 Research Article
Research Article
External Cortical Femoral Implant in ATHP A Long Term Follow Up of a Clinical Case
Yves Cirotteau, Neuilly Sur Seine Hospital, Courbevoie, France.
Received Date: July 15, 2019 Published Date: August 22, 2019
Summary
This article will show the clinical and surgical results of a patient who was operated of both hips for a severe coxarthrosis. The follow up is 30 years for the right hip and, and 26 years for the left hip. The woman was treated according to a new concept of the femoral stem. The goal of this concept is to respect-as close as possible-the physiological bone metabolism. The femoral implant, instead of being fixed in the medullary canal, is fixed on the femoral lateral cortex of the shaft to secure a fixation during all the patient’s life, whatever his age.
Abstract
The total Hip Arthroplasty of Sir John Charnley was a revolutionary step in the treatment of hip diseases. Currently, the long-term follow-up of such a prosthesis can be estimated from fifteen to twenty years. The question is: is that delay sufficient to treat young patients with severe hip disease. In a recent publication, Rik Huiskes claims that since Charnley, no so-called innovation has either scientific proof in real efficiency or in terms of longer longevity. This should not be a surprise for all total hip prothesis are placed in the medullary canal, either with or without cement. In fact, the so-called innovations are minimal modifications in the design of the stem. It is obvious that if these modifications are not efficient, one should not follow this line of research. It seems that almost everything has been written on total hip arthroplasty failure. We must therefore work in another direction, with other criteria.
Suppose that it is the bone, with all its specifications, which is the possible reason for that long-term failure. Is the “kuntscher” imperial road, the only highway to deal with the shaft of a long bone? A new concept, a new philosophy to fix a hip stem prosthesis on the femoral shaft becomes apparent. In other words, according to this new scientifically point of view, the mechanical aspect of a stem hip prothesis is no longer of interest. If the stem can be placed inside the medullary canal, why could not it be fixed outside of the shaft, for example on the external part of the diaphyseal cortex, below the periosteal layer? It seems that searcher should work today on bone physiology, instead of working on any mechanical aspect of surgical fixation in the medullary canal. Using the physiological properties of a living bone could be the answer to avoid any failure of the stem all the life’s patient long.
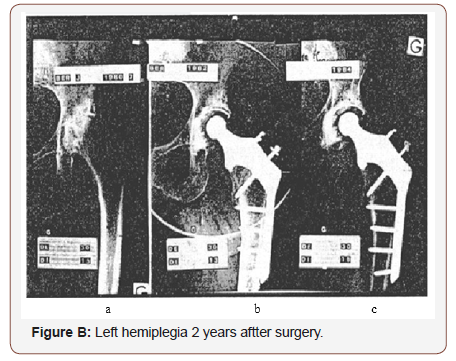
Pathological Modifications of the Femoral Cortices
Everyone, in his practice, had patients with more or less severe brain dysfunction, one is hemiplegia [1]. What could happen for the patient from an orthopedic point of view, on the lower limb when such a disease happens? The reduced use of the limb reduces the pressure on the bearing bone and, from a physiological point of view, a reduction of the mineralization. The bone becomes osteoporotic [2]. The physical phenomenon is reversible when the pressure conditions are restored. Here are two examples. This patient had a right haemorrhagic stroke few years ago. He had a left hemiplegia and spent a long time in physiotherapy due to the difficulty to walk. Note the thin both femoral cortical due to the bad utilization of the left lower limb (Figure a). Few years later, he recovered a best walk. Note the very good thickening due to the best support of his body weight by the limb (Figure b). Adversingly, despite the severe coxarthrosis note the good thickness of the femoral cortex before surgery (Figure a, b). Few years later the patient had a hemiplegia. Note the increasing diameter of the femoral medullary canal (Figure c). What would have happened if an intramedullary implant was settle in it?

Scientific Reasons of this New Concept
The choice of this implant’s design was done in the aim of a more physiological respect of the bone structures [3-5].
a) The joint elasticity is mainly due to the cancellous bone of a joint. Most of the intra-medullary canal implants destroy it. In this case the cancellous bone is in the upper femoral metaphyseal neck, more or less in totality (Figure a, b).
b) The bone marrow has one of the most important roles in bone physiology: vascularization, cells of bone remodeling, blood cells, proteins and minerals are the major actors of the normal bone life.
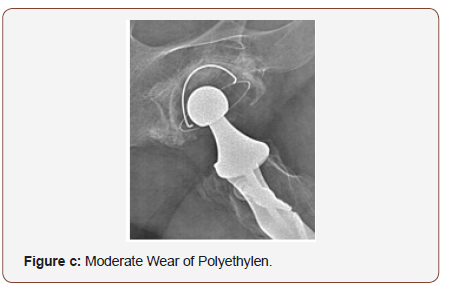
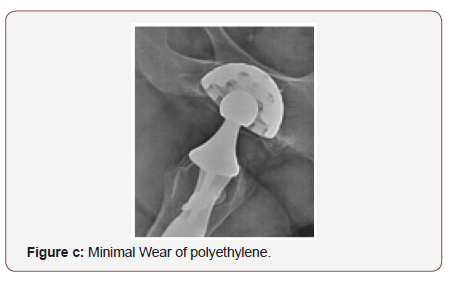
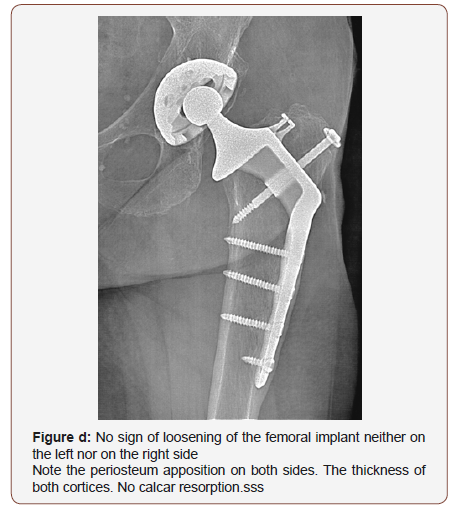
c) The periosteum is acting all lifelong (even after 100 years) and covers all foreign bodies which are fixed on the shaft, keeping a fixation stronger and stronger by time (Figure c, d).
d) The pressure on the calcar is necessary to increase and maintain it thickness. A large crown on the upper part of the implant rests firmly there so that there is no resorption [8-9].
Minimal Resection of the Cancellous Bone
To fix in the upper femoral metaphysis the prothesis needs a very few cancellous bone removals as shown on the drawing. It keeps the elasticity of this part of the femur (Figure a, b).
Technical procedure
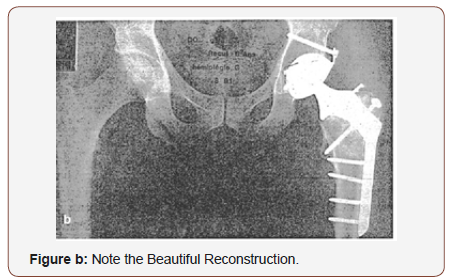
A cemented Charnley’s cup in polyethylene was cemented in the acetabulum. An external stem implant in titanium was fixed on the lateral cortex of the femoral shaft, below the periosteum. A 22,2 mm diameter of the head was used on the right side. Four years later, a non-cemented metal back acetabulum with a 22,2 diameter of the head was placed on the left side. Insert in polyethylene. A lateral femoral Implant in titanium was screwed. Screws of 5 mm of diameter for the femoral shaft, 6 mm of diameter to fix the greater trochanter.
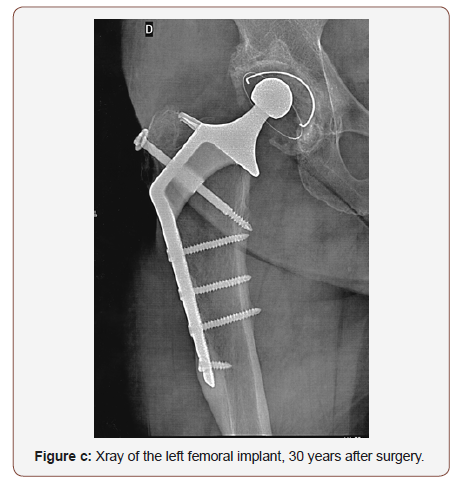
Clinical story and examination
Me T… Françoise is Born the 04 12 1938 - Her Height is 1.59m, her Weight is 59kg. This 80-year-old patient had a bilateral coxarthrosis. When she was 51 years old, in 1989, she was operated on the left side. Four years later, a THP as placed on the right side in 1993. She was seen in clinic office in May 2019. Follow up: 30 years on the right side Follow up: 26 years on the left side She has no pain. She can climb stairs up and down without difficulty. Over three floors, she uses the ramp stairs. She walks without help as long as she wants. One hour without stop She walks without limping.
PM: One hour, without stop in a quiet walk. She has a normal life.
She practices Sports Taï chi twice a weel, one hour with other members.
She goes in holydays either vacancies aux Canaries, Greece, dans les Pyrénées, 0 Saint Jean de luz. She is a grand-ma keeper for her Little children’s daughter on sunday.
She Plays piano, and sing in a chorus opera
She Has a lot of additional activities
Mobility: Left: 140 0 - 35 20 - 20 20
Right: 140 0 - 40 40 - 30 20
Functional scores
Postel-Merle d’Aubigné (PMA) Pain, Mobility, Walk 4 grades: 18 excellent. Harris hip score: Douleur, function, mobilité, absence de déformation Score jusquà 100: 90-100: excellent. Oxford hip score: Activities of the daily Life. Auto-administrated survey with12 items giving a score: 42-48: excellent.
Discussion
The first planning was to start with a well-considered definition of the goal expected. It was to secure the femoral implant on its support so that it would stay all day long, as long as patient’s life, without physical activity limitation. The second question was followed by the development of an effective strategy. Once establishing the goal and the strategy, do we have worked backwards to identify the next steps? Have we reach the goal expected? Can we be sure that the fémoral implant will be aware of complications in 100%.
In fact, the purpose is to answer to three questions:
a. Does bone physiology have been respected? The answer is yes concerning the cancellous bone, the femoral cortices, the role of the periosteum. There was no calcar resorption.
b. Do we have had any mechanical complications such as: broken screws or broken plates. Yes, in a very small cases, some screws fixing the greater trochanter broke. If the osteotomy of this apophysis is consolidated, nothing will happen. In some case the lateral part of the broken screws must be removed when painful. Since we have changed the design of the screws, (6 mm of diameter) no one broke. Have we reach the goal? In this experience, the answer is yes [4]. Not any femoral plate was removed. All patients are either too old now or are in a very high place in the sky where nobody can reach them or are still living with their implants.
Conclusion
The lateral femoral implant is, according to this cohorte, one of the good solutions for a long implant’s life, as long as the patient’s life, whatever his age [5-7]. But we should stress the difficulty of its fixation on the upper femoral metaphysis. The greater trochanteric osteotomy must be perfect. The screws must be of a good size and length. The consolidation delay of this bone section must be respected. The patient must walk with two crutches during this time with only a contact support. Surgeon must keep in mind that he is not at all a simple machine to operate. He must practice with his heart and must explain to his patient what he will do and why he will do for it in order to reach the target [9]. In this way, the surgeon does not destroy the intra-medullary bone marrow. He keeps as much as possible the cervical cancellous bone (Figure a, b). The implant applies a constant pressure on the femoral calcar [8], and the periosteum osteogenic power covers by time the implant plate, connecting strongly mechanically both bone and metal. This patient is in good health, has a normal activity for her age. Both femoral implants remain stable and will stay so until the end of the story.
Acknowledgment
None.
Conflict of Interest
No conflict of Interest.
References
- Y Cirotteau (1999) Morphological changes of the superior femoral metaphysis in men with osteoporotic disease. C R Acad Sci III 322(5): 401-411.
- Y Cirotteau (1994) Morphological changes of the diaphysis of a long bone in adults. Theoretical therapeutic deductions. The Surgical Letter. SOFCOT special issue N°128.
- Y Cirotteau (1985) Total prostheses with external cortical support. Annals of the Academy of Surgery III: 817-823.
- Y Cirotteau (1996) Femoral implant fixed on the external cortex: Longterm results of hip osteoarthritis of the young subject. Eur J Orthop Surg Traumatol 6: 247-253.
- Y Cirotteau (1989) Reviews and results of the total prosthesis with femoral support on the external cortex. Surgery 115: 373-379.
- Yves Cirotteau (1989) The interest of a hip prosthesis has femoral support on the external cortex. Total hip prosthesis Patient information booklet Questions-Answers.
- Y Cirotteau (1988) Prosthesis with external femoral support. Surgery books N°67-3.
- J Dumbleton, JH Buschelow M, A Strain Gage Analysis of the Cirotteau Hip Prothesis. Dumbleton; How medica: Divisional Research and Development. Rutherford, USA.
- F Pelisse (1990) Notes on the conclusions of the study made by the Howmedica Society on the prosthesis of Dr Y. Cirotteau CIAV: The Charmilles Valenton, France.
-
Yves Cirotteau. EXTERNAL CORTICAL FEMORAL IMPLANT IN A T.H.P. A long term follow up of a Clinical Case. Curr Tr Clin & Med Sci. 1(2): 2019. CTCMS.MS.ID.000510.
-
Coxarthrosis, Bone metabolism, Femoral implant, Medullary canal, Arthroplasty failure, Prothesis, Mineralization, Vascularization, Bone remodeling
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






