 Review Article
Review Article
Fashionability and Comfort: Designing Chemotherapy Uniforms to Enhance the Well-Being of Patients and Oncology Nurses
Dana Connell1* and Amanda Huff2
1Columbia College Chicago, USA
2RUSH University Medical Center, USA
Dana Connell, Associate Chair, School of Fine and Performing Arts, Columbia College Chicago, USA.
Received Date: April 02, 2019; Published Date: April 17, 2019
Abstract
In the United States, oncology nurses handling and administering chemotherapy drugs to cancer patients wear personal protective equipment (PPE). The recommendations for PPE gowns, designed to protect from potentially harmful spills, are consistent across several groups including the National Institute for Occupational Safety and Health (NIOSH), Occupational Safety and Health Administration (OSHA), and the American Public Health Association (APHA). Each disposable gown is one-size-fits-all, made of lint-free, low-permeability fabric, such as materials coated with polyethylene. Gowns have a solid front, long sleeves, and ribbed cuffs with a closure in the back. Though the safety of the staff that administers the drugs is paramount, equally important is the response of the patient to the nurse’s appearance. Patients receive chemotherapy wearing street clothes in an outpatient setting. When the nurse approaches shrouded in a noisy, somewhat monstrous uniform, the overall effect can be alarming. Additionally, nurses interviewed about their experience complain that the gowns are uncomfortable and hot. This paper conjectures that the comfort and ease of both nurses and cancer patients might be greatly enhanced through attractive user-friendly garments, made of breathable, washable textiles in adjustable sizes. In a faculty-led design challenge using a technician-safe, patient-friendly paradigm, students in a fashion design program at a mid- western college developed solutions that might improve the comfort level of all concerned, demonstrating that fashion plays an important role in more places than a catwalk or glossy magazine.
Introduction
The World Health Organization reports the incidence of cancer is projected to increase by 70% over the next 20 years, adding to the already 14 million people diagnosed and 8.2 million deaths in 2012 [1]. While progress has been made in the reduction of some cancers, other cancers are on the rise. Increases in cancer incidence are projected worldwide due in large part to the aging population. Researchers also point specifically to the high incidence of cancercausing behaviors including smoking, alcohol use, and sedentary lifestyles [2]. The growing number of cancer patients has given rise to additional ambulatory care cancer treatment centers both in traditional hospital settings and specialized cancer treatment centers.
Ambulatory care facilities and cancer treatment hospitals have benefitted from a boom in building new and improved healthcare facilities. Healthcare facilities have become significantly more customer-centric; hospital designers now seek “evidence-based design” of healthcare facilities. This approach is proving beneficial to patients and providers. Hamilton K [3] has resulted in healthcare facilities with dramatic improvements in function and comfort. Leading facilities such as the Dana-Farber/Brigham and Women’s Cancer Center (DFCI) in Boston, Massachusetts have advanced by engaging patients and families in building decision making. After a tragic chemotherapy overdose, DFCI instituted a patientfamily advisory council who, among other topics, participated in the planning and renovation of chemotherapy administration areas [4]. While evidence-based design has improved patient and healthcare provider outcomes through the physical environment, there remains work to be done to improve the nurse and patient interaction, specifically the uniform.
Meeting Needs of the Healthcare Provider and Patient
The administration of chemotherapy or antineoplastic drugs brings risk of exposure. Such exposure is most often through inhalation, dermal, or oral means. Inhalation is generally through exposure to droplets, particulates, and vapors. Highest risk of dermal exposure occurs when workers touch contaminated surfaces during the preparation, administration, or disposal of hazardous drugs [5]. Cancer treatment nurses in the United States are required to wear PPE when administering chemotherapy drugs. Such requirements are consistent across several groups, including the National Institute for Occupational Safety and Health (NIOSH), Occupational Safety and Health Administration (OSHA), and American Public Health Association. The PPE is intended to protect patients from infection and the healthcare providers against spills and splashes of potentially harmful chemicals contained in the chemotherapy regimens. Chemotherapy regimens are administered intravenously (IV), requiring nurses to handle and mix drugs according to set protocols, manipulate tubing to attach to patients, and in some cases, clean up hazardous medication spills. There are multiple points where exposure can occur during medication administration. These include IV bag leakage or punctures causing medication to spray, system malfunctions, or imperfect connections between the IV bag and tubing or patient IV connection. Grazing against or handling drug vials and bags alone risks exposure with the most common exposure caused by contaminated surfaces where hazardous materials have been previously placed [6].
Protecting the nurse against hazardous chemotherapy drugs is imperative. However, the garment most commonly used lacks comfort, true functionality, and versatility. For many, one-size-fitsall standard garments are too small or too large. According to a 2003 Size USA survey, the average woman is taller, heavier, and a different shape than in years past [7]. In addition, men have added one additional inch for each key measurement in chest, waist, hip, and collar [8]. Uniforms too small or too large encourage providers to prematurely remove the ill-fitting garment which may lead to increased exposure risk. The garment that is too small is difficult to put on and often rips at seams defeating its intended protective purpose and creating waste. The garment that is too large is cumbersome and bulky, impeding the nurse’s movement.
Function is another key issue. When administering chemotherapy drugs nurses may need a variety of additional supplies such as a stethoscope, bandages, scissors, alcohol wipes, gauze, medical tape, phone, and patient identification labels. These supplies are commonly utilized during each patient interaction. A well-designed garment meets both the functional and comfort needs of the user allowing them to effectively and efficiently perform their job. Functional pockets allow for both the storage of supplies as well as the ability to move efficiently.
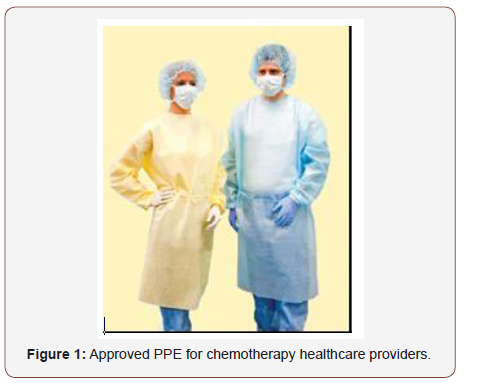
In addition to the fit and function of the garment is the actual “fabric” or textile used in uniform production. An approved uniform, shown in Figure 1, is made of lint-free, low-permeability fabric, such as polyethylene-coated materials. The garment is solid in the front with long sleeves, has a closure in the back, as well as elastic or knit cuffs at the wrist that are tucked under gloves. Though somewhat cost-effective, the fabric is non-breathable resulting in excessive heat and moisture build-up for the wearer. The garment is worn over the provider’s own clothing or hospital-mandated uniform. This single-use disposable garment costs approximately $6.45 per gown according to hospital procurement staff. Costs and discounts vary by supplier. It is recommended that the gowns are removed and discarded if visibly contaminated and upon leaving areas where drugs are mixed, handled, and administered [6].
The PPE is also designed to protect providers and patients from infectious diseases which threaten the well- being of all inside a healthcare facility. Recent decades have seen healthcare workers shrouded in protective gear during SARS, H1N1, and most recently Ebola outbreaks. A recent competition led by Johns Hopkins University. Paul S [9], cited a need for improved uniforms and suits to protect against disease and provide comfort and function, while also considering the patient response. Fear, anxiety, and discomfort may overcome the patient as a provider approaches in the noisy, poorly designed garment. There has yet to be a standard adopted across the board, however the 2014 NIOSH update “contains recommendations for the use of personal protective equipment (PPE) in specific situations” [10]. It would be beneficial if one standard were followed by each governing body to ensure a PPE developed is safe, functional, and policy-fulfilling.
Extensive studies of evidence-based facility design have resulted in 21st century design practices that are aesthetically pleasing and comfortable for patients and staff [11]. Researchers from Texas A&M and Georgia Institute of Technology identified 600 studies with evidence that improved hospital facility design can be “safer, more healing, and better places to work [12]. They cite four specific areas where evidence- based facility design can impact patients and staff:
1. Reduce staff stress and fatigue and increase effectiveness in delivering care
2. Improve patient safety
3. Reduce stress and improve outcomes
4. Improve overall healthcare quality
Poor uniform design threatens to reverse these positive impacts. It could be conjectured that the millions of dollars spent on the well-designed physical environment are significantly reduced by the current PPE. The PPE is in direct conflict with the comfortable chairs, calm lighting, music, and special warming blankets, all designed for calm and healing in the facility. Quality of acoustics in healthcare is also linked to healthcare provider pressure and strain. The hospital setting is fraught with unexpected alarms, machinery, audible patient distress, and overhead announcements. The noise encountered by healthcare providers has been shown to impact stress levels. The loud, irritating sound of shuffling paper PPE being worn by multiple providers could have a negative impact on nurses and patients and requires further examination.
It is important to also consider the patient perspective. As the patient sits in street clothes receiving a chemotherapy infusion, an enshrouded provider stands over, adding to the anxiety and fear of the illness. In one large metropolitan Chicago hospital, nurses suggest that one out of every three patients may be negatively impacted by PPE garments in the oncology unit. This information was obtained by a verbal survey of approximately 35 nurses at this particular facility. More research is needed to isolate the physical and psychological impacts of PPE and to formulate a plan to produce further action and change. Such research could offer PPE options for a variety of healthcare facilities beyond oncology.
Environmental Issues
Use of the current single-use disposable PPE in cancer treatment results in additional costs for proper disposal as a medical waste product. One hospital nurse, at the aforementioned facility, verbally estimated in April of 2014, that one nurse will dispose of approximately five PPE gowns within a 10-12-hour shift. The number of disposed gowns is staggering; if, for example, a large metropolitan outpatient clinic utilizes an average of 13 nurses donning five gowns per day in a given shift (1,300 gowns in a year), this totals $419.25 per day and approximately $106,070.25 in PPE gowns per year. These averages might equate to approximately 16,900 gowns, most often lightly used, being disposed of each year in one hospital. Under current guidelines, gowns are to be disposed of in yellow biohazard containers which can cost approximately $30-$50 per bin. If one bin is designated for disposal of gowns alone, an institution could face $15,000 per year to provide one bin per day.
An alternative to the inexpensive yet wasteful PPE is to consider a washable garment. Washable garments allow reuse by providers and minimize environmental impacts of disposal in favor of laundering. In a 2014 study of nonsurgical healthcare attire, only 36% of respondents stated their hospital provided laundering of hospital-issued attire. The study also noted that no difference in home laundered attire compared to hospital laundered attire [13]. Laundering of garments that may be contaminated with chemotherapy drugs brings new wastewater concerns. Such concerns will vary depending on the drugs used. At present, reusable garments are not permitted.
Form Follows Function
In a 2014 pilot study, researchers evaluated spills and exposure to chemotherapy drugs and the impact within the organization. The study revealed that of the 40 participants and spills reported, only 29% wore the PPE uniform. In addition, 60% of those experiencing a spill had little to no level of concern over the exposure. Though limited in participation, the study concludes that: “staff should participate actively in selecting personal protective equipment that balances comfort and safety” [14].
At a large metropolitan hospital in Chicago, healthcare providers echo the need for balancing comfort and safety with function. During initial interviews, nurses cited multiple problems with the current single-use PPE uniform. The current uniforms lack multiple pockets, which would enhance the functionality of the uniform and allow workers to have ready all of the tools necessary to administer chemotherapy drugs. The single-use uniforms are made of a paperlike polyethylene-coated material which nurses state easily rip or tear with weighted objects placed in and out of a pocket. Nurses are often forced to make multiple trips to the supply area or worse, defeat the purpose of the uniform by placing these objects in the pockets of their underlying street clothes. The polyethylene- coated material is non-permeable and consequently non-breathable. The uniform worn over street clothing or medical scrubs leaves the nurses overheated and anxious to remove the garments. The gowns are cumbersome to don and virtually impossible to put on quickly in case of an emergent situation. When surveyed, the most common complaint from nurses was that the gowns seem to be designed with only the male form in mind. This includes broad space in the shoulder areas and a straight waist down past the knees. Due to the excess material and poor overall fit, most female wearers end up with excessive perspiration and overheating. This overheating can compromise safe and quality care of patients due to the nurse being focused on the fastest route to gown removal.
For those on the small end of the scale, the garment billows and rustles as a large paper sack tied at the waist. Conversely, for those at the larger end of the scale, the garment is tight and restrictive. Tight, ill-fitting garments are more susceptible to stressed seams which are easily ripped or torn when worn. It should be noted that these uniforms are made in more than one size. It isn’t known what the decision-making path entails; however, procurement of a single size garment may stem from supply chain efficiency and cost effectiveness for inventory management.
The current PPE gowns worn by chemotherapy nurses serve an essential role in protecting workers from hazardous chemicals during infusion. However, these costly, disposable gowns pose a threat to the overall care provided when workers are anxious to remove the garment, the environment, and the psychological wellbeing of the patient.
Designing a better uniform: A pilot study
Students in a Chicago fashion design Bachelor of Fine Arts program entered a 2013 challenge to create a better uniform. The winning design was awarded $200. The challenge was to address the fit and functionality of the current PPE uniform. Nurses at a Chicago hospital oncology unit were interviewed by the faculty advisor to gather information for the design brief. One question and answer session were held between participants and a healthcare provider. The purpose of this session was to provide clarity on the needs as well as the regulatory limitations imposed by NIOSH and OSHA. Of key concern for nurses was breathability of the fabric and garment, pockets to hold essential work tools, and sizing. Students designed uniform ideas using a flat sketch format. After two weeks, sketches were submitted for review by the faculty and oncology nurses at the Chicago hospital (5 reviewers total). Parameters for the PPE uniform design were outlined for the students in the design competition.
The design shown in Figure 2 was the winning design. While it did not meet the requirement of covering to the neck, this design did meet most other criteria. This design was clean, functional, easy to put on and take off, and presented in a professional manner. The additional designs shown in Figure 3 had some desirable features that may be useful in future designs. In particular, under arm gussets made of layered mesh to provide breathability showed promise while the notion of an apron style layering piece was also an interesting solution. The competition design brief is shown in Figure 4.
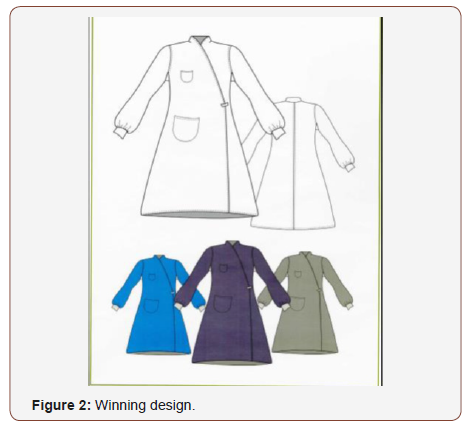
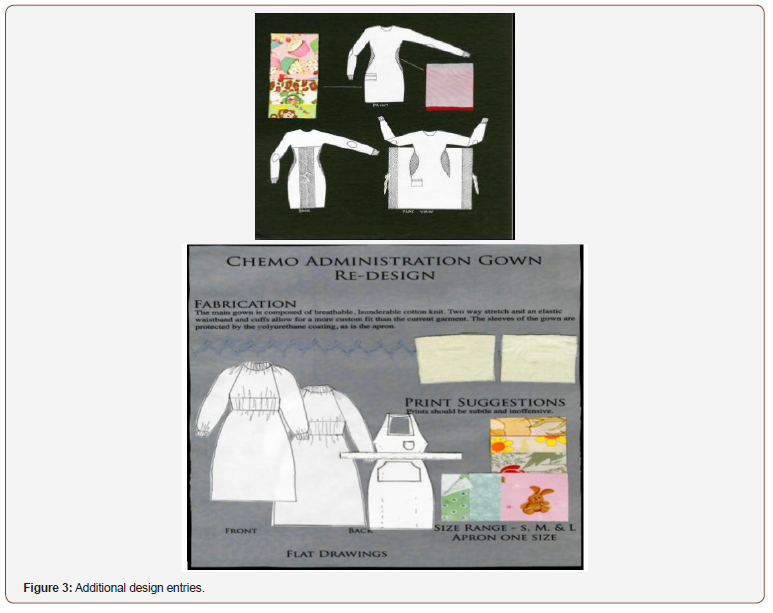
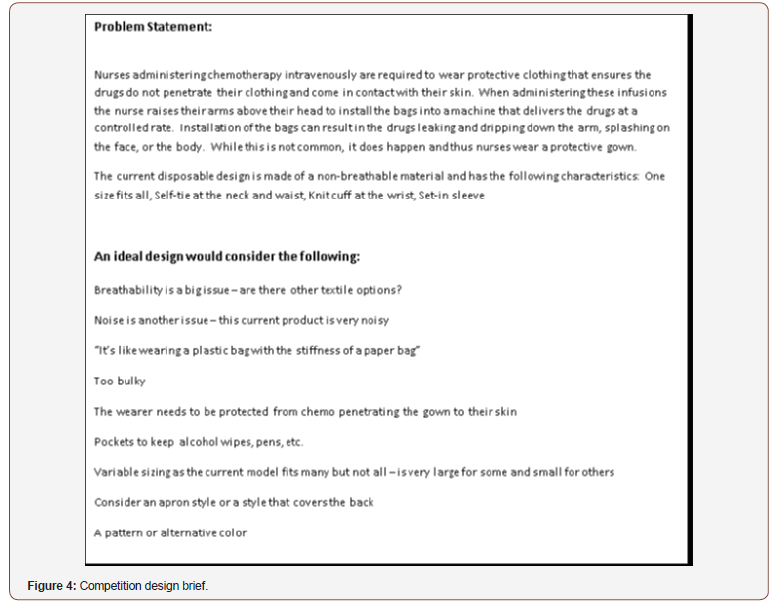
Table 1:Basic specifications of conductive wire.
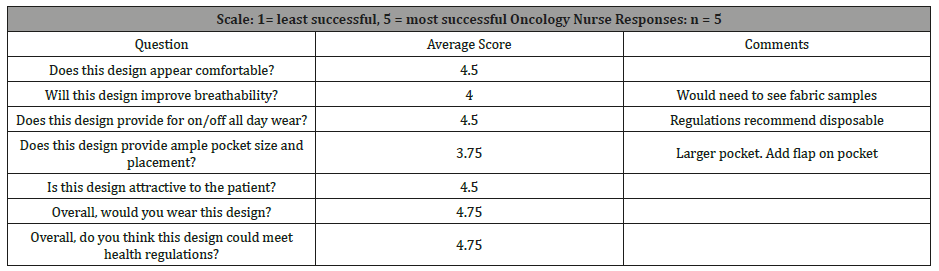
Students focused on each of the area’s nurses noted as needing improvement. All designs included a pocket, although in some the pocket was too small. Fabrics improved breathability, and garments were offered in multiple sizes. The competition was limited in fabric selection and requires further investigation. However, students did consider variations in style, color, and pattern towards a more fashionable textile. Following the design submission, nurses were given a brief survey to score the designs and provide feedback for six questions. Table 1 represents their collective responses. Overall results of the design challenge were positive with an average score of 4.75 of 5 in effectiveness of the winning design. The area needing most improvement was in pocket size and functionality, scoring 3.75.
Conclusion and Recommendations
The design challenge highlighted the need to address PPE in healthcare and specifically, oncology. Using evidence-based uniform design can improve satisfaction for providers and patients alike. The recent design challenge by Johns Hopkins University to design a better Ebola suit [9] signifies a need towards improved safety while also considering the impacts on patient perceptions of disease and quality of care. As recommended in the 2015 pilot study by Friese et al., healthcare providers can impact garment design by making recommendations for a uniform that is not only functional but also properly fitting with some element of style. Additional research areas should include a well-designed survey for nurses at multiple facilities of varying size and structure. Such a survey should explore the variations in facility PPE uniform protocol. Patient surveys are also necessary to fully understand the impact of PPE on patient psychological well-being and overall response to treatment.
Designing a better uniform will need to focus on both female and male healthcare providers. In 2011, the U.S. Census reported that 91% of U.S. nurses were female [15]. With just 330,000 male healthcare providers in nursing it is evident that most nursing specific, non-PPE, uniform designs should be geared towards female users. And yet, PPE is designed as a one-size garment more likely to fit males. There is evidence that male providers are on the rise indicating that uniform designs might be androgynous in nature but take into consideration body size and shape for improved fit. Androgynous designs geared to shape and overall size have the opportunity to improve overall comfort and functionality.
Beyond the human implications of the PPE are the textile advancements that are in rapid development. Issues of permeability, breathability, and stretch for improved fit are all possibilities in the future of textiles. There are a plethora of technical textiles advancing the industry and poised for growth in a variety of fields including medicine [16]. Identifying possible textiles for use is a first step in improving the uniform for healthcare workers. The future might provide new opportunities where function and fashion meet in the medical field.
pThe use of color and pattern in healthcare uniforms has expanded from solid color white traditional garments to a wide variety of patterns, colors, and styles. The current PPE uniforms are typically a medium blue or yellow solid color. Occasionally other solid colors such as aqua or green are seen. Textile design could incorporate designs that are patient-friendly while also meeting the professional needs of the provider and the facility.The PPE uniform also indicates a need for a business case study to analyze the cost effectiveness of disposable versus washable uniforms. Such research would explore the costs associated with hazardous waste disposal and laundering. Additionally, overhead costs and inventory management would need to be addressed. Together, surveys, personal interviews, and design challenges each offer insight and improvement to the current PPE in healthcare.
Limitations
The outcomes of this paper are limited to the experiences of one large mid-western Chicago hospital cancer center and limited participation by healthcare providers. Participants were from one unit within the cancer center and did not include comprehensive feedback and analysis. Background knowledge also played a key role in the limitations of the design challenge as the student’s point of view was from a functional fashion aesthetic.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Kate T (2014) NIOSH Revamps Hazardous Drugs Uptake. American Journal of Health-System Pharmacy News.
- Friese CR, McArdle C, Zhao T, Sun D, Spasojevic I, et al. (2015) Antineoplastic drug exposure in an ambulatory setting: a pilot study. Cancer Nurs 38(2): 111-117.
- Dhanabalan V (2014) Waterproof breathable fabrics: Technologies and practices.
- Conway J, Johnson B, Edgman-Levitan S, Schlucter J, Ford D, et al. (2006) Partnering with patients and families to design a patient- and familycentered health care system: A roadmap for the future, A Work in Progress.
- Zernike K (2004) Sizing Up America: Signs of Expansion from Head to Toe. The New York Times.
- US Census Bureau. Social, Economic, and Housing Statistics Division. Industry and Occupational Statistics Branch (2013) Men in Nursing Occupations: American Community Survey Highlight Report, by Liana Christin Landivar.
- Connor TH, McDiarmid MA (2006) Preventing occupational exposures to antineoplastic drugs in health care settings. CA Cancer J Clin 56(6): 354-365.
- Bolton DL, Seth Eisenberg, Glynn-Tucker EM, Howard-Ruben J, McDiarmid MA, et al. (2011) Safe Handling of Hazardous Drugs, edited by Martha Polovich. Pittsburgh: Oncology Nursing Society.
- Paul S (2014) Improved Suit for Ebola Caregivers Chosen for Funding in Federal Competition.
- Leather P, Beale D, Santos A, Watts J, Lee L (2003) Outcomes of environmental appraisal of different hospital waiting areas.” Environment and Behavior 35(6): 842-869.
- Bearman G, Bryant K, Leekha S, Mayer J, Munoz-Price LS, et al. (2014) Healthcare personnel attire in non-operating-room settings. Infect Control Hosp Epidemiol 35(2): 107-121.
- Newcomb B, Istook C (2006) Using Size USA to Improve Apparel Fit. Annual meeting for the International Foundation of Fashion Technology Institutes, North Carolina University.
- Ulrich R, Quan X, Zimring C, Joseph A, Choudhary R (2005) The Role of the Physical Environment in the Hospital of the 21st Century: A Once-ina- Lifetime Opportunity.
- Steward BW, and Wild CP (edts) 2014. World Cancer Report. Lyon, France: World Health Organization, International Agency for Research on Cancer.
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61(2): 69-90.
-
Dana Connell, Amanda Huff. Fashionability and Comfort: Designing Chemotherapy Uniforms to Enhance the Well-Being of Patients and Oncology Nurses. J Textile Sci & Fashion Tech. 2(3): 2019. JTSFT.MS.ID.000538.
-
Fashionability, Designing, Chemotherapy, Oncology nurses, Permeability, Fabric, Polyethylene, Gowns, Ribbed cuffs, Alarming, Garments
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






