 Research Article
Research Article
Clinical Outcome of Posterior Wall Acetabular Fractures Treated by Open Reduction and Internal Fixation
Mahmoud I Abdel-Ghany* Ayman K Saleh Tohamy G Hassan and Moahmmed A Al-Dinasoury
Department of Orthopedic, Al-Azhar university, Faculty of Medicine for Girls, Cairo, Egypt
Mahmoud I Abdel-Ghany, Department of Orthopedic, Al- Azhar university, Faculty of Medicine for Girls, Cairo, Egypt.
Received Date: January 01, 2021; Published Date: March 5, 2021
Abstract
Background: Posterior wall acetabular fractures are the most common type of fracture acetabulum. Surgical treatment is the standard solution for displaced posterior acetabular wallfractures.
Study Design: This retrospective study evaluatesclinical and radiologic outcomes of open reduction and internal fixation in patients with posterior wall acetabular fractures.
Patients and methods: This study includes49 cases (37 males (75.5%) and 12 females (24.5%)), average age was 32.1 Years.All patients were admitted in both hospitals andunderwent surgical treatment of posterior wall acetabular fractures. All patients treated at Al-Zahraa University Hospital and Heliopolis hospitalbetweenMarch2011andJanuary2019. All patients had history of fall from height or car accident.
Result: Clinicaloutcomes were assessed by Modified Merl d’Aubejan Score (MMS) after surgery at the time of the study and evaluation of general condition and return to previous activities. The final clinical outcome was excellent in 32 cases (65.3%), good in 13 cases (26.5%), fair in 2 cases (4.1%) and poor in 2 cases (4.1%). Finally, both excellent and good outcome were considered satisfactory 45 cases (91.8%) and both fair and poor outcome were considered as unsatisfactory 4 cases(8.2%). Cases with satisfactory outcome had less associated injury and younger in age. Five cases (10.2 %) had superficial infection that treated by antibiotics and dressing,one case (2.05%) had sciatic nerve injury and two cases (4.1%)had AVN femoral head were reporte 654kd.
Conclusion: posterior wall acetabular fractures had favorable outcome with open reduction and internal fixation. Optimum time for surgery is earlier as possible, however early mobilization is preferred it may depends on the associated injury and treatment of that injuries. At least static exercise should be tried to improve the clinical outcome and minimize the complication of morbidity.
Keywords: Acetabular fracture; Posterior wall acetabular fracture, Internal fixation
Mini Review
Posterior wall acetabular fractures are the most common type of acetabular fractures, accounting for approximately 35–47% of all acetabular fractures [1]. Acetabular fractures constitute a challenging joint reconstruction problem, as the aim of surgery is to reform and creating the concave articulating surface through precise open reduction and stable fixation to achieve as possible as normal hip function [2]. Mostly fractures results of high-energy trauma with the femoral head transmitting axial load through the acetabulum, commonly seen in car accidents when the knee contacts the dashboard [3]. An accurate reduction with anatomical restoration of an acetabular fracture is probably the single most important factor in achieving a satisfactory outcome [4].
There are factors founded to predict outcome, patient age younger than 40 years; simple fractures and absence of damage to the femoral head. Possible influential factors that makes unsatisfactory outcome included additional injuries, immediate complications, quality of reduction, heterotopic ossification, ipsilateral femoral fracture, and sciatic nerve damage [5,6].
Patients and Methods
This study includes49 cases (37 males (75.6%) and 12 females (24.5%)), their age ranged from 19-51 years with average age was 32.1 years who had had fracture posterior wall acetabulum. There were 14 patients (28.5%) fell from height and 35 patients (71.4 %) had car accidents (Table 1). Associated fractures were observed in 28 patients (57.1%) fracture upper shaft femur, calceneal fractures and humeral shaft fractures, other brain, abdominal and chest injuries were recorded (Table 2).All patients underwent open reduction and internal fixation of the acetabular fractures and the associated fractures. All surgeries had been performed by the same surgical team at Al-Zahraa University Hospital and Heliopolis hospital between 2011- 2019. All patients were informed by the procedure and expected complications and signed consent was obtained from all of them. The study protocol was approved by local ethical committee of Faculty of Medicine for Girls(FMG).
Methods
All patients treated surgically “open reduction and internal fixation (ORIF)” by reconstruction plate through a Kocher-Langen beck approach. Patient position for all patients was lateral position with anterior tilt 10 degree forward. Care should be taken at dividing the external rotators to avoid damage to the posterior ascending branch of the medial femoral circumflex artery, supplying the femoral head. Identification and protection of sciatic nerve were achieved by using fingertip of assistant to trace sciatic nerve proximally and medially towards the greater sciatic notch. Open reduction of the displaced fragments with its soft tissue pedicle and temporary with K-wires fixation. Definitive fixation performed by using 4 mm lag screw and 3.5 reconstruction plate. Suction drain used for 48 hours. Prophylactic antibiotics (Ciphotriaxone 1 gm IV) usually started 2 hours before surgery and were continued for 3 days after surgery unless another surgery for the associated injuries (Table 1&2).
Table 1: Baseline characteristics of patients with fracture posterior wall Acetabulum (No = 49).
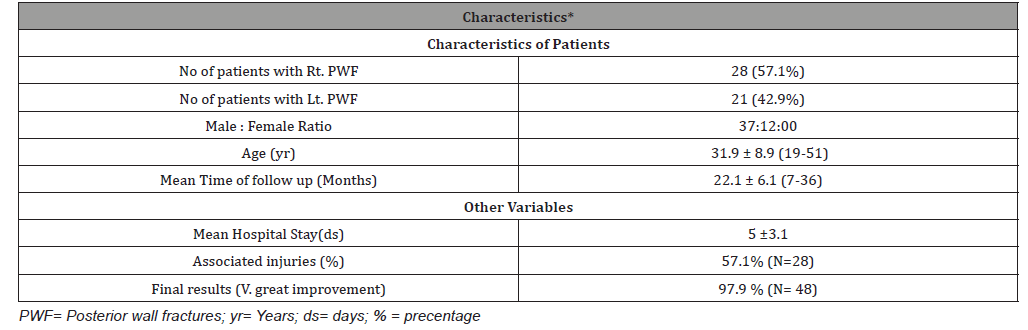
Table 2: Associated injuries with fracture acetabulum.
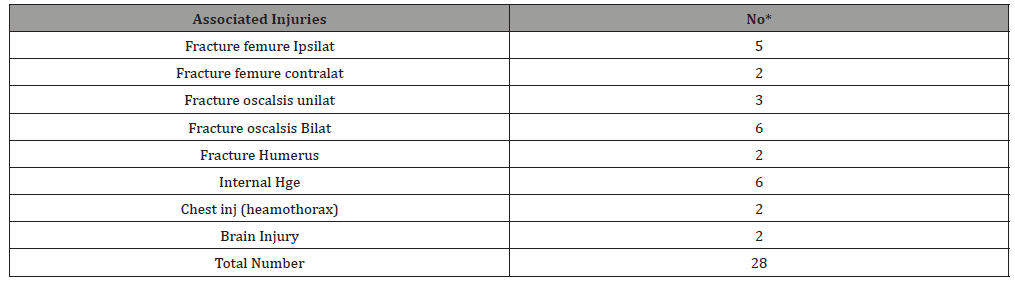
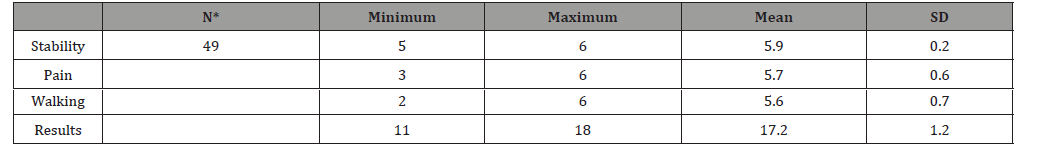
Table 3: Modified Merle D Aubigne mean score for all patients.
Blood loss during surgeries was ranged from 340-700 cc with mean 505 ±97.5cc. and times of surgery were ranged from 45-90 minutes with average 68.3 minutes.
All patients kept in bed for 2-3 weeks, pain-free assisted quadriceps, hips and knee-flexion exercises on the second day after surgery. Mobilization without weight bearing of affected side for more 3 weeks. Partial weight bearing with crutches was allowed 6-8 weeks after surgery.
Plain X-ray of the pelvis were obtained directly after surgery, two months, five months and one year, then yearly for the follow up period. Follow up X-rays (three views) were examined early for loss of reduction of fracture fragments and late for bone healing, plate or screw breakage, screws pull out.
Enoxoparine (Low molecular Heparin) 5mg/kg Sc twice / day were used for all patients after admission for prevention of thrombo-embolic diseases. Indomethacin 25 mg. three times /d was also used for prevention of heterotropic ossification.
Result
All patients were followed up after surgeryclinically by Modified Merle d’Aubigné (MMA) score [7,8] and SF-36 score[9,10] for quality of life after pelvic injury. Follow up period ranged from12- 36 months with average 22.3 months.
According to Modified Merle d’Aubigne score [8], Stability score were ranged from (5-6) with mean score 5.9 SD± 0.2; pain score ranged from (3-6) with mean 5.7 SD±0.6 and ability to walk score ranged from2-6 with mean score 5.6 SD±0.5. The final results mean score 17.2 SD±1.2 and ranged from [11,18] (Table 3).
As a clinical outcome after surgery according to Modified Merle d’Aubigne score there were 48 patients (97.9%) had score more than 12 and considered as very great improvement one patient (2.1%) had score 11 and considered as great improvement.
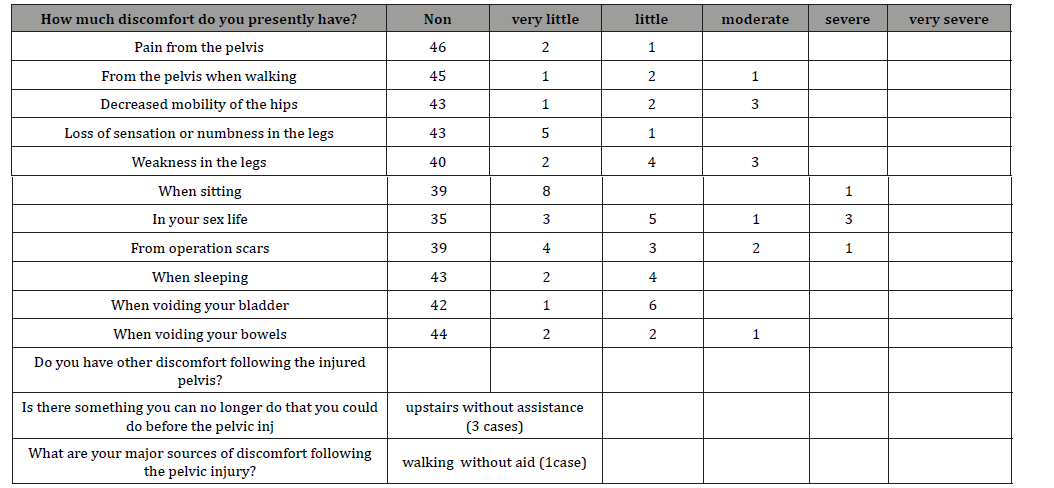
According to (SF-36) Questionnaire [11,12] for outcome of hip injury pain is improved completely in 46 patients (93.8%), two patients (4.08 %) had very little pain and one patients (2.04 %) developed severe pain at 6 months. Ability to walk 45 patients (91.8 %) had no limitation in their normal walking distance, however 1 patient (2.04 %) had very little limitation in normal walking distance and 2 patients (4.08 %) reported little difference in walking distance and one patient (2.04 %) had severe affection of his walking distance and needs assistance in his walk. Regarding hip mobility there were 43 patients (87.7%) satisfied with hip mobility, 1 patient (2.04%) reported very little limited mobility,two patients (4.08%) had little mobility affection and three patients (6.1%) had moderate limited mobility of the affected side. There werelittle sensory disturbance reported in 5 patients (10.2%), one patient (2.04%) had little sensory disturbance which improved within 6 months by medications. There were 43 patients (87.7%) had no little sensory disturbance. There were 40 patients (81.6%) normal power of legs according to their feeling 2 patients (4.08%) felt little weakness, 4 patients (8.1%) and 3 patients (6.1%) felt moderate weakness in their affected leg. However by manual muscle test (MMT) there were 46 patients (93.6%) had no weakness (G5) and 3 patients (6.1%) had little differences (G4) muscle strength.
There were no urinary disturbances in 42 patients (86.7%), 7 patients 9 (14.3%) had complaint from dysuria which may be related to previous urinary infection or catheterization at ED department. We had 44 patients (89.7%) had no bowel disturbance however 5 patients (10.2%) reported little to moderate bowel disturbance. There were 3 patients (6.1%) reported upstairs difficulties one (2.04) of them has severe disability in up and downstairs this case also complaining of difficulties in walking without assistance (Table 4).
Table 4: (SF-63) questionnaire for all patients at the final follow up.
Activity daily living (ADL) wereafter surgeries reported by Katz and Akpom(13) to determine the success of surgery and its relations to activity of patients as an index for return to normal activity (Table 5).
Table 5: Functional status of patients with hip fractures as defined by Katz and Akpom.

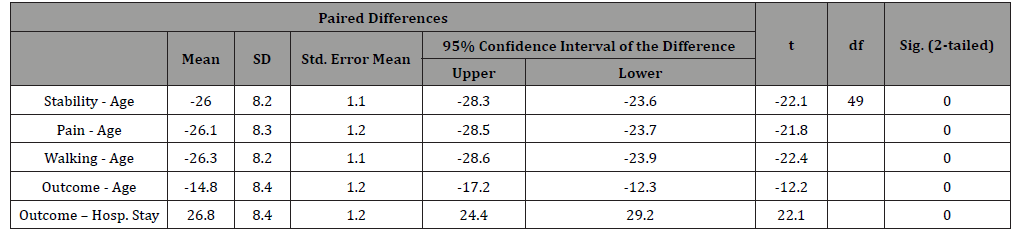
Table 6: Paired Sample T test for correlation of all parameter of Merl d’Aubigne score.
Radiographic examination for the patients was obtained after surgery, then after 2 months, six months then at one year. Unless there is a complaint follow up X-Ray were obtained every year for the next years. We considered the consolidated fragment associated with loss of pain and return of normal painless function without loosening of screws breakage nor femoral head subluxation considered an excellent outcome. All patients had union with improvement of mobility and function. One patient (2.04 %) had developed three months after surgery severe pain and disability by plain X-ray there is head osteopenia with remarkable finding suggesting avascular necrosis of the femoral head (AVNFH). This patient treated by removal of the plate and total hip arthroplasty.
Statistical Analysis: all data of the patients collected, tabulated and statistic analysis for the collected data and analyzed by using SPSS v 16. Inc., USA Quantitative data were expressed as mean and standard deviation, while qualitative data were expressed as relative frequency and percent distribution. Unpaired Sample T test used for comparison and p value < 0.05 was considered significant (Table 6).
Statistical analysis with paired simple T-test by correlation of all items of Merle d’Aubigne score (stability, Pain, and ability to walk) and outcome to age and to the hospital stay shows highly significant differences (< 0.005)in all parameters (table 6). The final clinical outcomes according to Modified Merle d’Aubigne score showed very great improvement (Score more than 12) in 48 patients (97.9%) and one case (2.1%) had less than 12. However radiological follow up shows complete consolidation of fractures with painless motion. Some patients had complained from unremarkable weakness of leg or some parasthesia were improved by neurotropic therapy and physiotherapy to strengthen the hip and thigh muscles.
Discussion
Posterior wall fractures are common acetabular fractures with an expected incidence of approximately 17% [6]. Severe pelvic and acetabular fractures are frequent when jumping from great height due to the high energy involved [14]. In a study comparing survival jumpers and fallers Teh et al [15] reported a higher proportion of pelvic injuries in jumpers when compared to fallers.
We have in this study there were males 75.5% and females 24.5%;Gänsslen et al(16) Zinghi et al [17] found similar results as they reported that the majority of patients were men. There were 28.5% fell from height and 71.4 % had car accidents; Parasartritha and Chaivanichsiri [18] reported 14.7 % fell down and 85.3 % due to Road Traffic Accident (RTA) in their study however their associated injuries were higher as they were reported 60.3 % associated injuries. Gänsslen et al [16] and Praveen et al, [19] had similar data to our study as they reported 78.9 % RTA and 21.1 % fell from heights, and associated injuries in 57.9 % of their series. In our study we had a similar incidence of associated fractures as we had 57.1%.
Average time between injury and surgery 5.2 days and mean blood losses recorded in our study as 505 ±97.5cc while average times of surgery were 68.3 minutes. This recorded data is nearly the same recorded by Magu et al (20)Keel et al [21] as they reported average time between injury and surgical procedure 4.2±1.7 days and average operative time 105 min. Gänsslen et al [16] reported mean operative time was 190±90 minutes, intraoperative blood loss averaged 855±700 ml. Borg [22] reported in his study that surgery was performed average 6 days after the trauma. There are paucity of literature exists regarding exact timing of acetabular fixation with worsening results when surgical intervention is undertaken after 3 weeks [23].
Enoxoparine 5mg/kg Sc. twice /day were used for all patients for prevention of thrombo-embolic diseases. Indomethacin 25 mg. three times /d was also used for prevention of heterotropic ossification. Letournel and Judet reported dangerous thromboembolic complication and thrombo phelebitis however patients receive anticoagulants [24]. We didn’t encounter such complications as patient moving in his bed and with aids non-weight bearing walk. Tile recommends use of anticoagulants (low molecular weight heparin) as soon as it is safe, usually within 24H. He recommends to use it till surgery, and continued postoperatively. Screening for DVT prior to surgery is essential, if prophylactic measures have not been instituted as above [25].
Indomethacin used for prevention of heterotropic ossification in our study as mentioned however we didn’t notice any case of heterotropic ossification. This drug usage in the same dose for the same purpose reported by Meena et al as they used Indomethacin 25 mg TID for 6 weeks for heterotopic ossification prevention in patients who were operated through extended iliofemoral approach or combined approaches [26]. Karunakar et al in their comparative study to use indomethacin versus placebo after posterior acetabular fracture concluded that they can’t demonstrate a statistically significant reduction of heterotopic ossification with the use of indomethacin when compared with a placebo [27].Burd et al compared indomethacin versus radiation for prevention of heterotropic ossifications and they concluded that They mention that both are effective in treatment however there is no significance difference between both regime in prevention of hterotropic ossification [28].
According to Modified Merle d’Aubigne score we have mean score 17.2 SD±1.2 points and 97.9% of patients had score more than 12 points and considered as very great improvement however 2.1% had score less than 11 points and considered as great improvement. This results is comparable to results reported in several studies [16,29,30] mean Merle d‘Aubigné score 15.4 ± 2.8 points with 31.3% of patients with a perfect functional result, 25.4% with a good, 28.4% with a moderate and 14.9% a poor functional outcome.
Functional outcome in this series according to (SF-36) Questionnaire [11,12] for outcome of hip injury pain is improved completely in 93.8%, however 6.2% of patients had some pain. Ability to walk there were 91.8% of patients had nearly normal walking distance, however 8.25 of patients reported difficulties of their walking distance which may needs assistance for long distance.
Outcome of surgery can be predicted for the fracture acetabulum and pelvic injury. Age, gender and fracture pattern were not found to affect the outcome significantly [26]. However, time of surgery, anatomical reduction and fixation are surgeon dependent factors and can affect the eventual outcome [31,32,33].
Poor functional outcome was 14.9 %, there were 2 cases around fifties and other either has hip dislocation or there is a time between fracture and surgery. Several authors mentioned that outcome of acetabular fracture in elderly individuals is suboptimal [26]. Hip dislocation wasrecorded in 2 patients (4.08%)whohad outcome less than 11 Merle d‘Aubigné score. Hip dislocation has detrimental effect on the eventual functional outcome; it not only compromises vascularity of the femoral head but also makes the surgical reconstruction of the acetabulum more challenging [32].
We have noticed the earlier surgical intervention the better outcome. Several authors suggested that earlier reconstruction leads to better reduction [34-36]. Early mobilization of patients by doing simple exercise in bed dynamic and static improving the outcome of surgery. This is agreeing with Vallier et al, as they reported that mobilizing patients early could be expected to limit secondary morbidity [35].
Conclusion
Fracture acetabulum of one of the challenging fractures; its complications and associated injuries makes treatment more sophisticated.Surgical treatment is suitable for most of cases specially those whom had displacement of the fractures, subluxation or dislocation of head femur. Difficulties of surgeries is expected as learning curve to be expert surgeons may be taking more time than other fractures. Optimum time for surgery is earlier as possible, however early mobilization is preferred it may depend on the associated injury and treatment of that injuries. At least static exercise should be tried to improve the clinical outcome and minimize the complication of morbidity.
Conflict of Interest
Authors declare any conflict of interest for this article.
Ethical Committee
This study is approved by local ethical committee of our institution. All patients signed a consent as routine before surgeries to use their data for research purposes.
References
- Kreder HJ, Rozen N, Borkhoff CM (2006) Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. JBJS 88(6): 776-782.
- Rockwood CA (2006) Rockwood and Green’s Fractures in Adults. (6th) Heckman JD, Court-Brown C Bucholz RW, Philadelphia PA Lippincott Williams & Wilkins 1665–1714.
- Borg T, Berg P, Fugl-Meyer K, Larsson S (2010) Health-related quality of life and life satisfaction in patients following surgically treated pelvic ring fractures. A prospective observational study with two years follow-up. Injury 41(4): 400-404.
- Kim H, Tang C, Krishnamoorthy S (1994) Operative treatment of acetabular fractures. Singapore Med J 35: 137-176.
- Liebergall M, Mosheiff R, Low J, Goldvirt M, Matan Y, et al. (1999) Acetabular fractures Clinical outcome of surgical treatment. Clin Orthop Relat Res 366: 205-216.
- Giannoudis PV, Tzioupis C, Moed BR (2007) Two-level reconstruction of comminuted posterior wall fractures of the acetabulum. JBJS 89(4): 503-509.
- Merle, D Aubigne Traumascores 2016.
- Ugino FK, Righetti MC, Alves PLD, Guimaraes PR, Honda KE, et al. Evaluation of the reliability of the modified merle d’aubigné and postel method. Acta Ortop Bras 20(4): 213-217.
- McHorney CA, Ware JE, Raczek AE (1993) The MOS 36-Item Short Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31(3): 247-263.
- Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36) I Conceptual framework and item selection. Med Care 30(6): 473-483.
- Taft C, Karlsson J, Sullivan M (2001) Do SF-36 summary components cores accurately summarize subscale scores? Qual Life Res 10(5): 395-304.
- McHorney CA, Ware JE, Raczek AE (1993) The MOS 36-Item Short- Form Health Survey (SF-36): II. Psychometric and clinical tests of validityin measuring physical and mental health constructs. Med Care, 31(3): 247-263.
- Katz S, Akpom CA (1976) Index of ADL. Med Care 14(supp 5): 116-118.
- Borg T, Holstad M, Larsson S (2010) Quality of life in patients operated for pelvic fractures caused by suicide attempt by jumping. Scandinavian Journal of Surgery 99(3): 180-186.
- The J, Firth M, Sharmaa, A Wilson, R Reznek, O Chan (2003) Jumpers and fallers: a comparison of the distribution of skeletal injury. Clin Radiol 58: 482-486.
- Gansslen A, Hildeband F, Krettek C (2013) Transverse + Posterior Wall Fractures of the Acetabulum: Epidemiology, Operative Management and Long-Term Results. Acta Chirurgiae Orthopaedicae Et Traumatologiae Cechosl, 80(1): 27-33.
- Zinghi G, Briccoly A, Bungaro P, Davoli O, Ponziani L, et al. (2004) Fractures in the vertical plane. GF Zinghi. Fractures of the pelvis and acetabulum. Stuttgart : Thieme-Verlag Stuttgart 157-163.
- Prasartritha T, Chaivanichsiri P (2013) The study of broken quadrilateral surface in fractures of the acetabulum. International Orthopaedics (SICOT) 37(6): 1127–1134.
- Praveen SK, Venkatachalam K, Mani A, Karrun P, Bheeshma B (2016) A Prospective Study of Open Reduction and Internal Fixation of Complex Acetabular Fractures. Sch Acad J Biosci 4(10-B): 917-133 .
- Magu NK, Gogna P, Singh A, Singla R, Rohilla R, et al. (2014) Long term results after surgical management of posterior wall acetabular fractures. J Orthopaed Traumatol 15: 173-179.
- Keel, BJM S, Tomagra MH, Bonel AK, Siebenrock DJ, et al. (2014) Clinical results of acetabular fracture management with the Pararectus approach. Injury 45(12): 1900-1907.
- Borg T (2011) Pelvic ring injury and acetabular fractures, quality of life following surgical treatment. comprehinsive digital summaries of Uppsala Dissertations from faculty of Medicine 956, Acta Universitatis Upsalienenis 1-66.
- Lin YC, CH Chen, HT Huang, JC Chen, PJ Huang, et al (2008) Percutaneousante grade screwing for anterior column fracture of acetabulum with fluoroscopic based computerized navigation. Arch Orthop Trauma Surg 128(2): 223-226.
- Letournel E, R Judet (1981) Treatment of Specific Types of Fracture. (ed.) Eison RA Fractures of the Acetabulum. Springer-Verlag Berlin Heidelberg 21: 255-210.
- Bartlett SC, Helfet LD (2015) Techniques , Specific surgical approaches and technique. [book auth.] M. Helfet ID Tile and Kellam FJ. Fracture of pelvis and acetablum. 4th Thiems 6: 507-510.
- Meena UK, Tripathy SK, Sen RK, Aggarwal S, Behera P (2013) Predictors of postoperative outcome for acetabular fractures. Orthopaedics & Traumatology: Surgery & Research 99(8): 929-935.
- Karunakar MA, Sen A, Bosse MJ, Sims SH, Goulet JA, et al. (2006) Indometacin as prophylaxis for heterotopic ossification after the operative treatment of fractures of the acetabulum. JBJS 88-B (12): 1613-1617.
- Burd TA, Lowry KJ, Anglen JO (2001) Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. JBJS 83-A(12): 1783-1788.
- Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. JBJS 78-A: 1632-1636.
- Mitsionis GI, MG Lykissas, E, Motsis D, Mitsiou TA, Gkiatas I Xenakis AE, et al. (2012) Surgical management of posterior hip dislocations associated with posterior wall acetabular fracture: a study with a minimum follow-up of 15 years. J Orthop Trauma 26(8): 460-465.
- Mears DC, Velyvis JH, Chang CP (2003) Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res 407: 173-186.
- Bhandari M, Matta J, Ferguson T (2006) Predictors of clinical and radiological outcome in patients with fractures of acetabulum and concomitant posterior dislocation of hip. JBJS 88(12): 1618-1624.
- Ferguson TA, Patel R, Bhandari M, Matta JM (2010) Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. JBJS 92(2): 250-257.
- Plaisier BR, Meldon SW, Super DM, Malangoni MA (2000) Improved outcome after early fixation of acetabular fractures. Injury 31(2): 81-84.
- Vallier HA, Cureton BA, Ekstein C, Oldenburg FP, Wilber JH (2010) Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma 69(3): 677-684.
- Briffa N, Pearce R, Hill AM, Bircher M (2011) Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg 93(2): 229-236.
- Letournel E, Judet R (1993) Fractures of the acetabulum . [2nd ] Elson R, New York, NY: Springer 29-581.
- Sagi HC, Jordan CJ, Barei DP (2014) Indomethacin prophylaxis for heterotopic ossification after acetabular fracture surgery increases the risk for non-union of the posterior wall. J Orthop Trauma 28(7): 377-383.
-
Mahmoud I Abdel-Ghany, Ayman K Saleh Tohamy G Hassan, Moahmmed A Al-Dinasoury. Clinical Outcome of Posterior Wall Acetabular Fractures Treated by Open Reduction and Internal Fixation. Glob J Ortho Res. 3(1): 2021. GJOR.MS.ID.000551.
-
Acetabular fracture, Posterior wall acetabular fracture, Internal fixation, Urinary infection, Surgery, Avascular necrosis, Physiotherapy, Hip, Thigh muscles, Thromboembolic, Heterotropic
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






