 Short Communication
Short Communication
B.E.L.T.TM: Framework for Nurse Champions to Successful Implement Sustainable Telehealth Services
Antonia Arnaert* and Zoumanan Debe
McGill University, Ingram School of Nursing, Canada
Antonia Arnaert, McGill University, Ingram School of Nursing, Canada.
Received Date: May 05, 2019; Published Date: May 17, 2019
Abstract
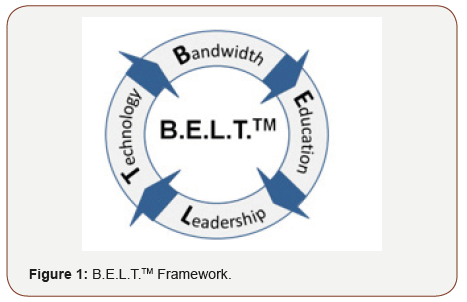
Despite the growing use of telehealth and mobile health, the implementation of these services remains challenging. Nurses, who are often called upon by healthcare organizations to take on the role of champions to initiate and promote the uptake of telehealth services, have expressed a need for a holistic implementation framework. To complement the existing guidelines and recommendations for the provision of telehealth services, the B.E.L.T.™ Framework is an easy tool and catchy mnemonic to guide a systematic environmental assessment of an organization’s readiness, which can foster successful implementation. B.E.L.T.™ stands for “Bandwidth/Broadband, Education/Environment, Leadership & Technology”, as these have been identified by the authors to be the recurrent sources of difficulty in implementation, in both developed and emerging countries. From a metaphorical perspective, B.E.L.T.TM represents a loop. In which these identified elements are interdependent; any breach in this loop will ultimately influence one’s readiness for implementation.
Keywords: Nursing; Clinical champion; B.E.L.T.TM framework; Telehealth; Telemedicine; Mobile health
Introduction
Evidence exists that telehealth or the delivery of healthcare services remotely using a variety of digital technologies has the potential to increase access and quality of care, with the added benefit of cost reduction. Despite its many opportunities, the success rate of telehealth is still disappointing and not integrated optimally in mainstream healthcare services across the globe [1,2]. The development and implementation of a new telehealth service is without doubt complex; it represents the introduction of a multi-faced intervention into an already complex system and often underestimated by healthcare professionals and managers [3]. A conglomeration of factors, ranging from technological to organizational and infrastructure issues, have an impact on the success and sustainability of telehealth services [4]. Despite the efforts from researchers to develop guidelines [5,6], no practical framework have actually been developed for telehealth nurses, as they often take on the role of clinical and managerial change champions in promoting and integrating telehealth [7,8].
The present of a champion is an important driving force behind the implementation of a novel initiative, such as the delivery of telehealth [9]. Nevertheless, telehealth nurse champions need a functional practical framework to assess the readiness of an organization/unit to use telehealth. Based on the challenges and successes of our telehealth projects, we have developed the B.EL.T.™ framework that represents the key contextual elements “Bandwidth/Broadband, Education/Environment, Leadership and Technology” necessary for the provision, implementation and sustainability of telehealth services. From a metaphorical point of view, B.E.L.T.™ represents a loop, in which the above identified elements are interdependent; any breach in this loop will ultimately influence one’s readiness for implementation (Figure 1).
Elements of the B.E.L.T.™ Framework
B.E.L.T.™ - bandwidth / broadband
The letter “B” or the first core element encountered for successful telehealth use and adoption is the need for an Internet connection with the appropriate bandwidth capacity. Network bandwidth refers to the amount of data that passes through the connection over time, whereas broadband refers to as “high-speed” access to the Internet. In other words, broadband works through its bandwidth. If the width of the band is increased, the Internet speed will be faster. In the last decade, the enabling of highspeed data transmission has greatly enhanced the effectiveness and range of telehealth services. Different telehealth services or applications require different bandwidths. For example, the use of video-technology for a real-time videoconferencing telemedicine consultation between a patient and a specialist in a hub location will require higher Internet speed and bandwidth than a home tele-monitoring system for chronic disease management that uses a store-and-forward system to support the transmission and interpretation of patient data at a distance.
The provision of telehealth services also depends on the telecommunication infrastructure available in the geographical region where the hospital is located or where the patient lives. For example, in a home tele-monitoring project on the Island of Montreal in Canada, diabetes patients were obliged to go on their balcony to connect their smartphones to the internet for transmitting data to the telehealth nurse [10,11]. The situation where patients could not download and transmit their data effectively to the nurse had a negative effect on the quality of care provided and the experience of patients. Identical internet connectivity issues were finding in our mobile health project in Burkina Faso, Africa, where we provided antennal care to pregnant women living in rural areas using smart phones [12]. In these projects, the loop was broken because of these Internet challenges. When delivering telehealth, especially home tele-monitoring services, the nurse should assess in collaboration with the technical experts the Internet connection, its capabilities and its use within the establishment, but also connectivity in the remote region where the patient is located.
B.E.L.T.™ - education/environment
The letter “E” represents both the educational component and the adaptation to the sociocultural environment in order to successful implement telehealth. Education, which includes raising awareness of the potential opportunities and benefits of telehealth, is a crucial element for success and should be integrated throughout the development and implementation phases. Although some people within a healthcare organization quickly embrace new technology to enhance and improve all areas of patient care services, the majority of clinicians lack an understanding of hardware and software, as well as the competencies on how to use the technology and deliver the service in their everyday practice [13].
The telehealth nurse champion should oversee that all protocols with training content specific to each organization/unit and adapted to each group of users, for example physicians, nurses, nursing aids, etc., are available as their responsibilities may be different when delivering the service. For example, when providing home telemonitoring, the protocols should cover the operating procedures of the technology; the equipment management and maintenance (i.e., storage, tracking, decontamination and recycling), common technical faults and troubleshooting issues, patient health and safety issues, etc. [14]. In addition to knowing the features of the home tele-monitoring software from the clinician’s point of view, nurses also need to become familiar with the telehealth system from the patient’s point of view. This can be achieved by offering training in a simulated environment, allowing nurses to become familiar with the technology. It is important to provide regular refresher around specific protocols to enhance knowledge but also to adapt to the rapid evolution of digital technology.
Patient educational needs are often underestimated when setting-up telehealth services as we take for granted that patients have already embraced the information age and that they will learn to use the new technology in a timely manner, which often leads to a depreciation of the impact of telehealth on personal health. As with professionals, patients must receive in-depth training in upstream with live telehealth applications. Adaptation to the socio-cultural environment is another important aspect to consider as traditional and religious beliefs, local taboos and language barriers can make acceptability difficult and therefore underestimate the success of any telehealth initiative.
B.E.L.T.™ - leadership
Leadership, which is the third core element “L” of B.E.L.T.TM, stresses the importance of having a champion within an organization/unit that shows an interest in telehealth, takes the lead in using these services and starts promoting the idea to colleagues [15]. Generally, nurses will assume the role of champions, as they are already care managers who journey with patients in the healthcare maze [16]. They coordinate all clinical interventions for the patient with the clinical team and utilize all available resources to meet an individual’s health needs. Champions must have experience with the clinical and medical issues addressed by the new service, the ability to motivate the telehealth team to overcome the difficulties of the change process, and the ability to build bridges between different values, beliefs and assumptions of all stakeholders, i.e. clinicians, managers, support staff and technology experts. During the implementation of a telehealth program, the role of the champion will change from a team leader, to a patient advocate and coach and eventually a marketer and salesperson.
B.E.L.T.™ - technology
The letter “T” stands for the technology; which is an element that most people envision when they hear the term telehealth. Notwithstanding, technology encompasses a broad concept that is not limited only to information technology and communications and related infrastructure such as hardware, software, peripherals (i.e., electronic stethoscope, general exam camera, etc.), cloud storage, etc. but it also refers to the general infrastructure such as access to electricity and transportation. When developing a telehealth program, the nurse champion within the organization must be involved in all steps to evaluate the choice of technology needed to provide telehealth services; that should be done in terms of features and specifications required to provide the services, and not in terms of suppliers or equipment models.
In addition, the various fixed or mobile devices use to provide remote care must be user friendly for patients and integrate into their lifestyle. From a practical standpoint, organizations must also consider interoperability between two or more hardware and software systems for successful integration into their current services. It is important that the equipment available in point A is fully compatible with what will be used in point B. The general infrastructure, which is often defective or absent, can be a significant barrier when implementing telehealth in rural areas and/or low and middle-income countries. For example, a lack of electricity power creates challenges for nurses and patients to charge their smart phones or computers. As such, any project must evaluate a substitute to circumvent these different technical interruptions.
Conclusion
To complement the existing guidelines and recommendations for the provision of telehealth and mobile health services, the B.E.L.T.™ Framework is an easy-to-use tool and an eye-catching mnemonic that guides systematic preparation and evaluation of an organization to support successful implementation. We do not intend to suggest that this framework and its components are comprehensive and that other factors do not contribute to the availability of an organization to adopt and implement telehealth services. On the contrary, we consider B.E.L.T.™ as a checklist for nurse telehealth champions within a health care organization seeking to implement telehealth services. More research on the items in this list should continue for the effective functioning of remote health services, as it is a complex enterprise.
Conflict of Interest
No Conflict of interest.
Acknowledgement
None.
References
- van Dyk L (2014) A review of telehealth service implementation frameworks. International Journal of Environmental Research and Public Health 11(2): 1279-1298.
- Scott RE, Mars M (2015) Telehealth in the developing world: Current status and future prospects. Smart Homecare Technology and Telehealth 3: 25-37.
- Boddy D, King G, Clark J, Heaney D, Mair F (2009) The influence of context and process when implementing eHealth. BMC Medical Informatics and Decision Making 9: 9.
- Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, et al. (2016) Evaluating barriers to telemedicine worldwide: A systematic review. Journal of Telemedicine and Telecare 24(1): 4-12.
- .Doarn CR, Merrell RC (2014) Standards and guidelines for telemedicinean evolution. Telemedicine and e-Health 20(3): 187-189.
- Krupinski EA, Antoniotti N, Bernard J (2013) Utilization of the American Telemedicine Association’s clinical practice guidelines. Telemedicine and e-Health 19(11): 846-851.
- Wade V, Eliott J (2012) The role of the champion in telehealth service development: A qualitative analysis. Journal of Telemedicine and Telecare 18(8): 490-492.
- Fathi JT, Modin HE, Scott JD (2017) Nurses advancing telehealth services in the era of healthcare reform. The Online Journal of Issues in Nursing 22(2).
- Shaw EK, Howard J, West DR, Crabtree BF, Nease DE, et al. (2012) The role of the champion in primary care change efforts. Journal of American Family Medicine 25(5): 676-685.
- Arnaert A, Wainwright M (2008) Developing a home telecare services for elderly patients with COPD: Steps and challenges. Canadian Journal of Nursing Informatics 3(2): 49-83.
- Arnaert A, Gabos TG, Thomas E (2011) Telemonitoring of blood sugar levels for diabetes self-management in multi-ethnic Quebec: Evaluation Report. Public Health Agency of Canada, Canada.
- Arnaert A, Ponzoni N, Sanou H, Noufou GN (2019) Using the B.E.L.T. Framework to implement an mhealth pilot project for preventative screening and monitoring of pregnant women in rural Burkina Faso, Africa. Telehealth and Medicine Today (in Press).
- Ayatollahi H, Sarabi FZP, Langarizadeh M (2015) Clinicians’ knowledge and perception of telemedicine technology. Perspectives in Health Information Management 12(Fall): 1c.
- Starren J, Tsai C, Bakken S, Aidala A, Morin PC, et al. (2005) The role of nurses in installing telehealth technology in the home. Computers Informatics Nursing 23(4): 181-189.
- Lindsey J, Ono C, Debe Z, Ledua A, Mallari RQ (2007) The Necessity of the Clinical Champion, 7th International Conference on Successes and Failures in Telehealth. Journal of Telemedicine and Telecare 13(3): 101- 110.
- White C (2011) Nurse champions: A key role in bridging the gap between research and practice. Journal of Emergency Nursing 37(4): 386-387.
-
Antonia Arnaert, Zoumanan Debe. B.E.L.T.TM: Framework for Nurse Champions to Successful Implement Sustainable Telehealth Services Iris J of Nur & Car. 1(5): 2019. IJNC.MS.ID.000521.
-
Nursing, Clinical Champion, Telehealth Framework, Telehealth, Telemedicine, Mobile Health, Readiness for Implementation, Healthcare Services, Integrating Telehealth, Diabetes Patients, Telehealth Nurse, Implementation Phases, Framework, Organization to Support, Medical Issues, Clinical Issues, Digital Technology, Physicians, Nursing Aids
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






