 Research Article
Research Article
Evaluation of Adherence to the Guidelines of Clinical Practice of Vascular Lines by the Nursing Staff of the UMAE H.E. N.- 14 C.M.N. “A.R.C.” Veracruz Norte
José María Domínguez Ruíz1* and Esther Hernandez Martinez2
1Calle Delia De La Paz, Fracc. Villa Rica, N- 335, Veracruz, Mexico
José María Domínguez Ruíz, Calle Delia De La Paz, Fracc. Villa Rica, N- 335, Veracruz, Mexico.
Received Date: March 17, 2019; Published Date: April 18, 2019
Abstract
Introduction: Clinical practice guidelines are proposed to improve the quality of care. Its purpose is to establish a national reference to guide the making of clinical decisions based on recommendations based on the best available scientific evidence. The perspective of nursing in the 21st century is that all nurses look for evidence and apply it in their daily practice, in order to reflect on the assumptions considered as true and that guide the practice of day-to-day life, and which the impact and results of these interventions are routinely evaluated on patients.
Objective: To analyze the attachment to the prevention, diagnosis and treatment of infections related to vascular lines according to the recommendations of the clinical practice guide in the nursing staff of the intensive care unit in the High Specialty Medical Unit Number 14.
Material and methods: Observational, prospective and cross-sectional study, through review of 112 clinical files of patients with central venous catheters of the intensive care unit in the highly specialized medical unit number 14 Veracruz, Veracruz, Mexico, from August 2017 to November 2018. Incomplete files were excluded. To evaluate the adherence according to the recommendations of the clinical practice guideline, the single card of prevention, diagnosis and treatment of vascular-related infections was used, an adequate adherence was considered greater than 80%.
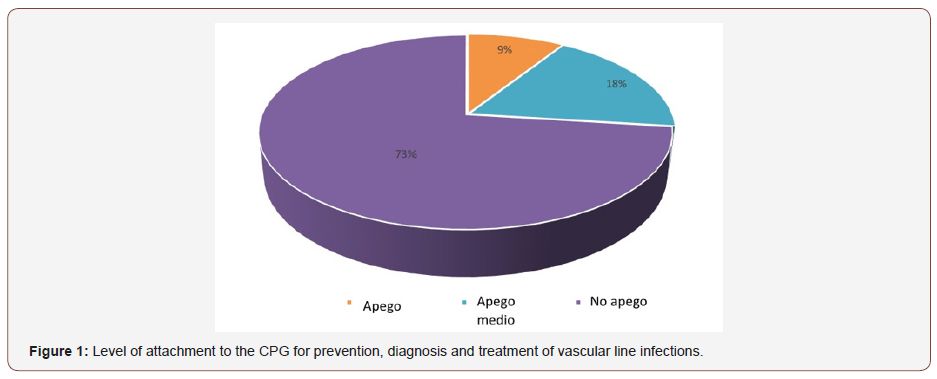
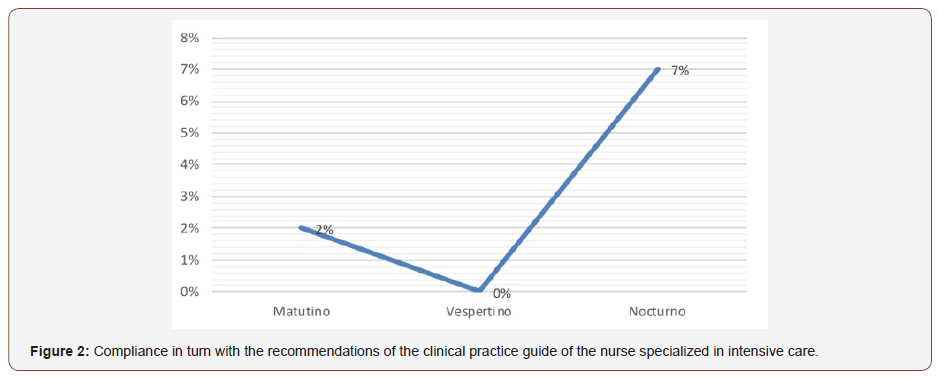
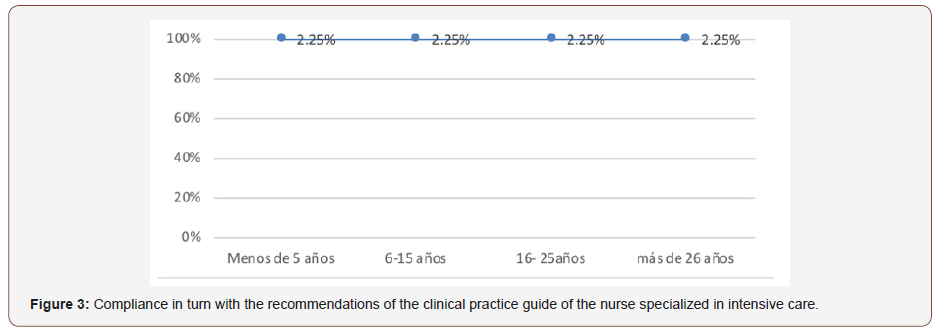
Results: It was discovered that 73% did not adhere to the recommendations of the clinical practice guide, while 18% had medium attachment and only 9% had attachment. Of this percentage, 7% corresponds to the night shift, with the evening shift being the one that does not show adherence to the recommendations. 9% attachment for seniority: less than 5 years (2.25%), 6-15 years (2.25%), 16-25 years (2.25%), more than 26 years (2.25%).
Conclusion: There is a need to continue with the continuous training and it is suggested to carry out an educational intervention to later evaluate in order to improve the results. It follows that no personal impulse has been shown in the research development on the subject.
Keywords: Attachment; Clinical Practice Guideline; Vascular line management; Evaluation of adherence
Introduction
The epidemiological profile that currently characterizes the national health system is dominated by diseases that are difficult to manage, as well as injuries generated by determinants of a complex nature related to both the living conditions of society and the abilities of people to make decisions. in favor of your own health and that of yours. As part of the use of high technology, the use of intravascular catheters is a fundamental tool in the monitoring and treatment of patients admitted to health institutions, regardless of the complexity of their condition; they are of vital importance especially in those that are in critical condition [1].The use of venous catheters is relatively recent, they appear in the literature in the year 1900 and in 1929, Werner Fossmann underwent central venous catheterization with cadavers, until 1957 Ross introduces the basic principles of intravenous therapy. However, in 1970, Swan The epidemiological profile that currently characterizes the national health system is dominated by diseases that are difficult to manage, as well as injuries generated by determinants of a complex nature related to both the living conditions of society and the abilities of people to make decisions. in favor of your own health and that of yours. As part of the use of high technology, the use of intravascular catheters is a fundamental tool in the monitoring and treatment of patients admitted to health institutions, regardless of the complexity of their condition; they are of vital importance especially in those that are in critical condition [1].The use of venous catheters is relatively recent, they appear in the literature in the year 1900 and in 1929, Werner Fossmann underwent central venous catheterization with cadavers, until 1957 Ross introduces the basic principles of intravenous therapy. However, in 1970, Swan
Historically, intravenous infusion therapy has contributed, in an important way, in the development of better treatments for health care. However, this procedure also poses serious risks for patients and for health service providers, since hospital stay (bed days) and spending due to adjacent complications are increased. The world literature has extensively described infectious complications and other problems such as extravasation, infiltration and occlusion, as a threat to the integrity of the patient because when they worsen, they are associated with considerable morbidity and an increased risk of death[4].Infections associated with a central catheter account for 10% of hospital infections; being the skin, the hematogenous route, the contamination of the connection system, the use of solutions and / or contaminated food, some of the routes by which they are produced. The incidence of infections associated with the vascular catheter varies depending on factors of the host, the catheter and its handling. There are specific factors described that correspond to the catheter, its location, the method of installation, the nature of placement in an emergency or elective situation, the number of lumens, the duration of catheterization and the characteristics of the host. Infections related to these vascular accesses increase morbidity, mortality, days of hospitalization and, consequently, costs for both the patient and the institutions. Therefore, they must be used under certain criteria, with infectious norms, assessing the particular benefit cost of each patient, since it is not a procedure free of other complications, risks and / or adverse events. The World Health Organization has shown that the prevention and protection of those risks that may endanger the well-being and life of the patient can be diminished through the implementation of checklists during the surgical act. In the same way, the consequences of those events that we must assume inevitably can be reduced. It is essential to have a prospective surveillance system for the assessment of infections and adverse events associated with vascular catheters. Thus, a checklist of patient safety with central venous catheter was implemented, which covers the procedure and follow-up of the patient with CVC; with the intention of improving the quality of care, providing patient safety, and reducing morbidity and mortality as well as hospital stay and health costs [5].
Approximately half of patients with an acute or chronic disease, carry some type of central venous catheter, some factors that increase the risk of infection are beyond our control, for example: patient’s immune status, base pathology and extreme ages. Central venous catheters are associated with a higher incidence of serious infections than short peripheral catheters, with the microorganisms commonly isolated being Staphylococcus Epidermis, Staphylococcus aureus, Escherichia coli and Pseudomona sp. In prospective studies the risk for a catheter-related infection is 2 to 855 times higher with central venous catheter. The cost that generates a hospital only in an intensive therapy in the United States of America each year is $ 296 million to 2.3 trillion dollars. Bloodstream infections continue to increase despite preventive recommendations and published guidelines, by professional organizations such as Centers for Disease Control (CDC), Nurses Society and Oncology Nursing Society.6 However, nursing professionals who are In the care of patients, they are challenged to avoid as much as possible the risks that contribute to a nosocomial process, always ensuring the safety of the patient through systematic care, such as catheter placement, maintenance and removal. The above reflects that the nursing staff must have competence, skill and knowledge to apply the various techniques and procedures immersed for a good maintenance of central vascular access so it is considered essential to homogenize the procedures and institutional criteria that guide and facilitate the work of the personnel in charge of these activities within the hospitals [6-7].
The main complications related to the insertion of central venous catheters are divided into mechanical and infectious, highlighting the infectious ones due to their impact on morbidity and mortality and the associated costs. The types of infection associated with the catheter have been established by the CDC. They can be local or systemic, and the latter result in serious complications such as endocarditis, meningitis, osteomyelitis or septic shock. Its incidence varies between the different hospital centers; According to the Spanish study of prevalence of nosocomial infections (EPINE) in 2010, catheter-related bacteremia (BRC) is the fourth most frequent nosocomial infection, with a prevalence of about 2 episodes per 100 patients with central venous catheter (CVC). In the vast majority of cases (> 75%) the causative organism is a positive gram, followed by the gram negative (10-15%) and yeast (5-10%). The first measure to avoid them is their prevention, so that a trained team can reduce the incidence up to 7 times. The procedures that have been shown to have the greatest impact on the reduction of catheter-related infections are hand hygiene, the use of maximum aseptic barriers during insertion, and asepsis of the skin at the insertion site with 2% chlorhexidine and before each manipulation of it. The diagnosis of BCR requires the isolation of the causative organism in a peripheral blood culture as well as a blood culture from the central line or in a segment of the catheter (Maki’s technique). There is a high suspicion that the bacteremia comes from the catheter if in the blood culture of the catheter grows a quantity of colonies more than five times higher than the peripheral blood culture. The best sign that the infection comes from the catheter is the culture of the tip with more than 15 colony forming units (CFU) [8].
Bacteremia are infections associated with frequent healthcare, in critical patients they represent a serious complication that can negatively affect the patient’s prognosis. They can be primary or secondary. Primary bacteremia occurs in the absence of another concomitant infection with the patient, is known as bloodstream infection, while secondary bacteremia occurs in the presence of a concomitant severe infection, in these cases the etiological agent most often involved is Escherichia coli, which is the first cause in bacteremia acquired in the community, and the third most common in nosocomial bacteremia. However, there has been a worldwide increase in bacteremia caused by other Enterobacteriaceae, such as Klebsiella spp. It is a recommended study to confirm a bacteremia when it is suspected in patients with or without an obvious source of infection, a positive blood culture suggests a definitive diagnosis in the orientation of an effective therapy against specific manganisms. In the United States, Staphylococcus aureus represents the highest frequency, followed by negative coagulase Staphylococcus and Enterococcus spp. In Latin America, the microorganisms that are most isolated are Staphylococcus aureus, Escherichia coli, Coagulase-negative Staphylococcus, Klebsiella pneumoniae and Pseudomonas aeruginosa. Also, in Mexico and Argentina are Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, Klebsiella pneumoniae and yeasts. The bloodstream infections are very important, because their mortality ranges between 13.6 and 38% [9-10].
The Center for Disease Control and Prevention (CDC) currently refers to nosocomial infections as Health Care Associated Infections (IACS), a localized or systemic condition resulting from an adverse effect in the presence of an infectious agent or its toxins. , acquired in a hospital environment during the course of a treatment for another medical condition, since, it may occur due to any procedure performed within the processes of health care, whether diagnostic or therapeutic. The global panorama is reflected in studies such as the one conducted by the World Health Organization (WHO) in 55 hospitals in 14 representative countries of 4 regions of the world (Europe, Eastern Mediterranean, Southeast Asia, and Western Pacific) through of a prevalence survey, which showed that, on average, 8.7% of hospitalized patients had intrahospital infections[11].
Study carried out in the adult intensive care unit in Bogotá, where they found rates of bacteremia associated with a catheter from 12.4 to14.9/1000 catheter days and in the epidemiological bulletin of the District Department of Health of 2013 reported rates of infection of the catheter-related bloodstream in the ICUs of Bogotá in 2013. The incidence is related to the effectiveness of nosocomial infection control programs as reported in the National Cancer Institute (INCAN) with an incidence of 2 episodes. 1000 days catheter [12].
The nursing professional plays a transcendental role in the management of intravascular devices, such as peripheral venous catheters, central venous catheters and long-stay venous catheters. Their participation is fundamental due to the increasingly frequent use of catheters for the diagnosis and curative or palliative treatment of the ailments. Their interaction with these devices is intimately related to the care that this professional provides during the insertion, maintenance and removal of these [13]. The methodological manual for the development of nursing clinical practice guidelines for the national health system states that the Clinical Practice Guidelines (GPC) encourage a reflective practice that discards routines, unfounded opinions and intervention based on intuition. The contribution of nursing based on evidence (EBE) through the CPG implies an active participation of the nursing professional in the decision making process in the choice of the best care for a specific patient and leads to a lower variability in the reflective clinical practice, as part of the culture of quality of care; for this reason it is important to emphasize that what is intended with the CPG is not to make the activities routine, but to develop in the health professionals a critical judgment, which allows them to make the best decision according to the needs, characteristics and individual clinical circumstances of the user [14].
Nursing is the professional of care and its basic principle is to protect the patient from diseases that are not the cause of his admission to the hospital so he must support the care on a scientific basis. The effectiveness of the implementation of catheterrelated infection prevention programs has been demonstrated through prevention packages and work procedures in insertion, maintenance, permanent attention and prevention of adverse events in vascular access, for example , CPG as evidence and recommendations developed through the systematic review of the medical literature with the aim of guiding the nursing professional to contribute to safe and quality care, through critical and reflective practice[15]. Studies carried out by different researchers have documented that nosocomial infections are an important cause of morbidity and mortality, in addition, they are considered endemic or epidemic diseases, affecting both developed and resource-poor countries, thus constituting an important public health problem at the national level. worldwide, not only for clinical but also economic reasons [16]. Due to the manipulation of these catheters, the nursing professional has a degree of responsibility required for health care with quality carried out in a judicious manner, so that the health professional must gather knowledge and skills that allow him to manipulate Vascular lines correctly[17]. Escobar Carmona et al. Carried out a work to determine the adherence to the clinical practice guide of prenatal control with a risk approach in pregnant patients of the FMU no.1 [thesis]. Mexican Social Security Institute. Orizaba Veracruz. January 2014, finding that in 94% they had a specialty they identified the risks for CKD, concluding to the conclusion that the addiction was 65% [18]. Oñate Ramírez and Rendón Macías investigated the attachment to clinical guidelines for the management of bronchiolitis found in 197 children that the attachment is good but that it is still necessary to establish the need to stick to these[19].Sámano Heras and Pérez Méndez determined the attachment of resident physicians of emergency medicine, to the guide of clinical practice diagnosis and treatment of spontaneous pneumothorax, found that 75.7% have a high level of adherence to this guide [20]. Adame and Reyes evaluated the adherence to the recommendations of the clinical practice guide for the diagnosis and treatment of low urinary tract infection during pregnancy by the first level of care doctor, where he got a bad attachment to the recommendations and evidence of the CPG by 95%. The main inconsistencies were that 90% did not request screening uroculture [21].
While Leyva Rodríguez and Miranda González investigated the attachment of the maternal and child nursing staff of the IMSS to the NOM-007 in the prenatal control, as a result they found that the level of attachment of the maternal and child nurses to the Official Norm 007 was high favoring the quality of attention to this vulnerable group [22]. On the other hand Hernandez Orozco and collaborators measured the attachment to hand hygiene before the patient’s attention, observed an attachment to hand hygiene of 54% in doctors and nurses and 73% in nursing assistants, concludes that the attachment to hygiene of hands is greater in nurses than in medical personnel [23-26].
Methodological Design
Type of study
Descriptive, transversal and prospective.
Universe, sample and sampling
The population of interest was constituted by 112 records of patients with central venous catheter in the intensive care unit, distributed in the morning, evening, night guard A and guard B shifts in the adult intensive care unit, coronary surgeries, medical and kidney transplant of the High Specialty Medical Unit No. 14, Veracruz Norte. From which a sample was calculated for finite populations, with a confidence level of 95% and estimation error 0.05, obtaining a sample of 112 records. The sampling was simple random probabilistic, the inclusion and exclusion criteria for the application of the research instrument were taken into account.
Instrument
The instrument used for its application is that of the gpc attachment checklist and vascular line follow-up code CMGPC IMSS- 273-13; Consider to qualify the following criteria; recommendations fulfilled: YES: 1, NO: 0. Not applicable: N/A. With 20 items divided into two parts, the first part, surveillance of the insertion point with 5 items and the second called care during the infusion of solutions and drugs with 15 items, the percentage of minimum compliance with the recommendations has been set at 80 % which is equivalent to 16 recommendations fulfilled according to the CPG.
Selection criteria
Inclusion criteria: Specialist Nurses, Indistinct Gender, All Shifts, Adult Intensive Care Unit, Post-Surgical Coronary Care Unit, Medical and Kidney Transplant Unit of the High Specialty Hospital No. 14 in Veracruz, Ver.
That accepts to participate in the study and with signed informed consent.
Exclusion criteria: Other categories and that are not in the service at the time of application.
Elimination criteria: Who decide to leave the study and incomplete cedulas?
Independent variable
• Adherence to the clinical practice guidelines for prevention, diagnosis and treatment of infections related to vascular lines.
Dependent variable
• Management of vascular lines.
Study Procedure
The study was conducted during the months October-November 2017, in the services: adult intensive care unit, surgical coronary, medical and kidney transplant of the Hospital of High Specialty No. 14 in Veracruz, Ver. After the authorization of the study protocol by the Sirelcis system, the services were visited starting with the morning, evening and night shift, where the specialist nurses worked and met the inclusion criteria. The purpose of the investigation was explained to them. After they were given informed consent to sign up to participate in the study, at the same time the dynamics and the need to be evaluated by observation were exposed, at the time that the nurses performed the central venous catheter cure or in the moment of manipulation of the catheter, as well as evaluating the clinical records of nursing (the CVC verification and maintenance sheet and the nursing sheet to see if they carry out epidemiological surveillance regarding the registration of the catheter days and if they record the characteristics of the central catheter in the signs and symptoms section. He was made to see that he had the freedom, autonomy and anonymity not to participate in the study if he so decided, that he could leave the study if he wished, without it having an impact on his praxis. They were also informed that whatever the results were, they would not be known to anyone, except to them in an ethical and moral way. At the end, the staff was thanked for their contribution. Once the application of the questionnaire was completed, the information gathered was concentrated in the Excel spreadsheet and SPSS for analysis and interpretation.
Results
The results were analyzed where 45 intensive care nurses were studied, of which 73% were women and 27% men; with a predominant working age between 6 and 15 years with 60% and only 2% corresponded to an age older than 26 years; the majority of nurses studied corresponded to the morning shift with 51%, 27% night shift and 22% the evening shift; in relation to the level of schooling, 93% have Post-technical in intensive care, while 7% have another academic level; According to the result of training in the clinical practice guide for prevention, diagnosis and treatment of infections related to vascular lines, 67% report that they had training and 33% did not have training. Primary tool to be at the forefront with updates to improve the care provided by the nursing professional.
Regarding variable adherence to the clinical practice guidelines for prevention, diagnosis and treatment of infections related to vascular lines, 73% did not become attached, while 18% had medium attachment and only 9% had attachment, as reflected in Figure 1. This is of great impact because it can affect the patient’s improvement and consequently the quality of life of the patients, thereby increasing their long hospital stay and the economic cost involved in the patient, due to the fact that there is no attachment to the national reference.
In relation to the shift that most adhered to the recommendations of the guide of clinical practice of prevention, diagnosis and treatment of infections of vascular lines of 9% of attachment that corresponded 7% to the night shift, being the evening shift the one that does not presents attachment in the recommendations Figure 2.
Regarding percentage of compliance by seniority in the recommendations of the clinical practice guide of the nurse specialized in intensive care. From the 9% attachment for each rank corresponds the following: less than 5 years (2.25%), 6-15 years (2.25%), 16-25 years (2.25%), more than 26 years (2.25%), as shown in Figure 3.
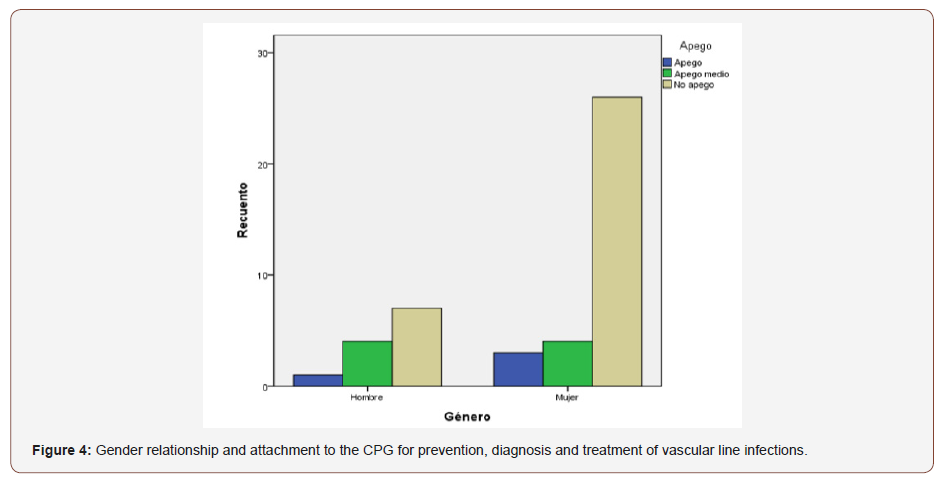
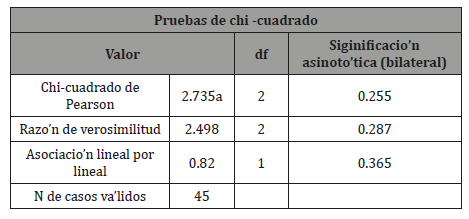
In the gender analysis, no significant difference was observed between women and men in relation to the attachment of the clinical practice guideline X2 (P> 0.05); The antiquity did not show a significant relationship with the adherence to the clinical practice guidelines because an X2 P> 0.05 was obtained. Figure 4.
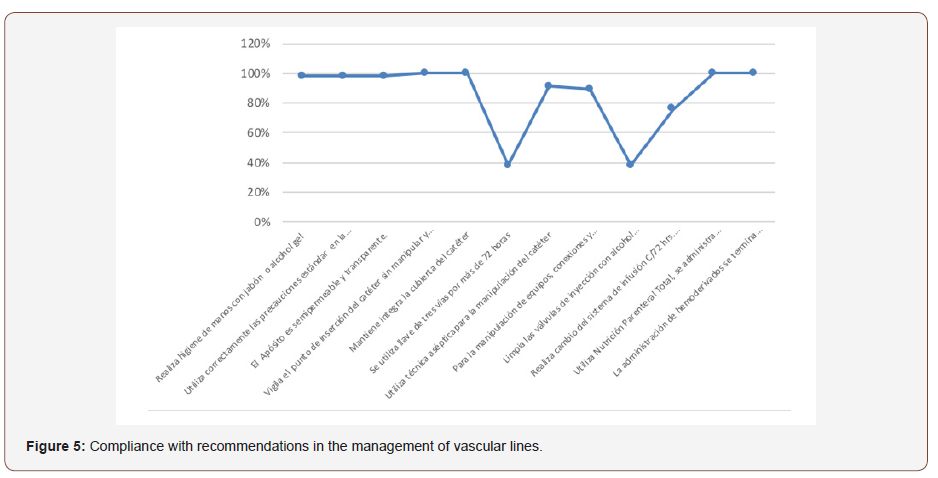
In relation to compliance with the recommendations in the management of vascular lines: it monitors the catheter insertion point without manipulating and removing the dressing, keeps the catheter cover integrated, uses Total Parenteral Nutrition, is always administered by the same lumen of the catheter, the administration of blood products is completed within four hours, verifies and heparinizes lumens at rest, puts a stopper, 100% compliance was obtained, which are listed in table1. While the recommendations: a three-way wrench is used for more than 72 hours and clean the injection valves with 70 ° isopropyl alcohol before accessing them with the system with a compliance percentage of 38%, as shown in Figure 5.
To conclude on the hypothesis, which established that intensivist nurses have attachment to the clinical practice guide of prevention, diagnosis and treatment of infections related to vascular lines. The square chi statistic was applied, it was not significant when relating the variables gender and attachment to the clinical practice guide, we obtained X2 (P> 0.05) between both variables, with this the acceptance of the null hypothesis is supported. Intensivist nurses were not attached to the clinical practice guidelines for the prevention, diagnosis and treatment of infections related to vascular lines Table 2.
Table 1: Compliance with recommendations in the management of vascular lines.
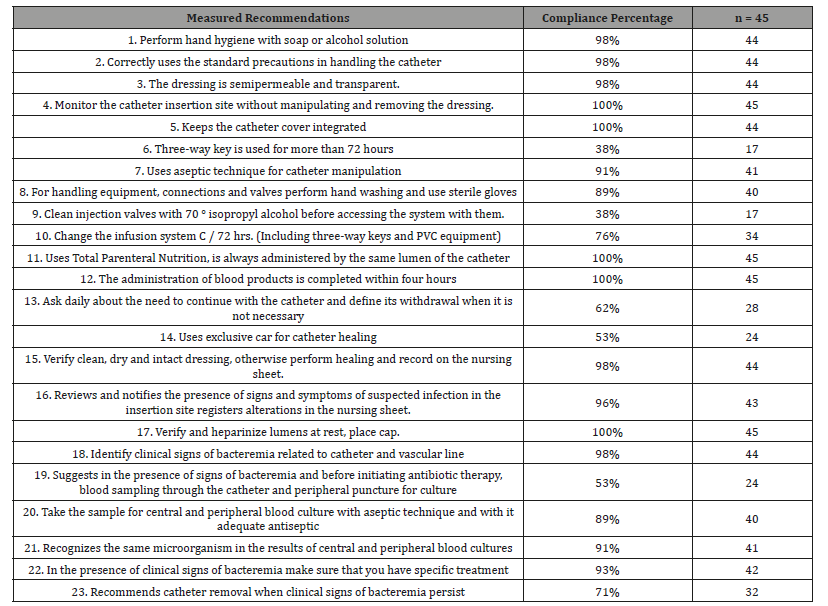
Table 2: Hypothesis test with Chi square (X2), P> 0.05.
Discussion
After the application of the attachment instrument of the clinical practice guide, prevention, diagnosis and treatment of infections related to vascular lines of intensive care nurses of an IMSS of the IMSS. From this study, no reference was found at the national level to another similar one in relation to adherence or not to the guidelines for the practice of vascular lines of intensivist nurses. However, Adame and Reyes evaluated the adherence to the recommendations of the clinical practice guide for the diagnosis and treatment of the lower urinary tract infection during pregnancy by the doctor of the first level of care, where he got a bad adherence to the recommendations and evidences of the CPG in 95%. Which coincides with the results obtained in this study obtaining a 73% non-attachment. Similarly, with Escobar Carmona and colleagues a 65% adherence to the clinical practice guide of prenatal care with a risk approach in pregnant patients. A serious explanation is that the health professional has not been made aware of the importance of the guidelines as a national reference for quality care in patients, since this influences the high rates of bacteremia related to catheters and therefore becomes a public health problem.
While Sámano Heras and Pérez Méndez determined the attachment of resident physicians of emergency medicine, to the guide of clinical practice diagnosis and treatment of spontaneous pneumothorax, they found that 75.7% have a high level of attachment to this guide. Outcome that does not coincide with the present study because they did not adhere to the clinical practice guide, possibly because of the approach applied by the guidelines and by the functions performed by the nursing professional differs from the activities of the doctors. Oñate Ramírez and Rendón Macías investigated the attachment to clinical guidelines for the management of bronchiolitis found in 197 children that the attachment is good but that it is still necessary to establish the need to stick to them.While Leyva Rodríguez and Miranda González investigated the attachment of the maternal and child nursing staff of the IMSS to the NOM-007 in the prenatal control, as a result they found that the level of attachment of the maternal and child nurses to the Official Norm 007 was high favoring the quality of attention to this vulnerable group.
On the other hand, Hernandez Orozco and collaborators measured the attachment to hand hygiene before the patient’s attention, observed an attachment to hand hygiene of 54% in doctors and nurses and 73% in nursing assistants, concludes that the attachment to hygiene of hands is greater in nursing staff than in medical personnel.
As it was observed in the aforementioned studies as part of the medical treatment, it showed a good percentage of attachment, however with the conclusion obtained when performing the study of the attachment to the CPG for the prevention of diagnosis and treatment of infections related to vascular lines was obtained significantly that intensivist nurses do not get attached. The evaluation that took place shows that for prevention as a cornerstone of the being of the nurse, it still requires greater commitment in the performance of the activities with a reference as is the clinical practice guide of this research.
The need to increase the efficiency of the human resource in the intensive nursing area has generated information search guides that guide the staff to act immediately and attached to the same reference that provides quality and warmth to the patient, which is why this study revealed that even with the availability of teaching resources for professional practice there is still a need for continuous training of nurses in the area of intensive nursing. Therefore, it is advisable to carry out an educational intervention once the attachment results have been revealed and then evaluate it again in order to improve the results obtained.
Conclusion
In the realization of this work, it has been observed that there is no attachment of the nurses (os) intensivistas of the guide of clinical practice prevention, diagnosis and treatment of the infections related to vascular lines. No association was found between the shift and the years of seniority with the attachment, it was found that the 9% of attachment that was, was distributed equally in the three shifts. With which it is concluded that there is a need to continue with the training, with the aim of widely disseminating the good practice guide for the management of catheters and thus favor the complete adoption by the intensive care nurses of the guide, since it is a national benchmark and indicator to measure the quality of nursing care.
On the other hand, it can be deduced that no personal impulse has been shown in the research development in the subject, which has influenced the lack of attachment of the clinical practice guide. In the present study it is clearly shown that there are no studies related to the subject at the national level, which concludes that the lack of investigation has concealed the current situation of intensivist nurses in relation to the management of catheters with attachment to a referral with unified criteria that guide professional practice. Due to this situation, the intervention of intensive nursing professionals through an educational intervention in favor of adherence to the guide for the management of vascular catheters is fundamental for improving the quality of care and keeping the patient exempt from compromise. his health due to the mishandling of vascular lines.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Pedrolo E, Marques de lazzari LS, Lemes Rodrigues de Oliveira G, Mingorance P, Reichembach Danski MT (2013) Evidence for nursing care with central venous catheter for short-term stay integrative review. Rev enferm ufpe on line 7 (1): 4199-208.
- Soto Salamanca EP, Suarez Giraldo ML. Practical Nursing Guide for the prevention of infections in patients with central venous catheters. [thesis]. Faculty of Nursing, University of La Sabana, Colombia.
- Parra Flores M, Souza Gallardo LM, García Correa GA, Centellas Hinojosa S (2017) Incidence of infection associated with central venous catheter and related risk factors in patients with total parenteral nutrition in a tertiary hospital. Surgery and Surgeons 85(2): 104-108.
- Ministry of Health (Mexico) Nursing Directorate of the General Directorate of Quality and Health Education. Official Mexican Standard NOM 022 SSA3- 2012. That establishes the conditions for the administration of infusion therapy in the United Mexican States.
- Algieri Rubén D, Ferrante MS, Nowydwor B, Fernández Juan P, Arribalzaga Eduardo B (2013)Implementation of the checklist of the patient with central venous catheter (CVC). Rev argent cir 104 (2).
- Altamirano Rojas J, Flores Mora LF, Rivas Espinosa JG, Torres Mora C (2011) Level of knowledge and application of measures for the maintenance of central vascular access. Rev CONAMED 16(Suppl 1): 17- 21.
- Ministry of Health (Mexico) NORMA Oficial Mexicana NOM 045 SSA2 2009. For epidemiological surveillance, prevention and control of nosocomial infections. Mexico: Ministry of Health.
- Seisdedos Elcuaz R, Conde García RM, Castellanos Monedero JJ, García Manzanares Vázquez de Agredos A, Valenzuela Gámez JC, et al. (2012) Infections related to the central venous catheter in patients with total parenteral nutrition. Nutr Hosp 27 (3): 775-780.
- Adrianzén D, Arbizu A, Ortiz J, Samalvides F (2013) Mortality due to bacteremia caused by Escherichia coli and Klebsiella spp. producers of extended-spectrum beta-lactamases: retrospective cohort in a hospital in Lima, Peru. Rev perú med. exp health issues 30: 18-25.
- Sánchez González RA, Becerra Victorio G, Grajales Avendaño L, Canseco Ávila LM (2010) Frequency of microorganisms isolated from blood cultures in a tertiary hospital in the state of Chiapas. Enf Inf Microbiol 30(2): 53-55.
- Gonzales L, Toledo S, Parra Y, Santofimio D, Osorio J, et al. (2013) Intrahospital infections in internal medicine and surgery services of the University Hospital of Neiva, 2012. Refs-Revista Facultad De Salud 5(2): 27-33.
- De la Hoz Pastor AE (2013) Characterization of the use of central venous catheter in the Pediatric Intensive Care Unit of Hospital de la Misericordia from January to November 2013. [thesis]. Bogotá DC, Colombia: National University of Colombia,Colombia.
- Almazán Castillo MR, Jiménez Sánchez J (2013) Standardization of intravascular therapy through catheter clinics. Rev Enferm Inst Mex Seguro Soc 21(3): 163-169.
- Mexican Institute of Social Security (2013) Methodological manual for the development of nursing clinical practice guides in the national health system. Mexico: Mexican Social Security Institute, Mexico.
- Sandoval M, Guevara A, Torres K, Viloria V (2013) Epidemiology of nosocomial infections due to the use of central venous catheters. Kasmera 41(1): 7-15.
- Cámara Encarnación RM, Marques P (2013) Permeability of central venous catheter: a systematic literature review. Nursing journal reference 3 (9): 161-169.
- Escobar Carmona I (2014) Adherence to the clinical practice guide of prenatal care with a risk approach in pregnant patients of the FMU no.1 [thesis]. Mexican Social Security Institute. Orizaba Veracruz, Mexico.
- Oñate Ramírez AL, Rendón Macías MA, Iglesias Leboreiro J, Bernárdez Zapata I (2014) Attachment to Guidelines for the management of Bronchiolitis. Bol Med Hosp Infant Mex 71(4): 227-232.
- Perin DC, Lorenzini Erdman A, Callegaro Higashi GD, Marcon Dal Sasso GT(2016) Evidence of care for prevention of bloodstream infection related to central venous catheter: systematic review. Rev. Latino-Am. Enfermagem 24: 1-10.
- Sámano Heras H, Perez Mendez C (2013) Attachment of resident physicians of emergency medicine, to the clinical practice guide “Diagnosis and treatment of spontaneous pneumothorax in the HGZ No. 2 of the IMSS, Hermosillo Sonora”. Mexican Institute of Social Security: National Autonomous University of Mexico, Mexico.
- Adame ML, Reyes RME (2013) Evaluation of the adherence to the recommendations of the clinical practice guide for the diagnosis and treatment of low urinary tract infection during pregnancy by the physician of the first level of care at FMU No. 250. Mexican Institute of Social Security: National Autonomous University from Mexico, Mexico.
- While Leyva Rodríguez MG, Miranda González MA (2010) Attachment of maternal and child nursing staff of IMSS to NOM-007 in prenatal care in San Luis Potosí. Mexican Institute of Social Security: Autonomous University of San Luis Potosí, Mexico.
- Hernández Orozco HG, Castañeda Narváez JL, González-Saldaña N, Ascarrunz L (2010) Hand hygiene before patient care. Acta Pediatr Mex 31(6): 290-292.
- Padgett D, Luque MT, Rivera DM, Zepeda LM, Hernandez AL (2013) Surveillance of nosocomial infections: experience in specialties hospital of the Honduran social security institute 2006-2012. Rev Med Hondur 81(2-4): 68-72.
- Ferrer C, Admiral B (2014) Infections related to the use of vascular catheters. Enferm Infecc Microbiol Clin 32(2): 115-124.
- Resendiz Gutiérrez MG, Muñoz Torres TJ (2012) Level of knowledge and practice acquired during an intravenous therapy workshop course. Electronic Journal of Global Nursing 3(26): 237-245.
-
José María Domínguez Ruíz, Esther Hernandez Martinez. Evaluation of Adherence to the Guidelines of Clinical Practice of Vascular Lines by the Nursing Staff of the UMAE H.E. N.- 14 C.M.N. “A.R.C.” Veracruz Norte. Iris J of Nur & Car. 1(4): 2019. IJNC.MS.ID.000518.
-
Attachment; Clinical Practice Guideline; Vascular line management; Evaluation of adherence
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






