Research Article
Research Article
The Resident’s Welcome Day: An Opportunity to Faster the Well-Done Job
Pensieri C1*, Saccoccia S2, De Micco F3, De Benedictis A4, Giacomobono F5 and Alloni R6
1Department of Human Sciences, LUMSA, Rome, Italy
2Clinical Leadership team FPUBM, Rome, Italy
3Clinical Risk Manager, FPUCBM, Rome, Italy
4Quality Manager, FPUCBM, Rome, Italy
5Università Campus Bio-Medico di Roma, Rome, Italy
6Clinical Director FPUCBM and UCBM Specialization School Coordination, Rome, Italy
Pensieri C, Department of Human Sciences, LUMSA, Rome, Italy
Received Date: August 30, 2024; Published Date: September 13, 2024
Abstract
The Fondazione Policlinico Universitario Campus Bio-Medico’s educational project in collaboration with the Università Campus Bio-Medico is an orientation path intended for 1st year residents. The project, started in 2015 with the mere distribution of printed information materials, has developed into the current version. Data show that students declare themselves to be lacking in some areas of the technical clinical skills needed for successful integration into the “practical-clinical” world. Regarding haemogasanalysis: 28% received accurate instruction on how to perform it. 21% performed only the arterial sampling (no blood extraction). Only 31% were aware of what pre-discharge therapeutic reconciliation was and what had to be done, after the training, 100% were able to answer correctly. From the satisfaction survey (and confirmed by the 10-month assessment questionnaire) we found that playful-interactive training (based on gamification) is the most appreciated. This confirms that teaching with the new generations should be very interactive and engaging.
Keywords: Education, Innovative teaching, Experiential training, Residents, Medical education
Background
Postgraduate medical training in Italy consists of a 4 or 5-year residency (according to the chosen specialty) following on from a national exam. Admission to the residency program is contingent on test results and overall academic scores, and there is a capped annual number of residency positions. During training, residents usually work in academic hospitals, gaining clinical experience in their relevant specialty and rotating throughout the main subspecialties. In addition, they follow an educational program mainly based on frontal lessons (i.e. teaching activities which take place from the front of the classroom), and they may be involved in research projects. The level of autonomy with which trainees can perform the required tasks is regulated by law and depends on the postgraduate year [1].
The Italian legislative decree n° 368 [2], transposing the European Union Directive 93/16/CEE that regulates also the medical residency, declared the transition of the resident from the status of student to that of worker-in-training, through the stipulation with the university and the Italian’s region of an employment contract of a subordinate nature lasting one year and renewable from year to year for the entire duration of the residency course (with the economic implications and tutelage of the case). Law 266/2005 (Financial Act 2006) allocated funds for the application of the contract starting from the academic year 2006 - 2007, introducing modifications to the original text.
Instead, the original version of the legislative decree (Legislative decree 368 / 99, art.37) envisaged a training-work contract, the current legislation, following the changes made by the law 266 / 2005 (art. 1, c. 300), speaks of a “specialized training contract”, and does not allow it to be traced back to any of the existing contract types.
This means that for all intents and purposes residents cannot be considered as workers of the hospital instead, it is determined that their contract (Legislative decree 368/99, art. 37) “is stipulated with the university, where the residency school is located, and with the region in whose territory the health companies are located, whose structures are the predominant part of the training network of the residency schools program”.
So, the contract of the new resident is not stipulated directly with the health companies in which they operate but with the reference university.
Moreover, since the competition is national (according to Italian law n. 244/2007: “the candidate who passes the competition is admitted to the chosen “School of Specialization” based on the score obtained and the final ranking”), it very often happens that the new resident finds himself / herself being placed in a different hospital from the one where he / she did his undergraduate training or where he / she studied medicine and therefore has to deal with a totally new environment [3].
This very often implies that the first-year resident:
1. Does not know where some important services of the hospital (hospital direction, admissions office, pharmacy, administrative offices) are located and the key people (heads of operational units, nursing coordinators, who manages the beds or other resources, etc.).
2. Does not know the physical structure of the hospital where he / she will take up his duties (where are the wards, where are the clinical services such as endoscopy, radiology etc.).
3. Does not know the hospital healthcare management system (information technology).
4. Does not know the rules of the institution (dress code, code of ethics, nursing organization, etc.).
5. Does not know the hospital’s existing “policies and procedures” (policies, guidelines, procedures, operating instructions, etc.) [3].
Setting
The Università Campus Bio-Medico di Roma (UCBM) had, in 2022, 26 residency schools with about 145 new residents who took up their duties at the Fondazione Policlinico Universitario Campus Bio-Medico (FPUCBM).
In 2017 the PUCBM started these initial orientation training for new residents. The Fondazione Policlinico Universitario Campus Bio-Medico is a teaching hospital with around 300 beds and roughly 30 clinical operational units, including an emergency department and a hospice. The Campus Bio-Medico University of Rome pursues the objective that its students, and so also the residents, “achieve high scientific, technical and professional competence, as well as high moral sense” [4]. In a context in which technical preparation and learning ability have a significant impact, the skills required have changed considerably and clinical work has changed profoundly [5].
According to the report ‘To err is human: building a safer health system’ [6] American health professionals are responsible for more than 98,000 deaths a year. If this were really the case, we should ask how health professionals could improve the quality of their education right from university and post university training. Med students’ desire more participatory lessons. In undergraduate medical and health faculties, lectures are a notable but not exclusive part of the forms of learning [7].
“The role of teachers is rightly believed to be universally crucial to the quality of education. Teachers, in addition to decisively affecting the educational outcomes of students, activate and support the improvement processes of the institutions they work in” [8].
Teaching at the university level requires skills that include (in addition to knowledge of the discipline) mastery of teaching strategies [9]. In addition, the use of effective teaching methodologies, capable of getting each student to acquire knowledge and skills more quickly, consistent with the identified objectives, effectively saves time-work time that can be invested in other areas of greater interest to the student [10].
The Fondazione Policlinico Universitario Campus Bio-Medico nursing care, unlike in many Italian hospitals, is organized according to the model for small teams and by complexity of care, a model integrated with the criterion of bed distribution by “intensity of care”. This means that patients are grouped by type of care required and not by operative unit [11].
The result is a very flexible organizational structure, which has given up the classic division into specialist departments to associate maximum efficiency with an optimal level of assistance. The Fondazione Policlinico Universitario Campus Bio-Medico is, from 2014, a Joint Commission International (JCI) accredited hospital (as “academic medical center”, a hospital in which both teaching and clinical research take place).
The Joint Commission International accreditation testifies the governance’s focus on quality and safety of the care provided. Is clear that, in this environment, the sudden entry into clinical work of a group of professionals in training is a critical moment. Of the residents taking up residency in November 2022, only 19% had studied at our university, a sharp decrease from 27% in 2019 and 22% in 2018.
The resident starts their service at the hospital on the date established by the decree published in the Italian’s official gazette, even if sometimes they are allowed to attend as an observer for a few days or weeks (as they are not covered by a contract or insurance); their first day of work often coincides with their first contact with the new environment. Unfortunately, there is no provision in the contract, nor in the law, for a program to introduce the clinical activities of residents. So, the common practice consists in the shadowing of a senior resident for the first weeks, to understand how to navigate and acquire basic knowledge (often in this phase, the resident is more a “burden” than some help) [3].
Generally, this phase lasts for two or three weeks but in some cases, it can last up to 6 months. After this shadowing period, the resident starts to work in autonomy, within the limits allowed by the chief of the residency program. From our non-detailed Google search, we noted that few Italian medical universities (in 2022) provide initial orientation for new doctors in training (we could only find online news on initial training from 7 other universities out of a total of 40 medical faculties in Italian + 18 medical faculties in English) (Annex 1).
Unfortunately, it’s not easy to find this kind of information because these orientation courses do not have a great impact in the press (therefore they are not easily identifiable via online search engines) nor an impact on scientific publications.
We have found that some specific acclimating program was held, for example in the department of radiology of the NYU Langone Health [12]. Acclimating residents to radiology residency requires attention to new responsibilities, educational material, and social cohesion. To this end, they instituted a structured orientation week for incoming residents and assessed its impact. First year residents attended a five-day orientation free of clinical duties, consisting of didactics, hands-on training sessions, and social events.
However, it is interesting that some Italian universities are starting to develop these introductory activities. Education in the past decades was based on mnemonic learning and it was one of the main elements (factor) of educationism, characterized by frontal lectures, memorization, and repetition. With the rise of constructivist perspectives and the increasing availability of “digital memories”, there has been a slow liquidation of memory and its function in relation to learning [13].
Undeniably related, learning and memory, however, are slightly different entities. “Learning is the acquisition or modification of a subject’s knowledge, behaviors, skills, values or preferences and may involve the synthesis of different types of information. Memory is a process by which information is encoded, stored, and then retrieved. Therefore, it is possible to remember something without actually having learned it from memory. Learning occurs through the stages of the memory process” [14].
In medicine, many years ago, learning procedures was based only on practice on the patient; they were the “first guinea pigs” of the students; today, however, this form of learning is limited for several reasons. Some procedures are performed quite infrequently, so it takes a very long time before the learner acquires the necessary autonomy and skill, which must then be maintained over time [15].
In simulation it is used to say this motto: “never the first time on the patient”. While it is true that the simulation mannequin imperfectly simulates the human person, the exercise in simulation allows the learner to gain knowledge of the tools to be used and the sequence of actions to be followed, giving the learner a familiarity with the “constant” and repeatable part of the procedure: it is really a way to overcome the “see one, do one, teach one” model [16], now inadequate to the number and complexity of procedures that each learner must learn to handle during the training period.
So, we needed something similar to help residents with training in bureaucratic, clinical, administrative and IT (information technology) procedures that would enable them to get into hospital work as quickly as possible.
By looking at the educational path of the residents through the magnifying glass of the cognitivism (which is fundamentally concerned with “how” we process information obtained to transform it into knowledge) [17], we have realized that the most effective learning method for new residents is problem solving, an activity that not only facilitates long-term memorization but also promotes the integration of new content into the learner’s complex knowledge network.
In fact, reaching and possessing information can build true learning only if it’s followed by a change in behavior. Following the approach of Piaget (i.e. the centrality of “discovery”) and Dewey (“learning by doing”) we decided to set up the orientation training days in a playful and interactive way. Indeed, “experiential learning theory” suggests that concrete experience, reflective observation, and active participation are essential elements for the student to assimilate new knowledge and new skills in order to act appropriately and confidently in real clinical situations [18].
We believe that the use of innovative and highly interactive teaching methodologies can foster usability and learning. According to De Paz [19], if a discipline is reduced to pure information, it loses the formative sense; it can instead have through a critical approach that requires reasoning and the learner’s personal contribution, that is, acts of construction and discovery. Starting from this concept of “practical action”, of “discovery” and “learning in the field”, the Fondazione Policlinico Universitario Campus Bio-Medico has strongly supported the practical and collaborative learning experience that helps to “fully learn new skills and knowledge” [20].
In fact, we went through the “restless trinomial” [21]: teach/ educate/train.
• Teaching: the transmission of knowledge and techniques.
Educating: “drawing out” (ex-ducere) but with the same root as “edere” which thus refers to “nourish” and “make grow” [22].
• Training: “the way in which human existence, considered in its totality, takes on the form that is proper to it, through [...] psychic and physical data, natural and historical-cultural data, individual and collective data, actions and events, freedom and necessity and, of course, the experiences that go hand in hand with these data and that determine the unique and unrepeatable character of each person” [23].
Training is an ancient and topical category. It is the prerequisite for educational action, as it constitutes the backbone of that process of human growth that encompasses and harmoniously unifies the different dimensions of existence [22].
Many factors determine a resident’s good training, such as a sailboat that needs the water to glide on, but also the wind, the rudder, the compass, the sail, but above all the navigator (the skipper) and the ability to deal with the unexpected.
Thus, training must have a direction to follow and tools to direct itself, techniques to steer, values that know how to inflate the sails and drive towards existential design goals [22]. It cannot therefore be focused on a single aspect, nor refer to a single moment of existence, nor concern a single sphere. It is not enough for us to build the resident’s boat, we want to equip him or her with all the features to safely face the stormy sea, starting with the initial orientation.
Methods
We administered 3 questionnaires to our new 147 residents.
1. An entry questionnaire to assess previous training and knowledge (145 questionnaires out of 147 enrolled). Then we collected data to assess possible future training needs, on 3 particular areas: technical skills, quality and safety procedures, and working environment knowledge.
2. A questionnaire at the end of the training to assess the change in this knowledge (65 participants).
3. A follow-up assessment questionnaire after 10 months to find out whether, in the field, this training was really useful (54 participants).
The educational program
We conducted the training on the first useful day after the start of the contract, on 2, 3 and 4 November 2022, we scheduled 18 hours of training as follows:
1) Lectures: 11 hours.
2) Practical activities 7 hours: role-play and innovative teaching activities (egg-challenge, covid dressing/undressing, etc.).
Even the choice of “places” where training has to take place was not random but determined by teaching requirements. In particular, we used the university’s Aula Magna, a lawn in front of the university, normal teaching rooms and our Simulation Center, in order to engage audiences and inject a bit of fun into mundane activities as well as to generate motivational and cognitive benefits.
In terms of the development of more engaging learning environments for students, Ulmanen [24] suggests that more attention should be paid to create positive opportunities to participate, in terms of both academic activities and peer interaction. Starting from this suggestion we thought to “balance” frontal lessons and practical activities.
Program:
DAY 1
1) Registration of participants and handing out of lab coat watches. PUCBM provides each resident with a lab coat watch (Figure 1) branded Università Campus Bio-Medico to motivate doctors not to use their wristwatches and collaborate to prevent the spread of infections.
2) Institutional greetings given by resident representative (in order to help new residents to see the “face” of those who represent them at the internal institutional level); Campus Bio- Medico University of Rome President; UCBM Dean; UCBM CEOGeneral- Director; Chief of the Faculty of Medicine, Directors of Residents Schools.
3) Campus Bio-Medico University of Rome: “Values and code of ethics” (The founding principles: what are our human values that underlie our clinical performance).
4) The resident’s employment contract (legal information).
5) Presentation of the Fondazione Policlinico Universitario Campus Bio-Medico by the CEO-General-Director of the PUCBM.
6) Training on covid dressing/undressing with water pistols filled with fake blood to test the ability to undress without contamination – held on the lawn in front of the university (this activity was designed because covid was still in place and because the use of particular personal protective equipment on some special occasions was still mandatory).
7) A role-play on a liver biopsy procedure with the aim of introducing doctors to quality and safety procedures (patient identification, hand hygiene, patient education: information notes and collection of informed consent, etc.). This activity was organized in more than one classroom using material from our simulation center, from the hospital beds to paper/informatics documentation, from sterile gloves to clinical instrumentation. The residents who participated to this sessions had to study a script and impersonate 2 structured physicians, a patient and his wife (with the mandate to be a “communicatively demanding” wife) and one of our “structured” nurses who had to make “pre-determined” mistakes such as incorrect patient identification (anytime information about a patient is recorded or accessed — from signin sheets to online scheduling systems to electronic health records. Because this process is universal, it is fraught with risk for wrongpatient errors), incorrect transport of biological specimens etc. Other students had the task of recording the errors they noticed during this session on a special observation sheet and then we made a single plenary session to debrief all together.
DAY 2
1) Quality and safety and introduction to Joint Commission International standards. How residents can report adverse events via hospital LAN (Local Area Network).
2) Hygiene and hospital infections (care-related infection control committee); bundle, hand hygiene and correct dress code.
3) GDPR and the management of sensitive patient data (privacy, data breach, not allowed using of WhatsApp, Microsoft Teams, etc.).
4) Personal protective equipment and their use: masks, eye protection including face shields and goggles, etc.
5) The Hospital Information System (SHI): computerized medical records, inpatient, outpatient, operating log, Prescription and Medication Administration Record (PMAR) document where medications are prescribed and administered in order to have an accurate medication management.
6) Nursing care organization in hospital wards (according to the model by small teams and by complexity of care).
7) Patient flow: the movement of the patient within the health care facility from admission to discharge.
8) Problem solving session and experiential team building: small group challenges, in which all interdisciplinary teams have to solve 9 problems in 30 minutes.
9) Small group discussion session of a clinical bioethics case: in particular, it was a clinical bioethical case of reconstructive surgery following neoplastic disease.
DAY 3
1) Resident school service: services provided and administrative arrangements (timecard stamping, tutoring, educational network, etc.).
2) Clinical risk and the importance of quality & risk management; a clinical case about risk management in which happened a dosing error of a chemotherapeutic drug.
3) Spiritual care of patients; chaplaincy and other religious ministers.
4) Correct dress code in the hospital, management of gowns and overalls (non-use of nail polish, wrist watches, bracelets, etc.).
5) “Campus Sharing” (student association for recreational activities).
6) “Campus Life”: recreational and educational activities organized by Campus Bio-Medico University of Rome.
7) “ASD Campus”: sport activities and events for University Campus Bio-Medico people (students, university’s staff, family, residents, etc.).
8) Final team building activity: the “egg challenge”: interdisciplinary teams had 3 days in order to design and build a lander that protects a raw egg that’s dropped from up high (the third floor of our university).
Results
The analysis of the data from the first questionnaire submitted to 1st year residents revealed that the previous university training seems did not adequately prepare doctors for the practical approach with patients. In fact, only a small part of the basic technical skills was acquired by doctors during their university training. For example, almost half of the residents (48%) had never performed a haemogasanalysis (neither complete nor partial), 32% had never taken a blood sample from a patient while, on the positive side, 98% had taken a pulse and blood pressure and 89% collected and wrote at least one medical history (Table 1).
Table 1: Results of educational needs.
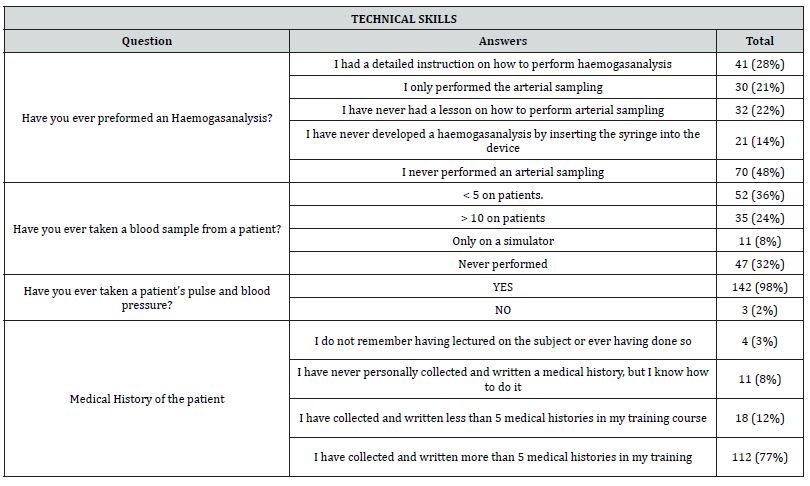
A comparison of the data collected from the pre, and post training questionnaires showed that, with regard to the quality & safety procedures (LASA: look-alike; sound-alike medication; therapeutic reconciliation at patient’s discharge; adverse event reporting and dress-code) the course provided an improvement, although the starting point was already very good (Figure 2).
Among the improvements achieved after the orientation day, we also found the improved ability to report an adverse event in which the resident has participated or has simply seen happen. During the training session, the correct way to report the adverse event through the Confidential Reporting System via the Hospital Information System (HIS) was indicated.
Regarding the hospital dress code, a + 5% related to some generic rules were specified during the class, for example:
• White coats should be buttoned completely to protect skin and clothing from splatter and spills.
• Wristwatch must not be worn when providing clinical care.
• Short and natural nails (fake or long nails or polished nails are not allowed).
• Long hair should be tied back.
• No rings when providing clinical care.
• No bracelets when providing clinical care.
• The use of a tie is allowed.
Knowledge of the working environment
The third section was devoted to specific knowledge of the hospital environment (Figure 3). This knowledge is necessary to orient oneself within the Fondazione Policlinico Universitario Campus Bio-Medico (e.g. where are physically located: the analysis laboratory, radiology, blood collection center, transfusion center, pathology department, etc.). Interestingly, the curve shifted from left to right (while maintaining a single 10 - which is the same student who answered 10 on the first submission).
It means that residents declared that they have increased their spatial awareness of internal services and units (black column in Figure 3).
Quality Assessment
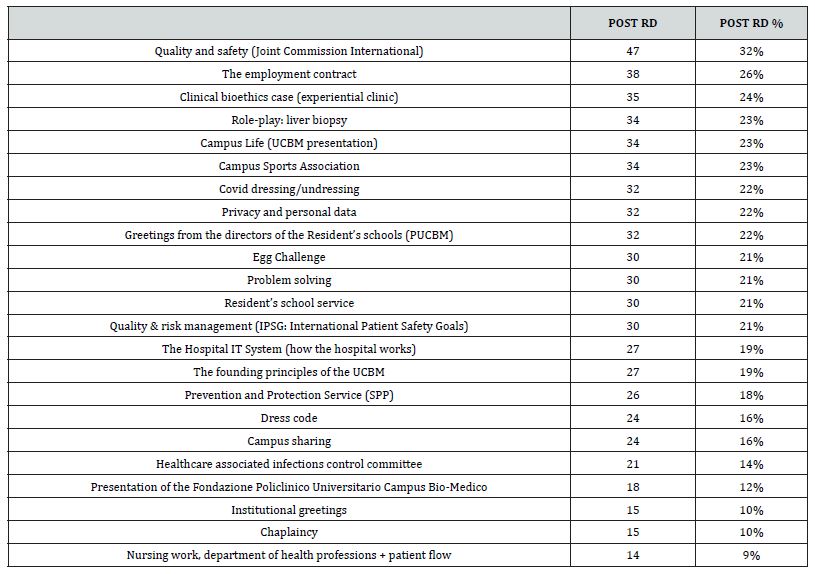
With regard to the “hot” assessment of the Resident Day, an online-based questionnaire was designed using the collaborative web survey software Google Forms to investigate the perceived usefulness of the various sessions.
Using Likert scales (1-5 from: “not at all useful” to “very useful”), we asked for feedback on the theoretical sessions (Table 2) and the practical sessions (Table 3). A few days after the Resident Day we asked to rate the perceived usefulness of the various activities carried out and then, 10 months later, we asked for feedback again, to assess how helpful the activities had been in “real” life at the hospital this study used a questionnaire-based approach to obtain information from medical residents enrolled in the Residency Programs of Campus Bio-Medico University of Rome.
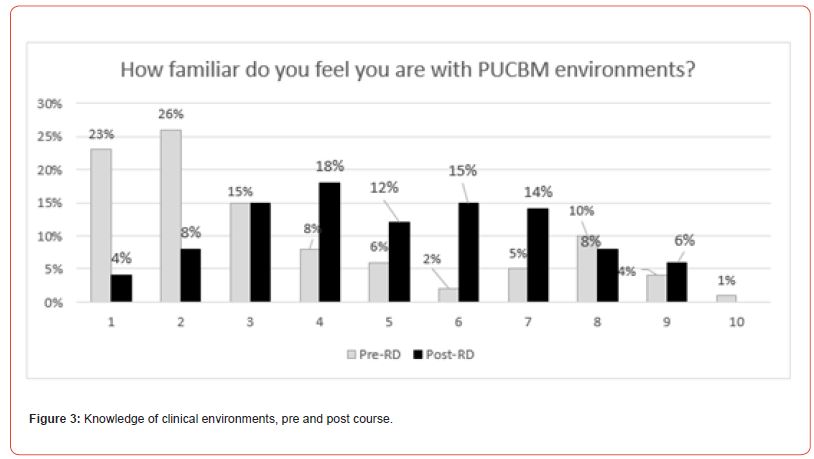
Table 2: Perceived usefulness of theory sessions.
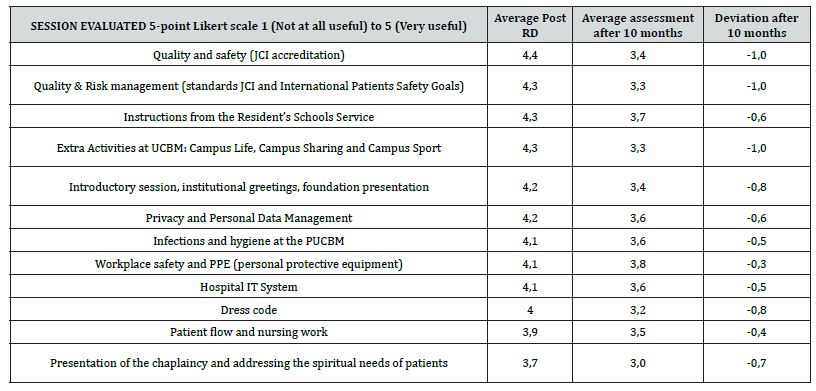
Table 3: Perceived usefulness of theory sessions.
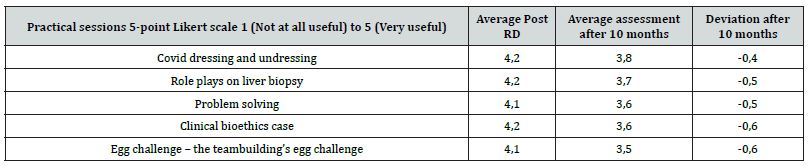
So, the importance of practical activities emerges from these data (Table 2 and Table 3). Practical activities had a lower 10 months changing score (from -0.4 to -0.6 points), while the traditional frontal training activities ranged between -0.3 and -1.0 points. It means that residents thought that, in the clinical field, the traditional frontal training was less useful than practical activities. This confirms the hypothesis of this article in which experiential learning and engagements activities are perceived as “useful” even after job placement. Finally, we assessed the expectations of the residents.
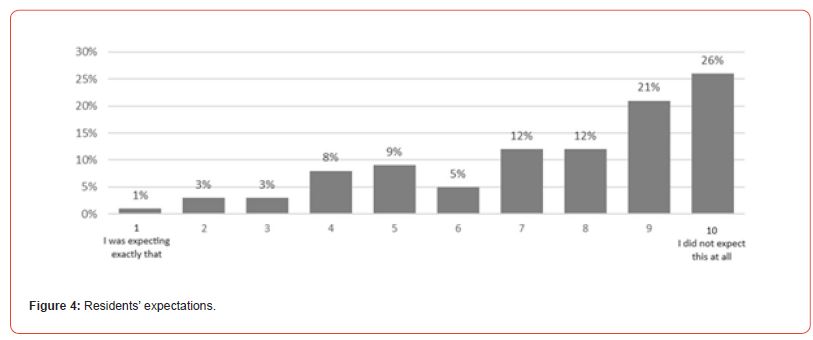
We asked whether, when they chose Campus Bio-Medico University of Rome as their university for the Residency program, they expected such an initial orientation. The answers, which are very interesting, are shown in Figure 4.
Interestingly, the lowest marks (1, 2, 3 and 4) were given by trainees who had graduated from our university and therefore (most likely) had already heard about the event or had seen some parts of the previous year’s event.
More than half of the new residents (59%) did not expect (from 8 to 10 pt. in Table 4) a week of orientation training like the one we offered. Finally, we asked which activities left something useful behind.
Table 4: perception of usefulness.
Discussion
Data collected highlights some very interesting aspects of the medical student’s training pathway. The technical skills necessary for successful integration into the ‘practical-clinical’ world are lacking in some areas. For example, regarding haemogasanalysis, only 28% claimed to have received accurate instruction on how to perform the test and 21% had only performed the arterial sampling.
32% stated that they never performed a blood test on a patient (while only 8% had performed it on a simulator). Another important aspect of ward life concerns pre-discharge therapeutic reconciliation, before our training only 31% were aware of what it was and what had to be done, after the training 100% were able to answer correctly.
We have decided we must improve our knowledge of the environment in the future: the improvement curve is in fact not very appreciable. However, we must consider that in 2022 the Covid restrictions had not yet ended, and it was not possible to organize playful training activities to introduce new residents to the various environments, even though we consider it essential for new residents to be well oriented ‘spatially’ in the wards/services of the hospital.
Lastly, a fundamentally important fact is the evidence that ludic-interactive training (also based on gamification) proved to be among the most appreciated by the students (grey lines in Table 4), confirming that teaching with the new generations of students should be increasingly interactive and engaging [25].
Limits
Our training project and data collection have limitations that must be considered. First, the non-exportability of the training project for large universities with 500-700 first year residents (it’s quite difficult to organize similar activities, practical ones would need 20 or more lecturers and tutors). As each university has its own peculiarities (the approach to the patient, the bioethical approach, the hospital layout), it is therefore not possible to think of a ‘standard’ event applicable to all universities.
Conclusions
The training project of the Fondazione Policlinico Universitario Campus Bio-Medico in collaboration with the Università Campus Bio-Medico di Roma is an orientation pathway that started in 2015 with the simple distribution of printed information material to new residents (procedures vademecum) and then in 2016 with one training day (without practical activities) that has developed over time to the current version described in this article and it is constantly evolving.
The assessment questionnaire 10 months after the educational edition allowed us to understand how useful some sessions proved to be “on the job” and how many lessons proved to be less useful. Very interestingly, after 10 months, the practical activities scored lower with a range between -0.4 and -0.6 pts (out of 5 pts) while the classic frontal educational activities between -0.3 and -1.0 pts. This confirms the hypothesis of this article in which, experiential learning activities that create engagement in learners are perceived as “useful” even after job placement.
Acknowledgment
None.
Financial Conflicts of Interests
There are no relevant financial or non-financial competing interests to report.
References
- Abati E, Nelva Stellio L, Manini A, Moroni F, Azzalini L, et al. (2022) A cross-sectional survey study of the impact of COVID-19 pandemic on the training and quality of life of Italian medical residents in the Lombardy region. Annals of Medicine 54(1): 2325–2338.
- Italian Legislative Decree of 17/8/1999, n°
- Pensieri C, De Benedictis A, Iori T, Nobile L, Alloni R (2021) L’orientamento iniziale dello specializzando. Nuova Secondaria - n. 5, gennaio 2021 - Anno XXXVIII: 43-57.
- (2020) UCBM (Università Campus Bio-Medico di Roma), Aims Charter ed p. 1.
- Guaglianone L, Malzani F (2007) Come cambia l’ambiente di lavoro: Regole, rischi, tecnologie. Giuffré editore, Milano.
- IOM (Institute of Medicine) Kohn LT, Corrigan JM & Donaldson MS, Editors (2000) To Err Is Human. Building a Safer Health System. Committee on Quality of Health Care in America, National Academy Press Washington DC.
- Pensieri C, Alloni R (2019) Educazione e simulazione nelle Facoltà universitarie. Una review. Ricerche di pedagogia e didattica 14: 121-142.
- Tammaro R, Petolicchio A, D Alessio A (2017) Formazione dei docenti e sistemi di reclutamento: un leitmotiv, Italian Journal of Educational Research (19): 53-67.
- Biasutti M, Makrakis V, Concina E, Frate S (2017) Sviluppo professionale dei docenti universitari: un’esperienza in un progetto internazionale. Italian Journal of Educational Research 18: 67-82
- Binetti P (2000) Diventare medici in Europa, Società Editrice Universo, Roma 133.
- Pensieri C, Saccoccia S, De Benedictis A, Alloni R (2022) Il Resident-Day 2019: l’esperienza del Policlinico Universitario Campus Bio-Medico per l’orientamento dei nuovi medici specializzandi. Nuova Secondaria Ricerca 7: 34-53.
- Prabhu V, Rispoli JM, Chhor CM, Mercado CL, Fefferman NR (2020) Assessing the impact of an orientation week on acclimation to radiology residency. Clin Imaging 65: 108-112.
- Rivoltella PC (2014) La previsione. Neuroscienze, apprendimento, Didattica. La Scuola, Roma.
- DeMaria S Jr, Levine AI (2013) The Use of Stress to Enrich the Simulated Environment; in A.I. Levine et al. (eds.), The Comprehensive Textbook of Healthcare Simulation, Springer Science + Business Media New York, USA pp. 66
- Innocenti F, Pini R (2015) La simulazione in medicina d’emergenza-urgenza, MEDIC 23(2): 56-63
- Vozenilek J, Huff JS, Reznek M, et al. (2004) See one, do one, teach one: advanced technology in medical education. Acad Emerg Med 11: 1149-1154.
- Cinque M (2011) E-teaching. Scenari didattici e competenze dei docenti nell’evoluzione del web. Palumbo ed. Palermo-Firenze.
- Zannini L (2005) La tutorship nella formazione degli adulti. Milano: Guerini Scientifica.
- De Paz M (2018) Il costruttivismo: una rivoluzione della didattica spesso dimenticata, Arte e Scienza 5(10): 49-64.
- Haynes JD, Sakai K, Rees G, Gilbert S, Frith C, Passingham RE (2007) Reading hidden intensions in the human brain. Curr Biol 17(4): 323-328.
- Cambi F (2000) Manuale di filosofia dell’educazione, Roma-Bari, Laterza.
- Iori V (2018) Educatori e Pedagogisti, Edizioni centro studi Erickson, Trento.
- Fadda R (2005) Scelta e caso nei processi formativi. In LD Alessandro e V Sarracino, Saggi di pedagogia contemporanea, Pisa, ETS.
- Ulmanen S, Soini T, Pyhältö K, Pietarinen J (2014) Strategies for academic engagement perceived by Finnish sixth and eighth graders. Cambridge Journal of Education 44(3): 425–443.
- Pensieri C, De Benedictis A, De Micco F, Saccoccia S, Ivziku D, et al. (2023) Continuing Education through the Campus Game: A Sustainable Gamification Project to Improve Doctors’ and Nurses’ Knowledge of Quality and Clinical Risk Management. Healthcare 11: 2236.
- National Academies of Sciences, Engineering, and Medicine (2000) To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press.
- Italian Law n. 244/2007 paragraph 433, Article 2, and Regulation No. 130/2017. Decree of the Ministry of University and Research, 2023.
- Joint Commission International (2021) Accreditation Standards for Hospitals, 7th ed.; Joint Commission International: Oakbrook Terrace, IL, USA.
-
Pensieri C, Saccoccia S, De Micco F, De Benedictis A, Giacomobono F. The Resident’s Welcome Day: An Opportunity to Faster the Well-Done Job. Iris J of Edu & Res. 4(1): 2024. IJER.MS.ID.000578.
-
Education, Innovative teaching, Experiential training, Residents, Medical education
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.