 Research Article
Research Article
Explaining Acupuncture: Testing Traditional Chinese Medicine versus Western Biomedicine Explications
Bryan B Whaley1* and Michael J Ng2
1Professor, University of San Francisco, United States
2Optim Health and Acupuncture, Inc, United States
Bryan B Whaley, University of San Francisco, United States.
Received Date:March 02, 2023; Published Date:March 27, 2023
Abstract
Acupuncture is an increasing health-service option for those living America. With this influx of acupuncture practice is the need to understand the communicative issues involved, specifically the actual explanation of acupuncture to patients by nursing and other health practitioners. Currently, there are two explications -- Traditional Chinese Medicine and the one touted by Western Medicine. Through two separate studies, this investigation found that participants overwhelming preferred the Western Medicine explication in ratings of dependent measures and rankings of explanations, regardless of the ethnicity (i.e., Asian- or Euro-descent) of the doctor attributed to the explanation.
Keywords:Explaining illness; Acupuncture; TCM; Western Medicine
Introduction
Acupuncture has been used for centuries to treat a plethora of health conditions. In America, its use has steadily increased in the last decade [1-3], and attitude toward its use improved [4]. For instance, some estimates suggest the number of acupuncture visits increased 32% between the years of 2002 and 2007 [2]. The American Heart Association estimates a quadrupling of the number of practicing acupuncturists by 2015. And, an increasing number of insurance companies are covering the expense of acupuncture [5].
Communicative challenges for nurses and other health practitioners that accompany this increase in acupuncture prescription and treatment concern language use, explaining the nature of the process, effects of acupuncture, and any interaction between complementary and alternative medicine personnel with those practicing allopathic medicine [6-9]. For instance, Karanikas [10] details the nature of this communication issue -- explaining acupuncture -- and urges further research concerning the forces and mechanisms at work when explicating both views of acupuncture, Traditional Chinese Medicine (TCM) and Western biomedical.
Anand [11] provides a variety of strategies, sometimes drawing from both the Chinese and Western perspectives in one explanation, to explicate acupuncture to patients, with explaining (via persons’ Chinese medicine diagnosis) being among them. Evans et al. [12] found seven different types of talk that occur between acupuncture practitioners and their patients. In addition, Suarez-Almazor et al. [13] determined that the communication style (i.e., talk of expectations -- high or neutral -- of treatment effects) of the acupuncturist may be a contributing factor to successful acupuncture treatment [14], with Sherman et al. [15] finding that persons with high pretreatment expectations of acupuncture failed to be a predictor of improved back-related symptoms or functions. Finally, acupuncturists are chosen and evaluated on communication and explanation skills [16,17].
Acupuncturists communicative task of explaining the nature of acupuncture increases in complexity given that there are two explanations for the nature of acupuncture and its effects. A foundational step in addressing these communication concerns is determining if there is a rating difference between the two explanatory options -- Traditional Chinese Medicine or Western Medicine. As such the following research question is warranted:
RQ1: Will there be a rating difference between the explanations?
Acupuncture is of Chinese origin, and traditionally acupuncturists have been of Chinese descent. Increasingly, however, persons of European heritage are studying acupuncture as well as becoming certified acupuncturists. Moreover, physicians of Euro decent are recommending acupuncture as a treatment option. And, given that there are two explanations of acupuncture (Chinese-based and Western-based), the ethnicity of the physician offering the explanation could affect patients’ perceptions of the acupuncture explanation. As such:
RQ2: Will there be a preference for an explanation based on perceived ethnicity of the doctor explaining acupuncture?
The aforementioned research questions will be answered by way of two investigations.
Study 1
Participants
Respondents were two-hundred six (n=206, females=132, males=64, non-report=10) undergraduate students at a private California coastal university. The ethnicity composition of this sample, as provided by participants, was: Euro-decent=104, Asian-decent= 57, Hispanic=20, Afro-decent=3, Middle Eastern=5, Multi- Mixed-decent=11, Undisclosed=6. Participation in the research was voluntary and all responses were anonymous1.
Materials and Procedures
Participants took part in a 2 (explanation type – TCM, Western) x 2 (doctor ethnicity – “Dr. Woo”, “Dr. Wood”) factorial design. Authors researched and reviewed the myriad of sources printed and on-line concerning the nature and differences between CTM and Western explanations of acupuncture and created two explanations of equal length. Respondents read one of the four message conditions and completed measures of dependent variables.
Dependent Measures
Participants were asked to respond to the doctor’s explanation on the following 9-point scales: clear/unclear, interesting/boring, factual/nonfactual, believable/unbelievable, informative/uninformative. Then, they were asked their attitude toward acupuncture, via semantic differential: good/bad, beneficial/harmful, favorable/ unfavorable, pleasant/unpleasant, wise/foolish.
Results
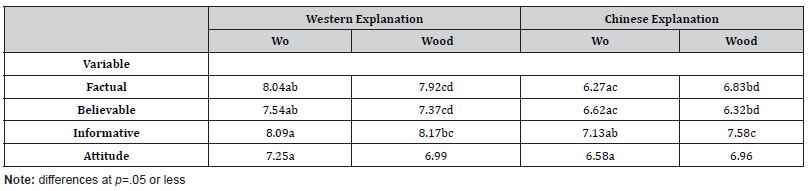
Analysis of variance procedures indicated several significant differences for dependent measures: factual (F[3,200]=13.94, p=.001), believable (F[3,202]=5.42, p=.001), informative (F[3,202]=5.45, p=.001, and attitude (F=3,202]=2.68, p=.048; RQ1). Subsequent t-test analyses noted specific differences between groups such that the Western explanation, regardless of doctor ethnicity (RQ2), was rated higher on the aforementioned variables (Table 1). There were no differences between Asian- and Euro-descent participants’ ratings on any of the dependent variables concerning the explanations. Interestingly, though there were no differences in attitude scores between these groups, Euro-descent participants found acupuncture to be more beneficial (m=7.45) than Asian-descent subjects (m=6.84; t[104]=2.08, p=.04) and more favorable (m=7.22, m=6.61, t[104]=2.31, p=.02), respectively.
Study 2
Research indicates that even though participants may rate one message higher on several dependent measures, their ranking the same messages when placed side-by-side could possibly vary. As such, in the pursuit of understanding respondents’ potential preference for one explanation over another, Study Two pitted the two messages against each other for participants to indicate their preferred explanation.
RQ3: Will there be a preference, via ranking, for acupuncture explanations?
Participants
Respondents were two-hundred ten (n=210, females=134, males=65, non-report=11) students at a private western university. Participation in the research was voluntary and all responses were anonymous. The ethnicity composition of this sample, as provided by participants, was: Euro-descent=91, Asian-descent=56, Hispanic= 31, Afro-descent=9, Middle Eastern=4, Multi-Mixed-descent=8, Undisclosed=11. Participation in the research was voluntary and all responses were anonymous.
Materials and Procedures
Participants were given one of four protocols. The protocol either had the TCM explanation first with the Western version immediately following, or visa versa to control for order effects, and attributed to “Dr. Woo” or “Dr. Wood”. Respondents were asked, simply, to rank their preference of explanation by putting a “1” in front of their preferred explanation, and a “2” in front of their second choice after reading the explanations of acupuncture.
Foot Notes
1 This investigation was considered exempt by the Institutional Research Board (IRB).
Results
Findings suggest that the Western explanation was overwhelmingly preferred (70%, n=147), with the Traditional Chinese Medicine explanation receiving the remaining 30% (n=63) of the first place rankings (RQ3). Moreover, 73% of the female respondents as compared to 62% of the male respondents ranked the Western explanation as their preference over the TCM explication. There was no evidence for a preference for the ethnicity of doctor (RQ2) doing the explaining or difference in rankings based on participant ethnicity.
Table 1: Between Group Means – Study One.
Discussion
This investigation queried whether research participants would have a preference for either of two explanations of acupuncture -- Traditional Chinese Medicine or Western Medicine. In addition, the question of whether the ethnicity of the doctor doing the explaining -- Chinese or Euro-descendent -- would be a factor in participants’ rankings of explanations. It was found that the Western Medicine explanation was more highly preferred, via ratings and rankings, over TCM’s version of how acupuncture functions. There was no preference found for an explanation based on the ethnicity of the doctor or participants.
The dominant way in which the Western Medicine explanation was preferred is surprising, given the demographics of where the data were collected (i.e., private California coastal university). One could predict that since acupuncture is Chinese, that the explanation of its originators would hold considerable weight, though much different in world view from Western thought. Alternatively, a case could be made that students studying at a American University, regardless of ethnicity or country of origin, would favor western views. Only an investigation querying the specific ethnicity of research participants, say Euro-descent or Chinese, with accompanying acculturation measures, would best address this issue.
Explaining the nature of acupuncture is becoming an increasingly inherent and critical part nurses’ and other health practitioners’ communicative tasks to patients. In practice, if patients are given both explanations, they can process and ponder the one that makes most sense to their health belief system and work within the framework of the explanations that benefits them most.
Acknowledgement
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
- Barnes PM, Bloom B, Nahin RL (2008) Complementary and alternative medicine use among adults and children: United States, 2007. National Health Statistics Reports 12: 1-23.
- Burke A, Upchurch DM, Dye C, Chyu C (2006) Acupuncture use in the United States: Findings from the National Health Interview Survey. J Altern Complement Med 12(7): 639-648.
- Edwards E (2009) Millions embrace acupuncture, despite thin evidence. Washington Post HEO4.
- Jastrowski Mano KE, Davies WH (2009) Parental attitudes toward acupuncture in a community sample. J Altern Complement Med 15(6): 661-668.
- Difference Between a Naturopath and Naturopathic Doctor. Very well health.
- Schreiber L (2005) The importance of precision in language: Communication research and (so-called) alternative medicine. Health Commun 17(2): 173-190.
- Whiteford S (2003) Communication growth promotes business growth: Recommendations for enhancing communication skills. California Journal of Oriental Medicine 14(2): 22-23.
- Wu J, Lu Z, Hayes M, Donovan D, Lore R (2009) Integration of acupuncture into family medicine teaching clinics. J Altern Complement Med 15(9): 1015-1019.
- Xu H, Chen K (2011) Acupuncture: A paradigm of worldwide cross-cultural communication. Chinese J Integr Med 17(3): 163-165.
- Karanikas M (1997) Describing acupuncture: A new challenge for technical communicators. Journal of Technical Writing and Communication 27(1): 69-85.
- Anand K (2003) Explaining how acupuncture works. Acupuncture Today 4(5): 1-2.
- Evans M, Paterson C, Wye L, Chapman R, Robinson J, et al. (2011) Lifestyle and self-care advice within traditional acupuncture consultations: A qualitative observational study nested in a co-operative inquiry. J Altern Complement Med 17(6): 519-529.
- Suarez-Almazor ME, Looney C, Liu Y, Cox V, Pietz K, et al. (2010) A randomized controlled trial of acupuncture of osteoarthritis of the knee: Effects of patient-provider communication. Arthritis Care Res (Hoboken) 62(9): 1129-1236.
- Christensen L (2010) Talking to patients about what to expect from acupuncture. Acupuncture Today 11(2): 1-3.
- Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Delaney K, et al. (2010) Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine (Phila Pa 1976) 35(15): 1471-1477.
- Bishop FL, Massey Y, Yardley L, Lewith GT (2011) How patients choose acupuncturists: A mixed-methods project. J Altern Complement Med 17(1): 19-25.
- Mavis B, Vaslienko P, Schnuth R, Marshall J, Jeffs MC (2005) Female patients’ preferences related to interpersonal communications, clinical competence, and gender when selecting a physician. Acad Med 80(12): 1159-1165.
-
Bryan B Whaley* and Michael J Ng. Explaining Acupuncture: Testing Traditional Chinese Medicine versus Western Biomedicine Explications. On J Complement & Alt Med. 8(2): 2023. OJCAM.MS.ID.000685.
-
Explaining illness; Acupuncture; TCM; Western Medicine; Acupuncture practice; Health practitioners; Complementary and alternative medicine; Allopathic medicine; Traditional Chinese Medicine; Western biomedical; Acupuncturists
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






