 Research Article
Research Article
Saphenous Nerve Block to the Adductor Canal and IPACK Block In Analgesic Management of Knee Replacements: Our Experience
Luca De Lipsis*
Anaesthesia Department, “Sacred Heart of Jesus” Hospital, Benevento, Italy
Luca De Lipsis, Anaesthesia Department, “Sacred Heart of Jesus” Hospital, Benevento, Italy.
Received Date: April 27, 2023; Published Date:May 24, 2023
Introduction
The implantation of a knee prosthesis is a very common operation but burdened by significant pain in the immediate operating place, after resolution of anesthesia [1]. Recent SAARTI guidelines suggest a reduction in the use of opioids, commonly used as first-line drugs in postoperative analgesia for interventions that cause intense pain, in order to reduce adverse effects [2-4]. Locoregional ultrasound-guided analgesia represents an alternative to the use of opioids and the new fascia blocks can represent a valid and safe method in the management of postoperative pain [5, 6]. The aim of our study was to improve analgesia during the postoperative period, using a double band block, saphenous nerve block to the adductor canal (ACB) and infiltration of local anesthetic in the interspace between the popliteal artery and the posterior capsule of the knee (IPACK block), testing in the postoperative NRS scale, the appearance of side effects, cumulative opioid use, physical recovery of patients and their degree of satisfaction.
Materials and Methods
At the Sacred Heart of Jesus Hospital, 30 patients undergoing knee replacement implantation were enrolled. The exclusion criteria were: patients with ASA III and IV classification, emergency interventions, revision of prostheses, implantation of uni compartmental prostheses. All patients received the following procedure:
a) Pregabalin 150 mg before surgery.
b) IPACK block: with the patient in the supine position and the leg slightly flexed on the thigh we positioned the linear transducer above the fold of the popliteal fossa until we visualized the tibial nerve, in the common peroneal nerve, the popliteal artery and the femoral condyles. From this position we slid the transducer proximately until we found the flat back of the femur shaft. At this point we inserted the 80 mm needle with technique in plane towards the space between the popliteal artery and the femur. Finally, after injecting 1-2ml of saline to open up the space we administered 20 ml of AL levobupivacaine 0.375% 20ml.
c) Single shot spinal anesthesia with 15 mg levobupivaciana 0.5 % 3ml.
d) Ultrasound-guided block of the saphenous nerve in the adductor canal (ACB): when the supine patient with the thigh slightly abducted we identified with the convex ultrasound probe the apex of the triangle of the Scarpa and then proceed medially along the entire adductor canal until the medial edge of the sartorius muscle meets the medial edge of the adductor muscle long. At this point we identified the femoral artery and infiltrated with 80 mm needle with in-plane technique first 1-2 ml of fuisiological solution, then 20 ml of AL levobupivacania 0.375%.
In the post-operative period we have included:
a. Paracetamol 1gr iv every 6 hours for 2 days.
b. Diclofenac 75mg 1 fl daily for 2 days.
If the NRS scale had a score greater than 3 we prescribed a bolus of morphine PCA (Patient Controlled Analgesia) as rescue analgesia.
I. The next day further ultrasound-guided blockade of the saphenous nerve to the adductor canal before physiotherapy.
II. Pain control was identified with the validated NRS scale administered at 4, 8, 12, 24, 36 and 48 hours after the end of surgery. Adverse events such as nausea, pruritus, respiratory depression, delirium and sleep deprivation were recorded.
Results
None of the patients experienced any side effects. Only three patients needed morphine PCA bolus because they had an NRS [7] greater than 3 within 20 hours of surgery. The rest of the patients had an NRS value of less than 3 in the following 48 hours. Motility was recovered after about 4 hours from spinal anesthesia. All patients began physiotherapy rehabilitation on the first post-operative day, after further ultrasound-guided blockade of the saphenous nerve to the adductor canal. There were no episodes of delirium or sleep deprivation. All patients were discharged on the fourth day with a high degree of satisfaction (Tables 1, 2). The analyzed sample consists of 30 patients whose pain levels were measured at time intervals of 6h-12h-24h-48h and divided into 3 pain scales 0-3, 4-7, 7-10. All the data are shown in the table.
Table 1:
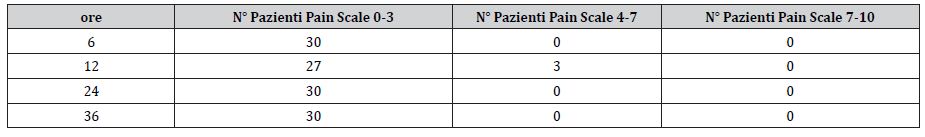
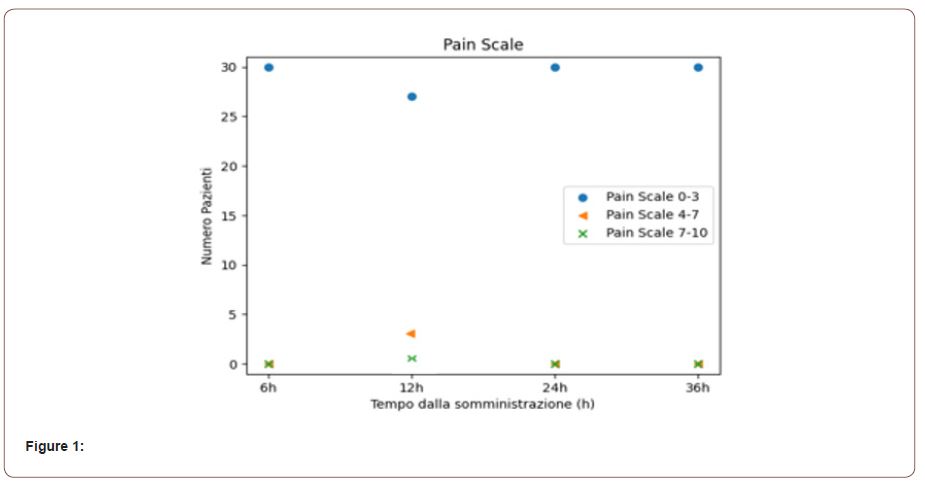
A first qualitative analysis shows that no patient fell into the Pain Scale 7-10 range, while only 3 patients passed from 0-3 to 4-7 at the 12th hour. Therefore, there is an increase in perceived pain in 10% of patients. Below are the Scatter Plots of the patient population by pain band as a function of time.
Table 2:
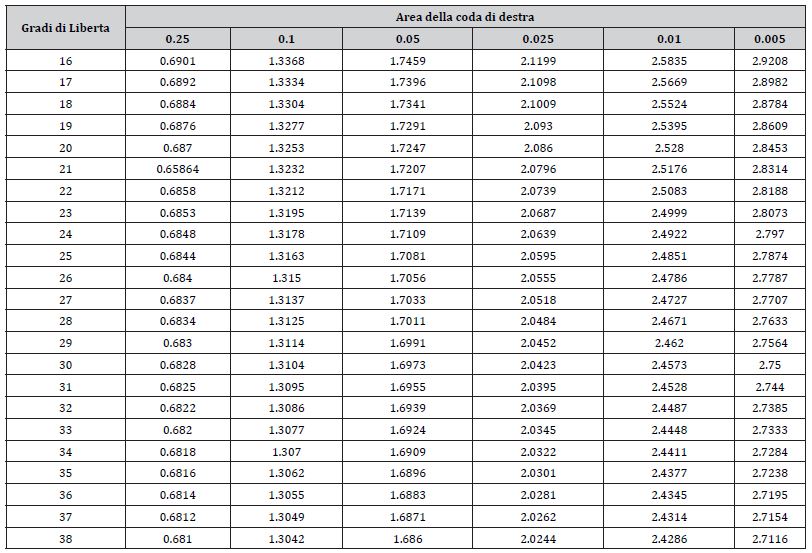
The value at 29 degrees of freedom and significance level 0.05 is equal to 1.6991.
Note that the empirical t value is 1.1967, which differs from the reference value only by 0.5024.
The null hypothesis, i.e. that the fluctuation of 10% is purely random and therefore compatible with the ideal case of 3%, cannot be rejected strictly at the chosen level of significance because the observed “t” is significantly lower than expected (in the table). However, it should be emphasized that we are facing a borderline case in which we can consider the hypothesis that the fluctuations are random plausible, but this likelihood is based on a small sample on which the test is as soon as possible, it would therefore be good to increase the sample population or carry out more tests to obtain a more nourished and clarifying statistic.
However, it should also be emphasized that the hypothesis tested is stringent, in fact as an expected value for the average of patients with pain was chosen the value corresponding to 3% of patients in the pain band 4-7 at 12h. In fact, if we admit that the treatment is successful for 29 patients out of 30 (3%) we would get a t equal to 1.1567 then the observed value would be fairly lower (of 0.5024) than the rejection threshold (1.6991), leading us to conclude that the discrepancy between observation and the ideal case that only one patient out of 30 shows pain would be very insignificant, and that the observed scenario is compatible with the ideal one. In light of these considerations, we can conclude that the treatment proves to be statistically compatible even with broadly optimistic ideal scenarios, but that it requires a strengthening of the sample population. We conclude that the test, compared to the ideal hypothesis, gave a positive result with P -value = 0.0352. (Medium-high statistical significance).
Statistical analysis
The analyzed sample consists of 30 patients whose pain levels were measured at time intervals of 6h-12h-24h-48h and divided into 3 pain scales 0-3, 4-7, 7-10. All the data are shown in the table.
A first qualitative analysis shows that no patient fell into the Pain Scale 7-10 range, while only 3 patients passed from 0-3 to 4-7 at the 12th hour. Therefore, there is an increase in perceived pain in 10% of patients. Below are the Scatter Plots of the patient population by pain band as a function of time.
The population of the sample analyzed is just enough to proceed with a hypothesis test that uses as a test statistic the random variable the “Student’s t”

Where we denote with the μ expected value of the sample mean and with the X sample mean, N is the population and is the σ variance estimator
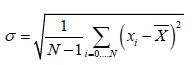
We will conduct a hypothesis test with a level of significance α=0,05. The null hypothesis of our test will be that the average of the observed pain values is that corresponding to having only one patient out of 30 with peak pain at 12h. We focus on the scenario detected 12h after administration because all other cases are evidently already compatible with this hypothesis. We therefore want to analyze the population at 12h and see if the 10% fluctuation recorded can be attributed to chance. We will exploit the invariance by rescaling of the variable “t”. We will compare the real situation with the ideal situation in which only one patient in 30 (3%) shows the ascent of pain in the range 4-7 to 12h and determine if the average of the values of the real case differs significantly from the ideal case mentioned above, in which μ=1/30. Attributing value 1 to the presence of pain and zero value to absence for patients in the range 4-7 to 12 h, registers
From which it can be deduced that the value of the test statistic is equal to:

We compare this value with the reference table for the chosen hypothesis test
(Table 2)
The value at 29 degrees of freedom and significance level 0.05 is equal to 1.6991.
Note that the empirical t value is 1.1967, which differs from the reference value only by 0.5024.
The null hypothesis, i.e. that the fluctuation of 10% is purely random and therefore compatible with the ideal case of 3%, cannot be rejected strictly at the chosen level of significance because the observed “t” is significantly lower than expected (in the table). However, it should be emphasized that we are facing a borderline case in which we can consider the hypothesis that the fluctuations are random plausible, but this likelihood is based on a small sample on which the test is as soon as possible, it would therefore be good to increase the sample population or carry out more tests to obtain a more nourished and clarifying statistic.
However, it should also be emphasized that the hypothesis tested is stringent, in fact as an expected value for the average of patients with pain was chosen the value corresponding to 3% of patients in the pain band 4-7 at 12h. In fact, if we admit that the treatment is successful for 29 patients out of 30 (3%) we would get a t equal to 1.1567 then the observed value would be fairly lower (of 0.5024) than the rejection threshold (1.6991), leading us to conclude that the discrepancy between observation and the ideal case that only one patient out of 30 shows pain would be very insignificant, and that the observed scenario is compatible with the ideal one. In light of these considerations, we can conclude that the treatment proves to be statistically compatible even with broadly optimistic ideal scenarios, but that it requires a strengthening of the sample population. We conclude that the test, compared to the ideal hypothesis, gave a positive result with P -value = 0.0352. (Medium-high statistical significance).
Considerations
There is currently a huge debate regarding which analgesic management should be preferred in knee prosthetic surgery. Multimodal pain management strategies have evolved to improve patient satisfaction, early mobilization of the prosthetic limb, and reduce side effects of opioids, commonly used as first-line drugs in the management of intense pain [8]. Addressing postoperative pain with a multimodal approach is essential for proper pain control and early discharge of patients. A typical regimen involves the use of drugs with different mechanisms of action such as paracetamol, nonsteroidal anti-inflammatory drugs and premedication gabapentinoid drugs, the latter used to attenuate the inflammatory cascade in response to surgery and decrease pain due to neuronal hyperexcitability. The blockade of the posterior compartment of the knee capsule (IPACK, Infiltration between the Popliteal Artery and Capsule of the Knee) is an exclusively analgesic block performed with the local administration of anesthetic close to the capsule itself, below the popliteal vessels [9]. By depositing with ultrasound a fair volume of anesthetic (20 ml) it is possible to affect the terminal sensory branches of the sciatic nerve that reach this compartment and that guarantee analgesic coverage of the posterior portion of the knee. Furthermore, blocking only the terminal branches significantly reduces the incidence of foot drop, i.e., the motor block of the muscles used for foot flexion [10, 11]. Adductor canal blockade (ACB) is currently considered the best choice in a context of active mobilization and early rehabilitation, since it has been shown to guarantee analgesic efficacy similar to femoral nerve block, while maintaining quadriceps muscle strength. In conclusion, saphenous nerve blockade to the adductor canal in association with IPACK block, NSAIDs, paracetamol and gabapentinoids as a form of multimodal analgesia, have shown greater efficacy in the management of post-operative pain of uni compartmental knee replacements, favoring early mobilization and reduced opioid consumption.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Gorguner M, Akgun M (2010) Acute inhalation injury. Eurasian J Med 42(1): 28-35.
- Keith A Lafferty KA, Bonhomme K, Martinez CV, Wiener SW, Serebrisky D, et al. (2018) Smoke Inhalation Injury.
- Neghab M, Choobineh A (2007) Work-related respiratory symptoms and ventilatory disorders among employees of a cement industry in Shiraz, Iran. J Occup Health 49: 273-278.
- Nordby KC (2011) Exposure to thoracic dust, airway symptoms and lung function in cement production workers. Eur Respir J 38(6): 1278-1286.
- Karkhanis V, Joshi JM (2011) Cement dust exposure-related emphysema in a construction worker. Lung India 28(4): 294-296.
- Alper HE, Yu S, Stellman SD, Brackbill RM (2017) Injury, intense dust exposure, and chronic disease among survivors of the World Trade Center terrorist attacks of September 11, 2001. Inj Epidemiol 4(1): 17.
- Barron Andrew R (2010) Chemical Composition of Portland Cement. OpenStax-CNX module: m16445.
- Gilomen S, Brack T, Klinik M, Glarus K (2012) Cement accident with severe consequences. Swiss Medical Foru 12(26): 539-541.
- Brun P, Kunz A, Funke M (2013) Buried under gypsum powder-A rare respiratory complication. Respir Med Case Rep 8: 36-39.
- Morin AM, Zahringer J, Kasper M, von Schmadel E, Suhayda A (1997) Acute respiratory insufficiency after inhaling concrete dust--a case report. Anasthesiol Intensivmed Notfallmed Schmerzther 32(1): 56-60.
- Albright JM, Davis CS, Bird MD, Ramirez L, Kim H, et al. (2012) The acute pulmonary inflammatory response to the graded severity of smoke inhalation injury. Crit Care Med 40(4): 1113-1121.
- Glazer CS (2003) Acute Inhalational Injury. In: Hanley ME, Welsh CH (eds.) Current Diagnosis & Treatment in Pulmonary Medicine. International (Edn.), New York: Mc-Graw Hill, Pp: 354-360.
- (1999) Hazard Prevention and Control in the Work Environment: Airborne Dust (WHO, 1999) WHO/SDE/OEH/99.14.
- Heyder J, Gebhart J, Rudolf G, Schiller CF, Stahlhofen W (1986) Deposition of particles in the human respiratory tract in the size range 0.005-155. Journal of Aerosol Science 17: 811-825.
- (2006) Portland Cement Dust- Hazard assessment document. UK Health and Safety Executive (HSE).
- Coumes CCD, Courtois S, Nectoux D, Leclercq S, Bourbon X (2006) Formulating a low-alkalinity, high-resistance and low-heat concrete for radioactive waste repositories. Cement and Concrete Research 36(12): 2152-2163.
- Catalano F, Mariano F, Maina G, Bianco C, Nuzzo J, et al. (2013) An unusual case of extensive self-inflicted cement burn. Ann Burns Fire Disasters 26(1): 40-43.
- Peters WJ (1984) Alkali burns from wet cement. Can Med Assoc J 130(7): 902-904.
- Gregoretti C, Decaroli D, Stella M, Mistretta A, et al. (2007) Management of Blast and Inhalation Injury. Breathe 3(4): 364-373.
- Hassan Z, Wong JK, Bush J, Bayat A, Dunn KW (2010) Assessing the severity of inhalation injuries in adults. Burns 36(2): 212-216.
- Meduri GU, Bridges L, Shih MC, Marik PE, Siemieniuk RAC, Kocak M (2016) Prolonged glucocorticoid treatment is associated with improved ARDS outcomes: analysis of individual patients' data from four randomized trials and trial-level meta-analysis of the updated literature. Intensive Care Med 42(5): 829-840.
-
Luca De Lipsis*. Saphenous Nerve Block to the Adductor Canal and IPACK Block In Analgesic Management of Knee Replacements: Our Experience. Anaest & Sur Open Access J. 4(2): 2023. ASOAJ.MS.ID.000581.
-
Knee prosthesis, Anesthesia, Physical recovery, Saphenous nerve, Patient Controlled Analgesia (PCA), Physiotherapy, Respiratory depression, Sleep deprivation, Adductor Canal Blockade (ACB)
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






