. (2015) Long-term outcome after transcatheter aortic valve implantation. Heart 101(12): 936-942.
- Codner P, Orvin K, Assali A, Sharony R, Vaknin-Assa H, et al. (2015) Long-Term Outcomes for Patients with Severe Symptomatic Aortic Stenosis Treated With Transcatheter Aortic Valve Implantation. Am J Cardiol 116(9): 1391-1398.
- D’Onofrio A, Facchin M, Besola L, Manzan E, Tessari C, et al. (2016) Intermediate Clinical and Hemodynamic Outcomes After Transcatheter Aortic Valve Implantation. Ann Thorac Surg 101(3): 881-888.
- Zahn R, Werner N, Gerckens U, Linke A, Sievert H, et al. (2017) Five-year follow-up after transcatheter aortic valve implantation for symptomatic aortic stenosis. Heart 103(24): 1970-1976.
- Martin GP, Sperrin M, Hulme W, Ludman PF, de Belder MA, et al. (2017) Relative Survival After Transcatheter Aortic Valve Implantation: How Do Patients Undergoing Transcatheter Aortic Valve Implantation Fare Relative to the General Population. J Am Heart Assoc 6(10): e007229.
- Theut M, Thygesen JB, De Backer O, Søndergaard L (2017) Survival and cause of death after transcatheter aortic valve replacement as compared to an age- and sex-matched background population. EuroIntervention 13(9): e1058-e1066.
- Kodali SK, Williams MR, Smith CR, Svensson LG, Webb JG, et al. (2012) Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 366(18): 1686-1695.
- Tam DY, Vo TX, Wijeysundera HC, Ko DT, Rocha RV, et al. (2017) Transcatheter vs Surgical Aortic Valve Replacement for Aortic Stenosis in Low-Intermediate Risk Patients: A Meta-analysis. Can J Cardiol 33(9): 1171-1179.
- Leon MB, Smith CR, Mack M, Miller DC, Moses JW, et al. (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363(17): 1597-1607.
- Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, et al. (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364(23): 2187-2198.
- Makkar RR, Fontana GP, Jilaihawi H, Kapadia S, Pichard AD, et al. (2012) Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med 366(18): 1696-1704.
- Gargiulo G, Sannino A, Capodanno D, Barbanti M, Buccheri S, et al. (2016) Transcatheter Aortic Valve Implantation Versus Surgical Aortic Valve Replacement: A Systematic Review and Meta-analysis. Ann Intern Med 165(5): 334-444.
- Sawa Y, Takayama M, Goto T, Takanashi S, Komiya T, et al. (2017) Five-Year Outcomes of the First Pivotal Clinical Trial of Balloon-Expandable Transcatheter Aortic Valve Replacement in Japan (PREVAIL JAPAN). Circ J 81(8): 1102-1107.
- Lareyre F, Raffort J, Dommerc C, Habib Y, Bourlon F, et al. (2018) A 7-Year Single-Center Experience of Transfemoral TAVI: Evolution of Surgical Activity and Impact on Vascular Outcome. Angiology 69(6): 532-539.
- Zhang XL, Zhang XW, Xu W, Xu B (2021) Response to the Comment on “Long-term and Temporal Outcomes of Transcatheter Versus Surgical Aortic-valve Replacement in Severe Aortic Stenosis: A Meta-analysis”. Ann Surg 274(6): e837-e838.
-
Mads P Kronby*, Lytfi Krasniqi and Lars PS Riber. Long Term Survival after TAVR in Western Denmark: A Multicentre Observational Study. On J Cardio Res & Rep. 6(4): 2022. OJCRR.MS.ID.000644.
-
Age, Male gender, Diabetes, Smoking, Heart disease, Cardiac death, Heart registry, Heart surgery, Heart rhythm failure, Bloodstream, Stroke, Epidemiology
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






