 Research Article
Research Article
Gender Based Disparities Among Wide Range of Cardiac Failure Patients Reporting at Benazir Bhutto Hospital Rawalpindi During 2019-2020
Imran Saeed Ali1, Rizwana Shahid2* and Tahira Sadiq3
1Professor of Cardiology, PAF Hospital, Pakistan
2Assistant Professor Community Medicine, Rawalpindi Medical University, Pakistan
3Assistant Professor of cardiology, PAF hospital Islamabad, Pakistan
Rizwana Shahid, Assistant Professor Community Medicine, Rawalpindi Medical University, Rawalpindi, Pakistan.
Received Date: March 07, 2023; Published Date: March 23, 2023
Objectives: To determine gender-based variations among cardiac failure patients visiting a tertiary care hospital of Rawalpindi during 2019- 2020.
Subjects & Methods: A cross-sectional descriptive study was done by enrolling 490 cardiac failure patients through consecutive non-probability sampling. Data was gathered from the patients and their attendants about demographics, clinical manifestations, comorbidities, test reports and healthcare outcomes. Patients were also categorized in accordance with New York Heart Association (NYHA) classification. Data analysis was done by SPSS version 25.0 and Microsoft Excel 16.0. Gender-wise differences in mean age of the patients was confirmed by independent sample t-test while the disparities in comorbidities, risk factors, lab tests, cardiac associated biochemical parameters and healthcare outcome were statistically proved by chi-square test. P ≤ 0.05 was considered as significant.
Results: Of the total 490 heart failure patients, 292 and 198 were males and females respectively. Mean age of the patients was 53.2 ± 15.04 years; however, gender-wise difference in mean age was statistically insignificant (P>0.89). More males complained of chest pain (P<0.001). Around 41% of the patients were in class-I of NYHA heart failure classification. Gender-based difference in proximity to predisposing factors like diabetes, hypertension and smoking was statistically significant with P<0.05, P<0.001 and P<0.000 respectively. Relatively more females had pallor (P<0.005). despite the derangement of CK-MB and chest X-ray among 75% of the cases, gender-wised disparity was statistically insignificant (P>0.20). about 77% and 88.3% of the male and female patients subjected to cardiac Troponin-I testing had negative test report. Total 8 patients were succumbed to heart failure.
Conclusion: overall gender-related variations in heart failure cases was statistically insignificant.
Keywords:Cardiac failure; New York Heart Association; Biochemical parameters; CK-MB; Healthcare outcome
Introduction
Cardiac failure is associated with certain anatomical and physiological diversities in myocardium that leads to diminished ventricular filling and henceforth minimal ejection fraction [1]. Patients with this disease are likely to have diverse healthcare outcomes that may vary from hospitalization for treatment to sudden death [2]. Being a silent epidemic, cardiovascular disorders have gained significant attention of healthcare professionals because this ailment in addition to other non-communicable diseases constitutes about 79% of the subsequent global burden of disease [3].
Ischemic heart disease was identified as the second commonest cause of death during 2009 and even after 10 years this disease persisted globally as the 2nd leading cause of mortality [4]. In addition to death, Disability Adjusted Life Years (DALY) has significantly been attributed to the cardiovascular disorders [5]. Demographic survey of Pakistan 2020 revealed that maximum propensity of our population is succumbing to cardiovascular disorders [6]. On reviewing the gender-based discrepancies in outcome of heart failure, women are known to have comparatively better prognosis. Even sudden cardiac death has been reported relatively more among male cardiac failure patients [7]. A study carried out by Ho JE, et al. on massive population to predict the risk of heart failure presented hazard ratio of 2.0 with respect to Heart failure reduced Ejection Fraction (HFrEF) [8].
Although gender-wise variations in epidemiology of cardiac failure have been elucidated in Framingham [9] and Rotterdam [10] heart studies carried out among 40 years and 55 years old people respectively about 19-20 years back; yet that data among Asians is scarce. The present study is hence proposed to study sex-based differences in risk factors, clinical presentations, investigations, and eventual healthcare outcomes among cardiac failure cases reporting to a public sector tertiary care hospital of Rawalpindi. This study by pinpointing the gender-wise diversities would enable our cardiologists and relevant staff to manage the cases aptly for their better prognosis.
Subjects & Methods
A cross research descriptive study was done among 490 heart failure patients who visited and managed at Cardiology department of Benazir Bhutto Hospital, Rawalpindi during 2019- 2020. This study was done conforming to STROBE checklist [11]. Patients getting consultation with cardiologist either in Outpatient or Emergency department were included in the study through consecutive non- probability sampling. The data was collected from these patients regarding their demographics, comorbidities, clinical manifestations, laboratory investigations and health outcomes. Heart failure of the patients was also graded as per NYHA functional classification that is meant to categorize heart failure of the patients in configuration with severity of symptoms [12]. A structured questionnaire was designed to gather all relevant data by interviewing the patients. Informed consent was taken from the patients or their attendants before interviewing in order to avoid procedural bias. The data was analyzed by means of SPSS version 25.0 and Microsoft Excel 16.0. Gender-wise diversities in mean age of the patients was determined by independent sample t-test while the variations in comorbidities, risk factors, test results, cardiac-linked biochemical indicators, and healthcare outcome were statistically verified by application of chi-square test. P ≤ 0.05 was considered as significant.
Results
Of the total 490 cardiac failure patients visiting Benazir Bhutto Hospital Rawalpindi during 2019-2020, males constituted the majority 292 (59.6%). Mean age of our patients was 53.2 ± 15.04 years. However, gender-wise difference in mean age of our cardiac failure patients was statistically insignificant as depicted below in Table 1.
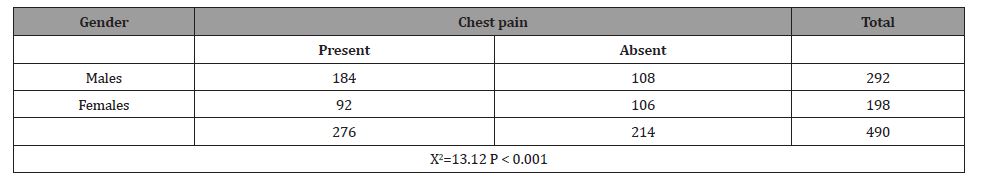
Chest pain was determined to be the most frequent among our male cardiac failure patients (P < 0.001) as illustrated below in Table 2.
Table 1:Gender-based variation in mean age of cases.
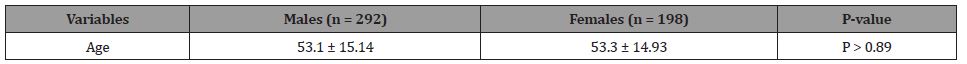
Table 2:Gender-wise variation in the frequency of chest pain among heart failure patients.
Most of the patients with chest pain were in Class-I of NYHA (New York Heart Association) as illustrated below in Figure 1.
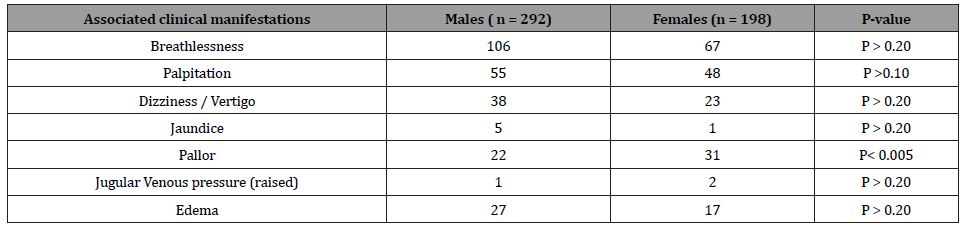
Of the varied clinical manifestations, pallor has momentously been detected among females (P <0.005) as reflected below in Table 4.
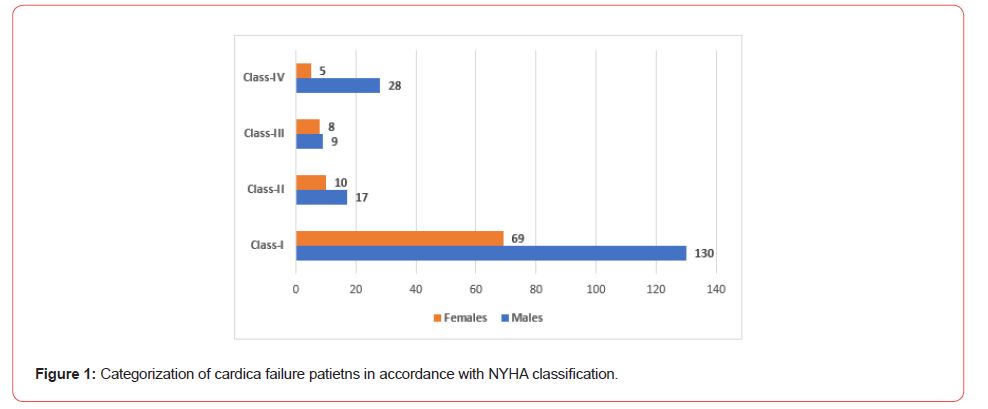
Table 3:Occurrence of predisposing factors in heart failure patients.
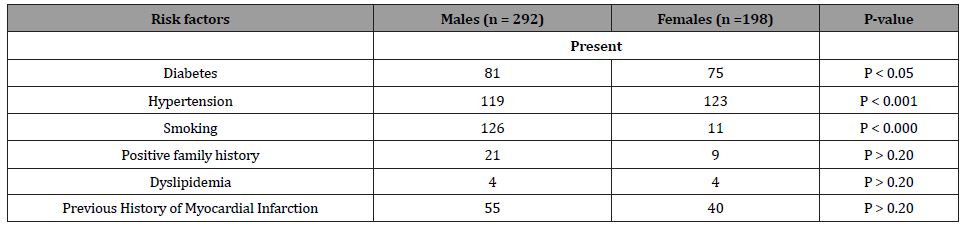
Table 4:Gender based disparities in clinical manifestations associated with cardiac failure patients.
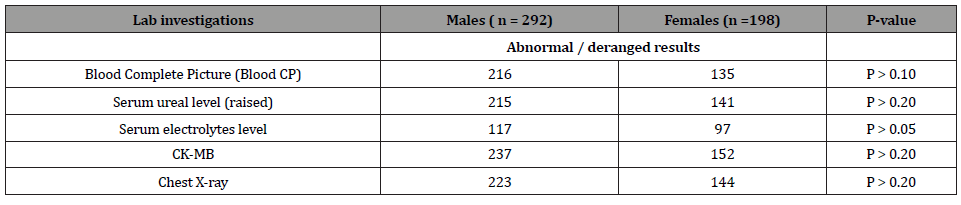
About 32 male and 16 female patients in current study received streptokinase injection. Out of 198 female patients, 3 had congenital anomalies which were Atrial Septal Defect (ASD), Patent Ductus Arteriosus (PDA) and ebstein anomaly. On the other hand, male patients did not have congenital anomaly. One male and two female patients had past history of rheumatic heart disease. Results of CK-MB and chest X-ray were comparatively more abnormal among male patients as shown below in Table 5.
Table 5:Gender-wise differences in Lab investigations and other tests.
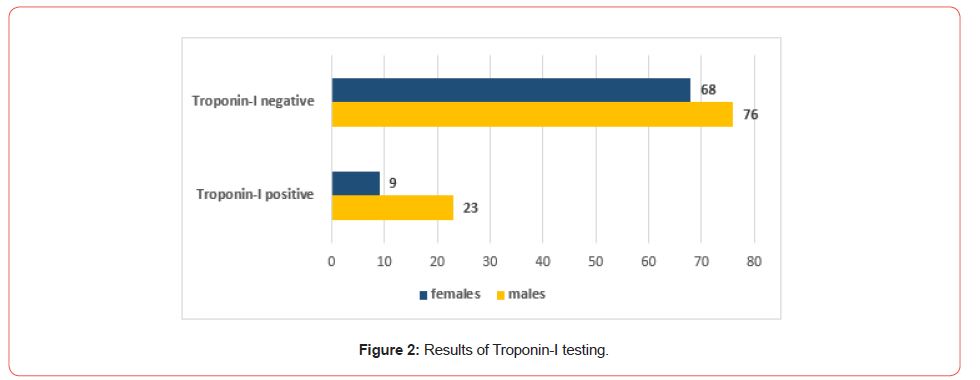
Only 99 males and 77 females were subjected to Troponin-I testing and about 77 % males and 88.3% females had negative test report as depicted below in Figure 2.
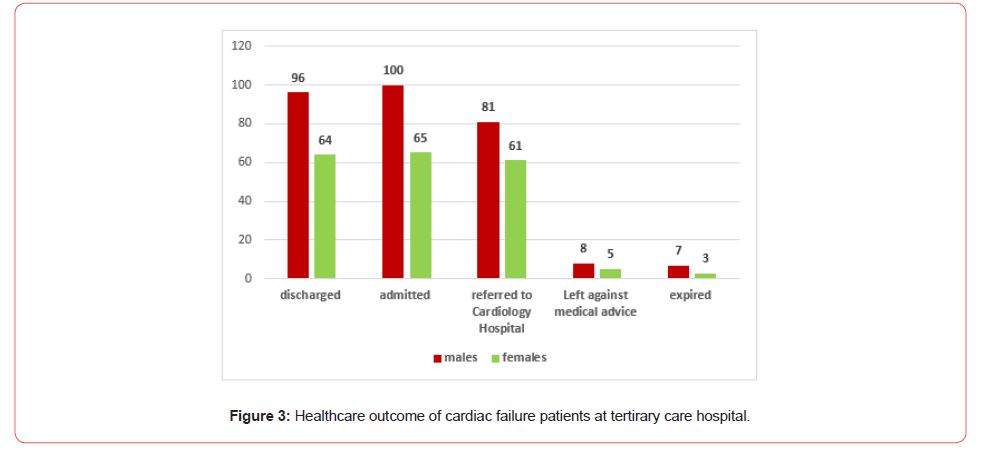
Fate of the cardiac patients in our study with males compartively more succumbig to cardiac failure is portrayed below in Figure 3.
Discussion
Cardiac failure being a silent epidemic has been predicted as a havoc that is not only drastically influencing the patients and their attendants but is also likely to result in tremendous rise in healthcare costs13. Succumbing to cardiac failure, increased hospitalizations and poor healthcare consequences are the attributes that emphasize the sensible management of cases with desirable outcome [14]. In current study, about 184 and 92 male and female patients respectively complained of chest pain while 106 males and 67 females had concomitant breathlessness. Chest pain was significantly been reported among males (P < 0.001). A prospective cohort study done by Barnett LA et al among cardiovascular cases of United Kingdom concluded that breathlessness was relatively more frequent among females. Contrary to our results, even breathlessness was determined to be in higher propensity than that of chest pain among cardiac failure patients [15]. Cardiovascular patients can experience the symptoms of chest pain and breathlessness either simultaneously or separately [16]. However, this difference in occurrence of both symptoms among UK and Pakistani population might be interlinked with multiple associated risk factors in addition to geographical diversity that should thoroughly be sought for clarification.
Of the varied comorbidities, male patients in our study were more diabetic (P<0.05) while females were comparatively more hypertensive (P<0.001). Maximum propensity of cardiac failure patients worldwide has been recognized with both cardiac as well as non-cardiac morbidities like diabetes, hypertension, obesity and chronic renal disorders [17]. Heart failure among our male cases has significantly been attributed to smoking (P <0.000). Gender based diversities in risk factors associated with heart failure have also been acknowledged in a cross-sectional study carried out among 65-84 years old patients who were randomly sampled in accordance with 2005 European Society of Cardiology (ESC) criteria [18]. Positive family history and dyslipidemia among our studied cases were not only meager but also revealed insignificant sexlinked association (P>0.20). A systematic review done to quantify the comorbidities among patients during heart failure clinical trials also illustrated upsurge of hypertension, chronic renal disease and atrial fibrillation but substantially reduced trend of smoking [19]. A study by Screever EM et al analyzing 15 years scenario delineated obesity as the most predominant comorbid state that drastically influenced the healthcare outcome of the heart failure patients [20]. One of the reasons for not displaying BMI in our study might be the collection of data from the general public who can afford visit and consultation in public sector hospitals. Correlation of BMI with heart failure can best be determined by executing a multicenter study.
Of the total 490 heart failure cases enrolled in present study, majority (59.6%) were males. However, gender-based difference in deaths was determined to be statistically insignificant (P > 0.20). A similar study by Larsen HE et al among Greenland people explicated comparable facts and figures [21]. Another study carried out among population of United Kingdom from 2000-2017 explicated less survival gains among cardiac failure females over the last two decades [22]. On comparing Tropinin-I level among our study subjects, females had comparatively more (88.3%) negative troponin-I test report (Figure 2). Likewise, a study by Cediel G exhibited lower cardiac troponin levels among women that is a diagnostic biomarker in heart failure [23]. Raised cardiac troponin-I levels have been detected among both acute and chronic heart failure cases that has been attributed to numerous pathophysiological changes [24]. This biomarker is of chiefly significant in measuring the prognosis and disease severity [25]. Patients with elevated troponin-I level have higher risk of mortality than those with diminishing levels [26]. A study by Gherasim L, et al. has emphasized the screening of general population for cardiac troponin-I levels in order to perceive their risk of developing heart failure [27]. However, apart from such biochemical indicators, clinical manifestations among the patients need due consideration for prompt management and care provision in order to get rid of grave consequences. Gender-wise similarities and discrepancies in risk to heart failure should be deliberated to dig out the complexities of heart failure.
Conclusion & Recommendations
Although heart failure is a complex disease with gender-based adherence to some of the modifiable risk factors; however sexlinked diversities among heart failure cases were insignificant. Prospective studies with extensive data can provide the stakeholders with certain facts that can substantially aid in suppressing the magnitude of this non-communicable disease.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Dassanayaka S, Jones SP (2015) Recent Developments in Heart Failure. Circ Res 117: e58-e63.
- Skrzynia C, Berg JS, Willis MS, Jensen BC (2015) Genetics and heart failure: a concise guide for the clinician. Curr Cardiol Rev 11(1): 10-17.
- Kazmi T, Nagi MLF, Razzaq S, Hussnain S, Shahid N, et al. (2022) Burden of noncommunicable diseases in Pakistan. East Mediterr Health J 28(11): 798-804.
- IHME Pakistan. What causes the most deaths?
- Global 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396: 1204-1222.
- Government of Pakistan. Pakistan Demographic Survey 2020. April 2022.
- Regitz-Zagrosek V (2020) Sex and Gender Differences in Heart Failure. Int J Heart Fail. Apr 13 2(3): 157-181.
- Ho JE, Enserro D, Brouwers FP, Kizer JR, Shah SJ, et al. (2016) Predicting Heart Failure with Preserved and Reduced Ejection Fraction: The International Collaboration on Heart Failure Subtypes. Circ Heart Fail. Jun 9(6): 10.
- Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D'Agostino RB, et al. (2002) Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. Dec 10 106(24): 3068-3072.
- Bleumink GS, Knetsch AM, Sturkenboom MC, Straus SM, Hofman A, et al. (2004) Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur Heart J Sep 25(18): 1614-1619.
- STROBE Checklist.
- American Heart Association. Classes of heart failure.
- Desai AS, Stevenson LW (2012) Rehospitalization for heart failure: predict or prevent? Circulation 126(4): 501-506.
- Dunlay SM, Redfield MM, Weston SA, Therneau TM, Hall Long K, et al. (2009) Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol 54(18): 1695-1702.
- Barnett LA, Prior JA, Kadam UT, Jordan KP (2017) Chest pain and shortness of breath in cardiovascular disease: a prospective cohort study in UK primary care. BMJ Open 7(5): e015857.
- Clark N, Fan VS, Slatore CG, Locke E, Whitson HE, et al. (2014) Dyspnea and Pain Frequently Co-occur among Medicare Managed Care Recipients. Ann Am Thorac Soc 11(6): 890-897.
- Iyngkaran P, Majoni W, Cass A, Sanders P, Ronco C, et al. (2015) Northern territory perspectives on heart failure with comorbidities-understanding trial validity and exploring collaborative opportunities to broaden the evidence base. Heart Lung Circ 24(6): 536-543.
- Cesaroni G, Mureddu GF, Agabiti N, Mayer F, Stafoggia M, et al. (2021) Sex differences in factors associated with heart failure and diastolic left ventricular dysfunction: a cross-sectional population-based study. BMC Public Health 21(1): 415.
- Khan MS, Tahhan AS, Vaduganathan M, Greene SJ, Alrohaibani A, et al. (2020) Trends in prevalence of comorbidities in heart failure clinical trials. European J Heart Failure 22(6): 1032-1042.
- Screever EM, van der Wal MHL, van Veldhuisen DJ, Jaarsma T, Koops A, van Dijk KS, et al. (2023) Comorbidities complicating heart failure: changes over the last 15 years. Clin Res Cardiol 112(1): 123-133.
- Larsen HE, Geisler UW, Gustafsson F, Jorgensen ME, Pedersen ML (2023) Prevalence and clinical features of heart failure in Greenland. Int J Circumpolar Health 82(1): 2178068.
- Taylor CJ, Ordonez-Mena JM, Jones NR, Roalfe AK, Lay-Flurrie S, et al. (2021) National trends in heart failure mortality in men and women, United Kingdom, 2000-2017. Eur J Heart Fail 23(1): 3-12.
- Cediel G, Codina P, Spitaleri G, Domingo M, Santiago-Vacas E, et al. (2021) Gender-related differences in heart failure biomarkers. Front Cardiovasc Med 7: 617705.
- Wettersten N, Maisel A (2015) Role of Cardiac Troponin Levels in Acute Heart Failure. Card Fail Rev Oct 1(2): 102-106.
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, et al. (2013) ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16): e147-239.
- Felker GM, Hasselblad V, Tang WH, Hernandez AF, Armstrong PW, et al. (2012) Troponin I in acute decompensated heart failure: insights from the ASCEND-HF study. Eur J Heart Fail 14(1): 1257-1264.
- Gherasim L (2019) Troponins in Heart Failure - a Perpetual Challenge. Maedica (Bucur). Dec 14(4): 371-377.
-
Imran Saeed Ali, Rizwana Shahid* and Tahira Sadiq. Gender Based Disparities Among Wide Range of Cardiac Failure Patients Reporting at Benazir Bhutto Hospital Rawalpindi During 2019-2020. On J Cardio Res & Rep. 7(2): 2023. OJCRR.MS.ID.000658.
-
Cardiac failure, Biochemical parameters, CK-MB, Healthcare outcome, Cardiovascular disorders, Myocardium, Heart disease, Heart failure, Cardiology, Chest pain, Breathlessness, Hypertension
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






