 Case Report
Case Report
Invasive Mole with Nephrotic Syndrome: A Case Report with Literature Review
Wenyun Wang1, Yuanyuan Qi2, Zhifang Zhao3, Shijie Ma3, Rui Ruan3 and Yu Zhao3*
1Department of Pediatric Surgery, Second Hospital of Lanzhou University, Lanzhou, China
2Department of Nephrology, Second Hospital of Lanzhou University, Lanzhou, China
3Department of Medicine, Northwest Minzu University, Lanzhou, China
Yu Zhao, Department of Medicine, Northwest Minzu University, No.1, Northwest Village, Cheng Guan District Lanzhou, Gansu 730000, China.
Received Date: June 16, 2020; Published Date: July 08, 2020
Abstract
Nephrotic syndrome(NS)associated with invasive mole (IM) is uncommon. In this report, we present a case of NS that developed from IM. A 22-year-old woman was admitted to our hospital because of left lower slightly abdominal pain with sparing vaginal bleeding and NS. Transabdominal ultrasound examination confirmed a regular shape, border clearance component with a typical honeycomb pattern in the left side of the uterus. The curettage was performed for her two times. A renal biopsy was performed and suggested minimal change disease (MCD). Interestingly, when the IM was removed, her NS was complete remission. We report the rare case to highlight the importance of considering that NS associated with IM should be kept in mind during management of a woman of childbearing age with renal involvement.
Keywords: Invasive mole; Nephrotic syndrome; Gestational trophoblastic neoplasia; hydatidiform mole
Introduction
Invasive mole (IM), a malignant tumor, is a form of gestational trophoblastic neoplasia (GTN), which are characterized by invasive hydatid tissue into the myometrium or distant metastasis [1]. The most common transfer locations for IM are the vagina, lungs and brain. The most common symptom of IM is irregular vaginal bleeding, but further symptoms caused by bleeding in the metastases may also be detected, such as hemoptysis and neurological symptoms [2]. Myometrial invasion, swollen villi and hyperplastic trophoblast are often considered to be the pathological features of IM. IM′s clinical diagnosis mainly depends on medical history, clinical symptoms, laboratory tests and examination using imaging. Pathological results are the most essential basis for diagnosis. Good prognosis based on timely and comprehensive chemotherapy [3]. In this report, we describe a patient presenting with NS in which the underlying diagnosis of IM was made by a combination of chance and a high level of clinical suspicion, and to improve patient care amongst internists by heightening awareness of this uncommon condition.
Case Report
A 22-year-old woman was admitted to our hospital because of slight left lower abdominal pain with sporadic vaginal bleeding. She reported amenorrhea for 37 days and had a positive urine β-hCG test. She had no obstetric history, with menarche at 13 years of age, regular menstruation and no pregnancy history. She was admitted to the department of nephrology because of NS and was treated with hydrochlorothiazide, but her oedema was aggravated. Her urine output decreased to 500 ml/day. She had no fever, erythema, joint pain or alopecia. Physical examination at admission revealed mucocutaneous pallor and generalized oedema. A soft elastic, non-tender palpable mass, approximately 10 cm in diameter, was identified in the lower left part of the abdomen. A vaginal examination showed a normal vulva and vagina. Laboratory examination showed the following: haemoglobin 93 g/L, total protein 50 g/L, albumin 28 g/L, serum β-hCG 15400 mIU/mL, urine β-hCG 34140 mIU/mL, and urine protein 3.5 g/24 h. Screening tests for hepatitis A, B, and C were negative. Testing for antinuclear antibodies, dsDNA antibodies, anticardiolipin antibodies and antineutrophil cytoplasmic antibodies were negative. Due to increased abdominal pain and oedema in the patient, haemoglobin was decreased to 81 g/L. Ectopic pregnancy was highly suspected and she was urgently transferred to the gynaecology department. A trans-abdominal ultrasound examination confirmed a regularshaped, clear-border mass with a typical honeycomb pattern on the left side of the uterus. An abdominopelvic computed tomography scan confirmed a substantial mass; ovarian cystadenocarcinoma and trophoblastic neoplasia of the uterus were considered. Suction curettage was performed twice. Gross suction curettage specimens showed placental tissue with different-sized vesicles that resembled a cluster of grapes, with the absence of a foetus. A light micrograph showed complete hydatidiform mole (III), and hydatidiform mole with myometrial invasion was confirmed by ultrasonography. A renal biopsy was performed. Light microscopy showed that the glomeruli were normal, without mesangial widening. The capillary loops were open and had normal in appearance. Immunofluorescence staining revealed that immunoglobulin G (IgG), IgA, IgM, C3, fibrinogen and C1q were all negative. Electron microscopy revealed that the thickness of the basement membrane was within the normal range, and diffuse foot process fusion was observed. The pathological findings suggested minimal change disease (MCD). After suction curettage, facial oedema and pretibial pitting oedema significantly subsided. Her urine output increased to 1000 ml/day, and she lost weight. Her abdominal pain was obviously eased, and the vaginal bleeding was clearly lessened. Serum β-hCG levels declined to 2068 mIU/mL. Blood chemistry tests revealed a total protein level of 54.3 g/L and albumin level of 32.6 g/L. 5-FU single chamber chemotherapy was administered. One month later, her serum β-hCG declined to 7.7 mIU/mL, her urine β-hCG decreased to 5 mIU/mL, her total protein was 57.7 g/L, her albumin was 41.9 g/L, and her urine protein was 0.56 g/24 h. She has been regularly followed for the last twenty-six months and has remained free of clinical symptoms.
Discussion
Table 1: Summary of literature
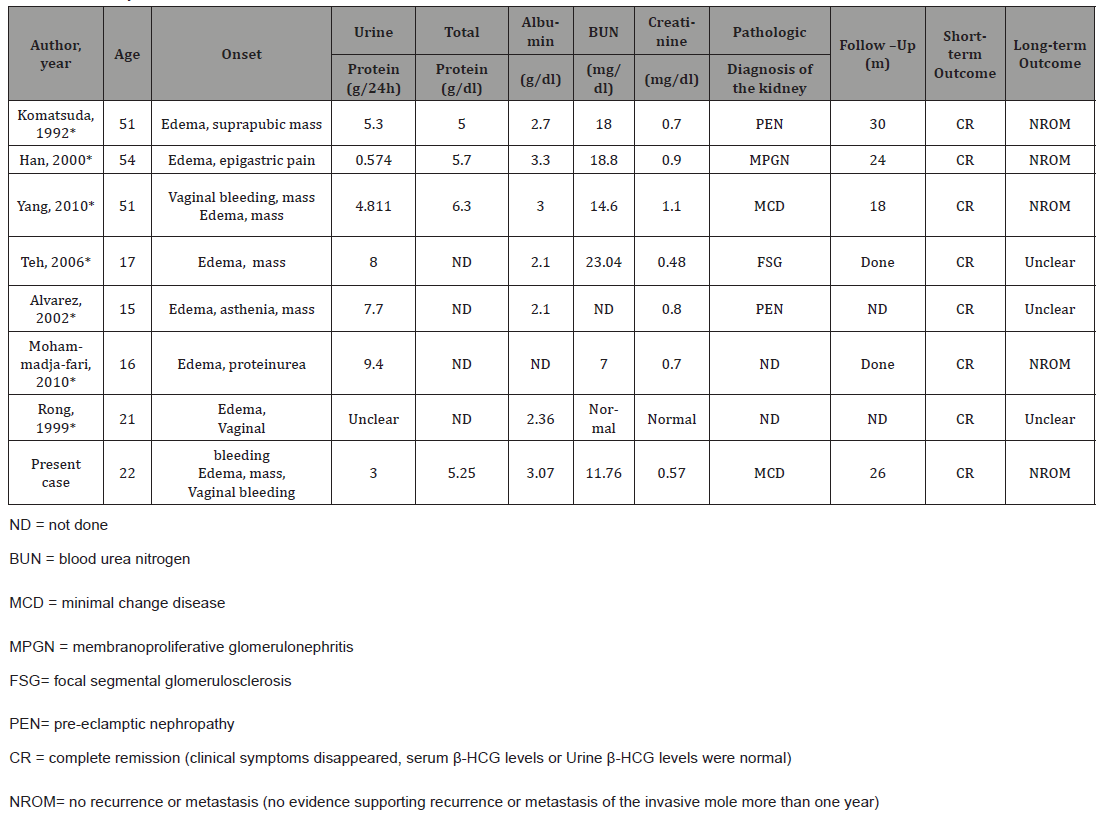
IM is responsible for the most cases of localized GTN1, which is one style of Gestational trophoblastic disease (GTD). IM occur in approximately 15% of patients with complete hydatidiform moles, while in other types of pregnancies it occurs less frequently [4]. In China, the incidence rate of IM following pregnancy is 0.94- 1.30% [5]. IM, sometimes, which are penetration of the peritoneum or adjacent parametria or the vaginal vault, are distinguished by excessive trophoblastic overgrowth and extensive penetration by trophoblastic elements, including whole villi, deep into the myometrium. As a result of the improved economy and the decline in overall birth rate, the prevalence of IM has declined over the past 30 years. However, IM has malignant tumor behavior and can undergo extensive metastasis. If not treated in time, it can be converted into choriocarcinoma with poor prognosis, which can lead to significant morbidity and mortality. The common causes of secondary adult female NS are systemic lupus erythematosus, hepatitis B, and Henoch-Schonlein purpura, etc. We report additionally the rare case about NS associated with IM in a 22-year-old unmarried woman. Myometrial invasion, swollen villi and hyperplastic trophoblasts are frequently considered to be pathological features of IM; however, the majority of IM cases are diagnosed clinically rather than pathologically [6]. Based on the clinical manifestation and correlation examination, we diagnosed NS associated with IM. From the treatment situation, with a nearly recover in laboratory test results after a week of the suction curettage. Our patient was consistent with the above references in clinical manifestation and prognosis. We thought the NS associated with IM, probably is the paraneoplastic phenomenon. Because when the suction curettage was administered, the NS secondary to the IM was general remission. It is not clear that the precise pathogenesis of relationship between the IM and NS. Rong YJ [7] showed that the pathogenesis may be due to maternal and trophoblast cells had abnormal immune response with immune complex deposition in glomeruli, causing increased permeability of the glomerular filtration membrane, which led to a series of pathophysiological changes. The placenta releases trophoblastic cells with cytotoxic characteristics and the capacity to cause secondary glomerular endothelial damage by Brown DW reported [8]. The NS associated with IM, probably is the paraneoplastic phenomenon. IM has malignant potential for local invasion and distant metastasis [8] and is probably capable of causing a paraneoplastic phenomenon, which is noted prior to the diagnosis of the malignancy. It is possible that the placenta releases trophoblastic cells with cytotoxic characteristics and the capacity to cause secondary glomerular endothelial damage. A review of the literature reveals that only 7 cases on NS accompanied by hydatidiform moles are shown in Table 1 [9-14].
Pathologic finding suggested respectively, pre-eclamptic nephropathy 9, 12, membrano proliferative glomerulonephritis10, focal segmental glomerulosclerosis [12] and MCD [13]. NS was the prominently manifestation, endothelial cell swelling or swollen epithelial cells with diffuse foot process fusion were the renal pathological presentation. Interestingly, when the IM was removed, the IM was complete remission. According the literatures, we did not find a tendency about pathology of NS associated with hydatidiform moles. Pathologic finding of our patient was MCD. We can actively infer that IM had a tendency to be associated with MCD. Recently, although MCD may occur in association with haematologic malignancies, lymphoma or leukaemias [15], rare cases of MCD associated with solid tumors have been reported. We report additionally the rare case to highlight the importance of considering that NS associated with GTD should be kept in mind during management of a woman of childbearing age with renal involvement, pregnancy history and menstrual history should be considered as an indispensable inquiry for the choice of correct treatment measures.
Funding
This study was supported by the Fundamental Research Funds for the central Universities [grant number 31920190106; 31920170042].
Acknowledgement
We thank Dr. Yuzhen Guo and Dr. Jing Wang for guiding the diagnosis and treatment of this case. We also thank to the participation of the patient being reported. Written informed consent has been obtained from the patient for publication of this case report and any accompanying images.
Conflict of Interest
The authors do not have any potential financial conflicts of interest to disclose.
References
- Seckl MJ, Sebire NJ, Berkowitz RS (2010) Gestational trophoblastic disease. Lancet 376: 717-729.
- Loukovaara M, Pukkala E, Lehtovirta P, Leminen A (2005) Epidemiology of hydatidiform mole in Finland, 1975 to 2001. Eur J Gynaecol Oncol 26(2): 207-208.
- Ngan H, Seckl MJ, Berkowitz RS, Yang X, Francois G, et al. (2018) Update on the diagnosis and management of gestational trophoblastic disease. Int J Gynaecol Obstet 2: 79-85.
- Shen Y, Wan X, Xie X (2017) A metastatic invasive mole arising from iatrogenic uterus perforation. BMC Cancer 17(1): 876.
- Shi YF, Li JQ, Zheng W, Chen XJ, Qiao YH, et al. (2005) Survey of gestational trophoblastic disease incidence among 3.6 million pregnancies in China. Zhonghua Fu Chan Ke Za Zhi 40(2): 76-78.
- Lurain JR (2010) Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol 203(6): 531-539.
- Rong YJ (1999) Nephrotic syndrome associated with hydatidiform mole: a case report. Journal of North Sichuan Medical College 1: 14.
- Brown DW (1999) Pre-eclampsia: a mistake of trophoblastic cells for tumour cells. Med Hypotheses 53(2): 124-126.
- Komatsuda A, Nakamoto Y, Asakura K, Yasuda T, Imai H, et al. (1992) Case report: nephrotic syndrome associated with a total hydatidiform mole. Am J Med Sci 303(5): 309-312.
- Han BG, Kim MH, Karl EH, Hong SW, Choi SO (2000) A case of membranoproliferative glomerulonephritis associated with a hydatidiform mole. Yonsei Med J 41(3): 407-410.
- Alvarez L, Ortega E, Rocamora N, Tromo A, Gil GM, et al. (2002) An unusual cause of nephrotic syndrome and hypertension in a young woman. Nephrol Dial Transplant 17(11): 2026-2029.
- Teh HS, Halim AG, Soehardy Z, Fauzi AR, Kong Norella CT (2006) Molar pregnancy and glomerulonephritis. Med J Malaysia 61(3): 361-362.
- Yang JW, Choi SO, Kim BR (2010) Nephrotic syndrome associated with invasive mole: a case report. Nephrol Dial Transplant 25: 2023-2026.
- Mohammadjafari R, Abedi P, Belady S (2010) A case of nephrotic syndrome associated with hydatiform mole. Rare Tumors 2: e61.
- Bacchetta J, Juillard L, Cochat P, Droz JP (2009) Paraneoplastic glomerular diseases and malignancies. Crit Rev Oncol Hematol 70(1): 39–58.
-
Shijie Ma, Rui Ruan, Yu Zhao. Invasive Mole with Nephrotic Syndrome: A Case Report with Literature Review. Annal Urol & Nephrol. 2(1): 2020. AUN.MS.ID.000529.
-
Acute kidney injury, Elderly, Diabetes mellitus, Hyperkalemia, High anion gap acidosis, Chronic kidney disease, Renin-angiotensin-aldosterone system inhibitors, Heart failure, Mineral corticoid receptor antagonists
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






