 Mini Review
Mini Review
Primary Headache in Childhood Associated with Psychiatric Disturbance: A Mini Review
Cacciaguerra G, Oliva C, Pappalardo MG, Messina G, Sapuppo A , Marino L, Sciuto S, Fontana A and Pavone P*
Department of Clinical and Experimental Medicine, University of Catania, Italy
Piero Pavone, Department of Clinical and Experimental Medicine, University of Catania, Via S. Sofia 78. 95123 Catania, Italy.
Received Date: June 05, 2020; Published Date: June 18, 2020
Abstract
Pediatric headache is a big chapter of all-time medicine. The many medical visits required for this problem suggest us to think on how much we still have to discover about this pathology.
Headache is the third cause of visits to pediatric emergency departments (ED). According to a systematic review, headaches in children evaluated in the ED are primarily due to benign conditions that tend to be self-limiting or resolve with appropriate pharmacological treatment. The more frequent causes of non-traumatic headache include primitive headaches (21.8-66.3%) and benign secondary headaches (35.4-63.2%), whereas potentially life-threatening (LT) secondary headaches are less frequent (2-15.3%).
Many conditions associated with the genesis of headache are under study, and the most classic causes of primary and secondary headache by now may not be sufficient to explain the totality of this phenomenon. Especially the primary headache (independent of other pathologies by definition) could influence the genesis of other pathologies and in turn be influenced by the same, in a negative cycle that leads the patient to the development of different conditions of discomfort.
In this short review we will report the studies of researchers who have tried to connect different states of health to headache, especially linking with psychiatric disturbance.
Keywords: Headache; Migraine; Tension-type headache; Psychological distress; Depression; Anxiety; Comorbidity
Abbreviations: Emergency departments; LT: Life-threatening; TTH: Tension type headache; ICHD-III: International Classification of Headache Disorders
Introduction
Headache is a common disorder in children and adolescents, and it can have a strong impact on school performance [1], being the major cause of absence from school [2], and widely affecting other daily activities [3]. In children under 10 years of age, the overall headache prevalence has been reported to be as high as 56 %. The prevalence increases with age, in fact from mid-adolescence to early adulthood the prevalence of headache can be as high as 91% [4-9].
Headache can be divided into primary (independent of another pathology) or secondary (symptoms of another pathology) recognizing this difference is important to evaluate and plan the appropriate treatment. The most common forms of primary headaches in childhood are migraines and tension headaches (TTH), the other varieties (uncommon) are much rarer. Migraines are further categorized into migraines with and without auras, complicated migraines and migraine variants [10-12]. Migraines have been estimated to affect nearly 75% of children under the age of 15 and have been reported in 3.9% of children between the ages of 7 and 15, with a range from 1.7% in 7-year old children to 5% in 15-year-old children [12,13].
It is essential to know the patient’s history, to build a precise description of migraine attacks, an accurate physical examination that requires a careful neurological investigation.
it is important to ask for all potentially triggering events, their distribution over time without forgetting details such as frequency, severity, duration, disability, other associated symptoms. It is also important to know the family history for the high family penetrance of migraine.
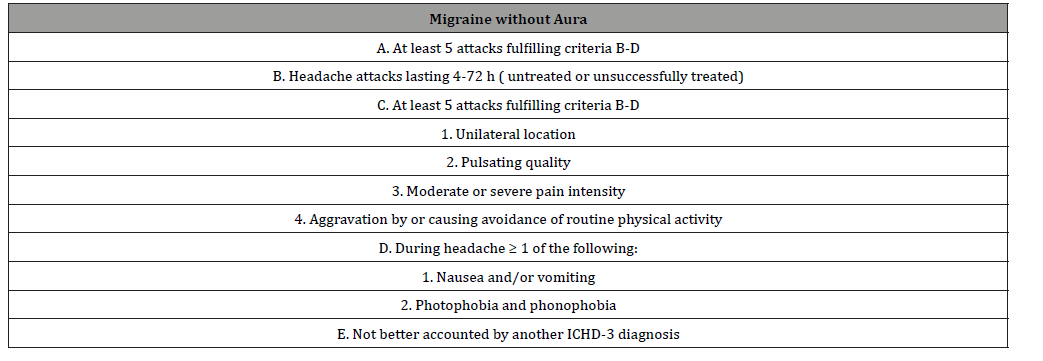
New guiding criteria for migraine (ICHD-III) with and without aura were defined in 2018 by the international headache society (Table 1& 2).
Table 1:ICDH-3 Cephalagia 2018, 38; 1-211. ©International Headache Society.

Table 2:ICDH-3 Cephalagia 2018, 38; 1-211. ©International Headache Society.
Tension-type headache (TTH) has a wide-ranging reported prevalence of 0.9% to 72.3% in children and adolescents [14]. Episodic tension-type headache may have particular features in children. Pain generally starts in the afternoon at school and the child can often carry on with activities despite severe or constant headache. As the headaches are rare or absent during extended holidays, clinical confirmation of the diagnosis may require assessment over these periods. The features of tensiontype headache may change from preschool age to adolescence [15,16]. The red flags that alert the physician to conduct further investigations for tension-type headache include sudden and severe unilateral headache, particularly in the absence of a family history of migraine, which needs computed tomography examination to exclude vascular disorders [15,17]. Secondary headaches are the symptom of an underlying disease, these secondary causes are often not so evident and making correct diagnosis is difficult.
According to the ICHD-III we can divide the secondary headaches into headache attributed to trauma or injury to the head and/or neck, headache attributed to cranial or cervical vascular disorder, headache attributed to non-vascular intracranial disorder.
Headache attributed to a substance or its withdrawal, attributed to infection ,attributed to disorder of homoeostasis, headache or facial pain attributed to disorder of the cranium, neck, eyes, ears, nose, sinuses, teeth, mouth or other facial or cervical structure and headache attributed to psychiatric disorder.
Discussion
The key to diagnosing headache is to recognize the underlying cause and demonstrate a direct cause-and-effect relationship.
In recent years the search for new associations between headache and underlying clinical conditions is becoming increasingly important, for Christopher B Oakley et al. [18] the risk of migraine in childhood is increased in those with obesity and that this risk increases with increasing obesity status [18].
Considering the new data that can be deduced from the literature and previous work, can weight loss therefore be considered a cure for migraine in the obese pediatric patient? Future studies will clarify the issue.
Another one of the most studied disturbance associated to primary headache is the psychiatric disturbance.
For Fearon P et al. [19] in children with frequent headache, there is an increased risk of developing psychiatric morbidity in adulthood [19].
For Grete Dyb et al. [20] taken together, psychological distress and headache often co-exist, the conditions share common risk factors, and empirical data suggest that headache may induce psychopathology and vice versa [20].
Mereover Rapoff MA et al. [21] demonstrate that in many cases, it is sufficient applying a simple cognitive approach with emphasis on identifying triggers for headache, modifiable lifestyle factors, and proper advice of medication and acute treatment. In addition, supplementary self-guided cognitive-behavioral self-management strategies might be a promising approach [21].
Moreover, C Romano et al. [22] report that the frequency of primary headache associated with emotional and behavioral disorders in children founding an association between headache and anxiety/depression (27% of children in the headache group vs. 8.3% of children in the control group, p<0.001).
Finally, the risk analysis showed that odds of anxiety and depression in children in the headache group is 4.20 times more frequent than in children in the control group [22].
Conclusion
As we can see, there is a growing interest in causes that ,although are independent from the genesis of the headache, seem to trigger a feeding pathological cycle, and in turn be fed by the headache itself.
Will chronic primary headache play an increasingly important role in association with the state of anxiety and depression? And is it possible to think of a headache secondary to a primary state of anxiety and depression?
We should also consider the emotional and psychiatric sphere of the headache patient and we could often realize that the therapy of an anxiety disorder could heal a chronic headache, and a therapy for a chronic headache could treat the underlying anxiety state through approaches that also include lifestyle changes.
The scientific literature continues in its investigation on the still unknown causes/comorbidity of headache, it is very likely that in the following years many innovations will be included among the causes of headache.
Acknowledgement
The document has been edited for proper English language, grammar, punctuation, typos error and spelling by AME (American manuscript editors USA. Certificate Verification Key: 234-589-107- 043-904: Project Number: 72815).
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is coherent with these guidelines.
Conflict of Interest
No conflict of interest.
References
- Souza-e-Silva HR, Rocha-Filho PA (2011) Headaches and academic performance in university students: cross-sectional study. Headache 51(10): 1493-1502.
- Abu-Arefeh I, Russell G (1994) Prevalence of headache and migraine in schoolchildren. BMJ 309(6957): 765-769.
- Barea LM, Tannhauser, Rotta NT (1996) An epidemiologic study of headache among children and adolescents of southern Brazil. Cephalalgia 16(8): 545-549.
- Deubner DC (1977) An epidemiologic study of migraine and headache in 10–20 year olds. Headache 17(4): 173-180.
- Sillanpaa M (1983) Changes in the prevalence of migraine and other headache during the first seven school years. Headache 23(1): 15-19.
- Liner MS, Stewart WF, Celentano DD, Ziegler D, Sprecher M (1989) An epidemiologic study of headache among adolescents and young adults. JAMA 261(15): 2211-2216.
- Stewart WF, Linet MS, Celentano DD, Van Natta M, Siegler D (1991) Age and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiol 134(10): 1111-1120.
- Sillanpaa M (1983) Prevalence of headache in pre puberty. Headache 23(1): 10-14.
- Abu-Arafeh I, Razak S, Sivaraman B, Graham C (2010) Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol 52(12): 1088-1097.
- Headache Classification Subcommittee of the International Headache Society (2004) The International classification of headache disorders. Cephalalgia 24(Supply 1): 1-160.
- Shah DH, Karla V (2009) Pediatric Migraine. Int J Pediatr 424192.
- Hershey AD (2010) Current approaches to the diagnosis and management of pediatric migraine. Lancet Neurol 9(2): 190-204.
- Winner P, Hershey AD (2007) Epidemiology and diagnosis of migraine in children. Curr Pain Headache Rep 11(5): 375-82.
- Wöber-Bingöl C (2013) Epidemiology of migraine and headache in children and adolescents. Curr Pain Headache Rep 17(6): 341.
- Seshia SS, Abu-Arafeh I, Hershey AD (2009) Tension-type headache in children: the Cinderella of headache disorders! Can J Neurol Sci 36(6): 687-695.
- Anttila P (2006) Tension-type headache in childhood and adolescence. Lancet Neurol 5(3): 268-274.
- Parisi P, Papetti L, Spalice A, Nicita F, Ursitti F, et al (2011) Tension-type headache in paediatric age. Acta Paediatr 100(4): 491-495.
- Christopher B Oakley, Ann I Scher, Ana Recober, B Lee Peterlin (2014) Headache and Obesity in the Pediatric Population Curr Pain Headache Rep 18(5): 416.
- Fearon P, Hotopf M (2001) Relation between headache in childhood and physical and psychiatric symptoms in adulthood: national birth cohort study. BMJ 322(7295): 1145.
- Dyb G, Stensland S, Zwart JA (2015) Psychiatric Comorbidity in Childhood and Adolescence Headache. Curr Pain Headache Rep 19(3): 5.
- Rapoff MA, Connelly M, Bickel JL, Powers SW, Hershey AD, et al. (2014) Headstrong intervention for pediatric migraine headache: a randomized clinical trial. J Headache Pain 15(1): 12.
- Romano C, Cho SY, Marino S, Raucci U, Fiumara A, et al. (2020) Primary headache in childhood associated with psychiatric disturbances: an update. European Review for Medical and Pharmacological Sciences. Eur Rev Med Pharmacol Sci 24(12): 6893-6898.
-
Sapuppo A, Marino L, Sciuto S, Fontana A, Pavone P. Primary Headache in Childhood Associated with Psychiatric Disturbance: A Mini Review. Glob J of Ped & Neonatol Car. 2(4): 2020. GJPNC.MS.ID.000541.
Marsh criteria, Duodenal biopsy, Anti ttg A, Patient, Celiac disease, Children, Endoscopy, Anti ttG A
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






