 Research Article
Research Article
Non-Sterile Clinical GALENIC LABORATORY: A Scientific Discipline Between Laboratory Practice Clinical Pharmacy and Personalized Pharmacological Therapy
Luisetto M1*, Khaled Edbey2, Fiazza C3, Mashori Gulam Rasool4, Nili B Ahmadabadi5, Cabianca L6 and Oleg Yurevich7
1IMA MARIJNSKAYA academy, applied pharmacologist, hospital pharmacist manager, member of ITALIAN GALENIST UNION, Galenic laboratory PC AREA, Italy
2Professor of physical chemistry, Libyan Authority for Scientific Research
3Independent researcher, hospital pharmacist manager PC AREA
4Professor, Department of Medical & Health Sciences for Woman, Peoples University of Medical and Health Sciences for Women, Pakistan
5Medicinal chemist, Nano Drug Delivery, (a Product Development Firm), United States
6Bio-medical laboratory turin Italy Citta’ della Salute
7Latyshew IMA president RU
Luisetto Mauro, IMA MARIJNSKAYA academy, applied pharmacologist, hospital pharmacist manager, member of ITALIAN GALENIST UNION, Galenic laboratory PC AREA, Italy.
Received Date:February 05, 2024; Published Date:February 14, 2024
Abstract
Observing the today hospital practice in many countries and the international literature involved it is clear How clinical pharmacy is linked to galenic laboratory practice. Today is more than recent past due to the various kind of magistral formula request by the clinicians. It is necessary that the clinical pharmacist perspective must be added to the classic GALENIC laboratory competencies: this makes possible to complete the profile of efficacy and safety of this fundamental Drugs. The clinical galenic activity is divided into sterile and Nonsterile. (Total parenteral nutrition bags, Pain therapy, oncological parenteral drugs laboratory, radio drugs and diagnostics, non-sterile galenics). The aim of this work is to deeply investigate this crucial link (CLINICAL PHARMACY with LABORATORY PRACTICE) in order to get the really best clinical results for the patients. Clinical pharmacy principle, PHARMACEUTICAL care, managerial competencies and personalized pharmacy added to the best knowledge and competencies in galenic laboratory make the difference in order to obtain the right final clinical results.
The same in this work are submitted to international pharmacy practioner, directors and researchers the Normatives rules operating in an advanced country: the simplified NBP, an example that can be applied also in non-advanced nations. In Italy pharmacist can follow or the full NBP of the official pharmacopeia or the simplified according to DM Salute 18.11.2003. (related the kind of galenic formula if sterile or not) The NBP (good manufacturing rules) introduces a QUALITY SYSTEM MANAGEMENT. The full NBP are more used in more complex laboratory in example involved in specialistic products Like oncologic or radiopharmaceutical and others. The aim of these rules is to guarantee quality, security and efficacy of a drug prepared in galenic lab. This is based on responsibility principles, plan, documentation of all activity. (QUALITY SYSTEM OF INSURANCE) All phases of the preparation are the responsibility of the pharmacist. The final quality depends on the correct use of API and excipients, right calculations operation, right volume or weight operation, procedure following.
Keywords:Galenic Laboratory; Magistral Formula; Clinical Pharmacy; Pharmaceutical Care; Personalized Pharmacy; Medicine Shortage; NBP; Simplified Rules; Official Pharmacopeia; Control Process; Quality Management System; Rare Disease; 3d PRINTING Systems
Check on the final products:Following the procedure, aspects, packaging, and its closure. According to NBP the laboratory must be separated (or it must be separable) from the pharmacy and a second pharmacist (that is different from the pharmacist that prepares) must check the final preparation. The locals must be according to strictly environmental condition to make possible to prepare in safety way the drugs. And it is mandatory must to follow written procedure. (Instruments verify, training of the pharmacist cleaning procedure, significations). Raw material certifications, technical sheet, safety sheet. Working sheet is mandatory. The pharmacist can follow these two options related the kind of drugs produced and the characteristic of the laboratory. It is not the main focus of this work to produce a literal translation of DM 18/11/03 only to submit its general meanings. This can be considered for the authors useful to be added also to the normative rules in force in non-advanced countries.
Introduction
Starting from the consideration that in history of the remedy for the pathology of human’s great contribution was obtained with the introduction of GALENIC principle and methods. From GALENUS form Pergamon (Greek) 129 dc-201 comes the term GALENIC art of the pharmacist to produce drugs inside in the pharmacy. He codified the preparation of drugs using multiple kinds of ingredients. (active principle added with excipients). For many centuries these methods were used in the laboratory to produce remedy to treat many human pathologies. Federico II Svevia 1194 – 1250 knowed as “STUPOR MUNDI “related his open mind concepts introduced In Europe and in Italy the need to have specific rules for regulation the activity of drugs production in the pharmacy laboratory from the prescription activity of the physicians. This in order to avoid conflict of interest between this prescriptive function form the pharmacy practice: this produced the mandatory separation between medicine and pharmacy: to the physicians the role in therapy and for pharmacist the production and sell of the drugs. But during the illuministic period, the industrial revolution, the success of medicinal chemistry since 1800 and 1900 many forces make possible to shift the drugs production form the pharmacy to the more complex industry. During all this periods many FORMULARIES and then PHARMACOPOEIA in various countries was introduced and adopted to make possible to get adequate quality of the drugs produced, safety and reproducibility of the procedure. (monography, methods of analysis, table et other) This text becomes mandatory by healthcare law in the various contests (FU Italian, FU European, US pharmacopeia and many other examples). Also, the competencies of who were involved in remedy preparation increased over centuries: from botanic expertise (SCUOLA SALERNITANA VII e VIII century) to the IATROCHEMISTRY principle (PARACELSUS from XVI century). Before the pharmacists, apothecaries that worked alongside priests and physicians in regard to the patient care. The history of pharmaceutical history is well known from introduction of the first SULFAMIDICS since the Actual the last antivirals (for covid-19 treatment). But related the last industrial pharmaceutical revolution, some problem arosed: not all pharmaceuticals’ industries produce drugs for all subpopulation (pediatric patients, swallowing problems in geriatrics). There is the needs of personalized dosages or personalized pharmaceutical form (for pediatric or geriatric patients) needs to introduce drugs in enteral nutrition, drugs not available form national or foreign producers (national or international shortcomings), orphan drugs for some rare disease, dermatologic products, cannabis preparate, some disinfectants band antiseptics formula, some antidotes (galenics), some laboratory reagents and solutions, some contrast agents, odontoiatric galenics and many other So due to this failure of industry to cover all this situation the galenic laboratory is a real opportunity.
Today also many pharmaceutical industries not like more to produce classic drugs as many cardioactive products and other and the magistral product make possible to overcome this problem. (especially today whit actual economic crisis). Also, a great number of galenic formulas are in use commonly in the hospital: corrosive products for dermatologist, alcohol solution for laboratory, various reactive, phytotherapy derivates and so on. Galenic Pharmacy also provides educational, scientific and research activities in the profile discipline-pharmaceutical technology to the pharmacy student or under specialization programs. But observing international literature it is possible to see that the best clinical results are obtained when the laboratory activity in production magistral formula by the physicians is completed when available the clinical pharmacist and managerial competencies in the same team. Galenics is the laboratory process that turns an active ingredient (API) into a ready-to-use medicine that can be dosed as required for various patients. This optimizes their absorption. It is the discipline (or science) of dosage form design.
According Review
Braz. J. Pharm. Sci. 56 2020 https://doi.org/10.1590/s2175-
97902019000418358
Preparation of extemporaneous oral liquid in the hospital
pharmacy
Márcio Robert Mattos da Silva Letícia Pereira Dysars Elisabete
Pereira dos Santos Eduardo Ricci Júnior
“At the hospital, the pharmacist is constantly challenged to prepare extemporaneous solutions ES from tablets, capsules or drug powder for patients unable to swallow, such as pediatric, elderly and patients that use nasoenteric and nasogastric tubes. The preparation of extemporaneous solutions ES from capsules, tablets and drug powder requires stability studies analysis” (Figures 1,2).
Material And Methods
With and observational point of view an review of relevant article related the topics of this work is performed. It is produced the meaning translation of an Italian normative rule DM 18 NOV 2003. An practical experimental study is reported with results from 2008 to 2023 . Finally a global conclusioni is submitted to the researcher related also innovations in fields of Galenic laboratory.
From Literature
J Pharm Pract. 2021 Jun 15;8971900211023643. doi: 10.1177/08971900211023643.


Hospital Pharmacy Response to Covid-19 Pandemic in Italy: What We Learned from the First Outbreak Wave Vera Damuzzo, Riccardo Bertin, Daniele Mengato, Marco Chiumente, Melania Rivano, Angelo Claudio Palozzo DOI: 10.1177/08971900211023643 “When COVID-19 pandemic started, Italian hospital pharmacists faced multiple challenges and change their work practices.
The aim of this study was to describe the impact of the COVID-19 emergency on pharmaceutical care (PC) provided by pharmacists during the first wave of the pandemic. Issues related to pharmacist’s involvement in the pandemic management were changes in activities, support received by authorities and pharmacists’ own perceived role in the Health System HS. A crosssectional study based on a web survey was conducted between May and June 2020 collecting information from pharmacists, members of Italian Society of Clinical Pharmacy and Therapeutics SCPT. 113 (11.4%) completed the questionnaire. The cohort was divided into 2 arms: pharmacists who worked in severely COVID-19 affected areas (High Spread Regions) and those employed in the less affected areas (Low Spread Regions).
The changes in the pharmacy work settings reflected the
increase of logistics area and non-sterile clinical galenic, and
reduction of clinical tasks. The most demanding challenge was
referred to shortages of medical devices and drugs, 61/113
pharmacists reported difficulty in obtaining products compliant
to quality standards. National Institutions and the Regional
Governments provided a greater perceived support. More than
50% of participants felt that their role did not change if compared
to other healthcare professionals. Despite some limitations related
to their clinical activity, pharmacists played a crucial role in
supplying personal protective equipment, medical devices MD and
medications to improve health outcomes during this emergency.
The results may guide pharmacists in future actions to improve the
management of the pandemic [6].
Croat Med J. 2014 Dec; doi: 10.3325/cmj.2014.55.662
Establishment of galenic laboratories in developing countries to produce high quality medicines: results of Aid Progress Pharmacist Agreement (A.P.P.A.®) Project
Francesca Baratta, Antonio Germano, Gaetano Di Lascio, Richard Petieau, and Paola Brusa
Aid Progress Pharmacist Agreement Project: aims in developing countries
Aid Progress Pharmacist Agreement (A.P.P.A.®) is a non-profit association based on voluntary work and its main activity is the A.P.P.A.® Project. The Project started in the 2005 as a result of the cooperation between the Pharmacy Faculty of Turin (TO) and Italian community pharmacists. Its main task is the establishment of galenic laboratories (GLs) in hospitals of developing countries (DCs) according to the principles of international health cooperation.
Aims of the Project:
• establishing GLs in DCs with the aim of preparing
medicinal products MP that comply with quality requirements,
first of all to fight the widespread counterfeiting of medicines in
DCs.
• -tailoring the dosages and pharmaceutical forms PF
according to the actual patient needs.
• -employing local staff, teaching them a “new job,” and
opening a suitable school.
• -minimizing costs necessary to prepare these medicines.
There are relevant and important reasons why galenics should
be used:
i) low cost of the production system and simple operative
procedures.
ii) the possibility to adapt dosages and pharmaceutical forms
PF to the patients’ needs and medical prescriptions.
iii) reduction in the use of counterfeit medicines CM in the
settings where the GL is located [7].
Study protocol 08 January 2018
Impact of collaborative pharmaceutical care on in-patients’ medication safety: study protocol for a stepped wedge cluster randomized trial (MEDREV study) Géraldine Leguelinel-Blache, Christel Castelli, Clarisse Roux-Marson, Sophie Bouvet, Sandrine Andrieu, Philippe Cestac, Rémy Collomp, Paul Landais, Bertrice Loulière, Christelle Mouchoux, Rémi Varin, Benoit Allenet, MEDREV Working Group, Pierrick Bedouch & Jean-Marie Kinowski
“The clinical pharmacist CP will have a collaborative meeting
with both the prescriber and the nurse in order to notify any
possible medication errors and suggest any proposals to optimize
the AMO according to the medical history, the clinical status, and the
therapeutic adherence. (change of galenic form due to swallowing
problem, dose adjustment to renal function). After the collaborative
meeting, the clinical pharmacist will check whether the prescriber
has accepted his/her suggestion(s) and modified the AMO. All
the pharmaceutical interventions, the medication errors detected
and the pharmaceutical suggestions of order modification, will be
collected and characterized in a standardized form according to the
French Society of Clinical Pharmacy FSCP” [8].
JDDG: Journal der Deutschen Dermatologischen Gesellschaft
Topical preparations and their use in dermatology
Johannes Wohlrab 23 November 2016 https://doi.
org/10.1111/ddg.13151
“The choice of a pharmaceutical (galenic) concept is primarily
based on the requirements of the physico-chemical properties of
the active ingredient to be applied. The fixed combination of active
pharmaceutical ingredients API in topical preparations is suitable
for only a limited number of clinical treatment scenarios” [9].
Hospital Pharmacology. 2015.
Information on the Quality of Substance for the Preparation of
Pharmaceutical Drugs in Terms of
Hospital Pharmacy Marija Dj. Jovović, Maja M. Ribar
“Compliance with national legislation, like as establishing compliance prescribed by the European legislation in the field of drug development is binding. All manufacturers of drugs and/or active pharmaceutical ingredients must apply quality standards prescribed by the European Pharmacopoeia EP in order to develop, manufacture and sales of medicines. When it comes to the quality of pharmaceutical ingredients PI for the production of drugs in the pharmacy, pharmacies especially in residential institutions in our country is permanently done by harmonizing national legislation NL in order to improve conditions for the preparation and production of galenic drugs GD in terms of inpatient health institutions performed in a manner that is prescribed by international regulations. Th is requiring the adaptation of institutions, including fundamental changes in competence as national professional and administrative and regulatory rules that apply to state- and private sectors “(10)
Original Article
DOI: 10.1016/j.rppede.2016.02.012
Magistral drugs in hospitalized newborns and children
Medicamentos magistrais em recém-nascidos e crianças hospitalizados
Agueda Cabral de Souza Pereira, Elaine Silva Miranda, Selma Rodrigues de Castilho, Débora Omena Futuro, Lenise Arneiro Teixeira, Geraldo Renato de Paula
Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil
“The constant consumption of magistral oral solutions MOS and suspensions by newborns and children of the assessed hospital indicates the need for such preparations as a pediatric therapeutic alternative in this hospital.” (11)
Dooms, M., Carvalho, M. Compounded medication for patients with rare diseases. Orphanet J Rare Dis 13, 1 (2018). https://doi. org/10.1186/s13023-017-0741-y
04 January 2018 “When there is no on-label or even no offlabel treatment for patients with rare diseases pharmacists have to compound the medication” [12].
Pharmaceutics. 2021 Apr.
2021 Mar 26. doi: 10.3390/pharmaceutics13040448
Medicine Shortages in Serbia: Pharmacists’ Standpoint and Potential Solutions for a Non-EU Country
Nataša Jovanović Lješković, Aleksandra Jovanović Galović, Svetlana Stojkov, Nikola Jojić, and Slobodan Gigov
Umberto Musazzi. “Backup manufacturing on a small scale (magistral and galenical) could be a good way to overcome some kind of shortages” [13].
Pharmaceuticals (Basel). 2022 Jan
Mini-Tablets: A Valid Strategy to Combine Efficacy and Safety in Pediatrics
Guendalina Zuccari, Silvana Alfei, Danilo Marimpietri, Valentina
Iurilli, Paola Barabino, Leonardo Marchitto
DOI: 10.3390/ph15010108
“In the treatment of pediatric diseases, mass-produced dosage
forms are often not suitable for children. Commercially available
medicines CAM are commonly manipulated and mixed with food by
caregivers at home, or extemporaneous medications are routinely
compounded in the hospital pharmacies to treat hospitalized
children. Despite considerable efforts by regulatory agencies
RA, the pediatric population is still exposed to questionable and
potentially harmful practices. When designing medicines for
children, the ability to fine-tune the dosage while ensuring the
safety of the ingredients is of paramount importance. For these
purposes solid formulations may represent a valid alternative to
liquid formulations for their simpler formula and more stability,
and, to overcome the problem of swelling ability, mini tablets
could be a practicable option. This review work deals with the
different approaches that may be applied to develop mini tablets
intended for pediatrics with a focus on the safety of excipients.
Alongside the conventional method of compression, 3D printing
appeared particularly appealing, as it allows to reduce the number
of ingredients and to avoid both the mixing of powders and
intermediate steps such as granulation. this technique could be well
adaptable to the daily galenic preparations of a hospital pharmacy
HP, thus leading to a reduction of the common practice of off-label
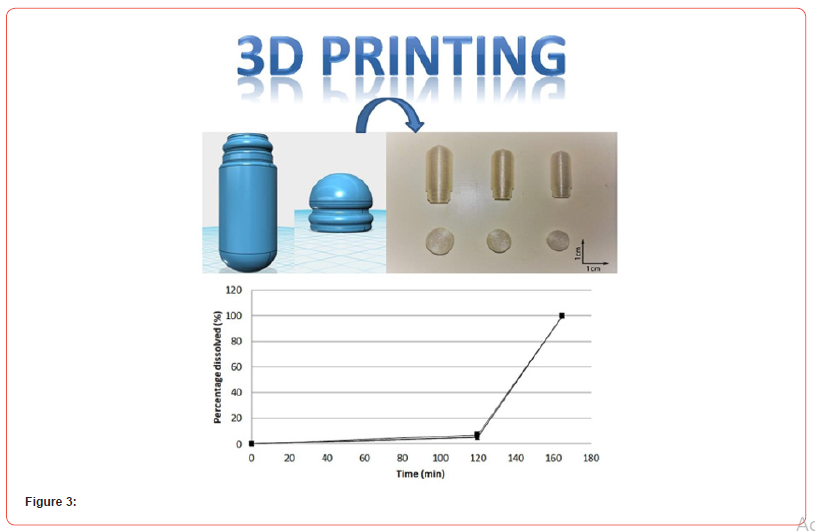
preparations” [14].
Volume 174, July 2021
Advanced Drug Delivery Reviews
Translating 3D printed pharmaceuticals: From hype to realworld
clinical applications
Seoane-Viaño, Sarah J. Trenfield , Abdul W. Basit , Alvaro
Goyanes
https://doi.org/10.1016/j.addr.2021.05.003
“Three-dimensional (3D) printing offers the potential to
revolutionize the production of pharmaceuticals targeted to
the gastrointestinal tract by offering a flexible drug product
manufacturing platform that can adapt readily to changing
market and patient needs. By using digital computer-aided design
software to produce medicines in a layer-by-layer manner, 3D
printing enables the on-demand production of drug products DP
with personalized dosages, drug combinations, geometries and
release characteristics; a concept which is currently unattainable
and cost inefficient with conventional manufacturing technologies
(tableting and encapsulation). This technology has been forecast
to disrupt a wide range of pharmaceutical applications, ranging
from expediting the drug development process DDP and providing
benefits for pharmaceutical manufacture, to on demand printing
of personalized medicines on the front-line and in hard-to-reach
areas” [15].
International Journal of Pharmaceutics
Volume 569, 5 October 2019
Feasibility study into the potential use of fused-deposition
modeling to manufacture 3D-printed enteric capsules in
compounding pharmacies Author links open overlay panel
Christoph Nober a, Giuseppe Manini a, Emeric Carlier a, Jean-Marie
Raquez b, Samira Benali b, Philippe Dubois b, Karim Amighi a,
Jonathan Goole a c
https://doi.org/10.1016/j.ijpharm.2019.118581
“The purpose of this research work was to investigate the feasibility of manufacturing enteric capsules, which could be used in compounding pharmacies, by fused-deposition modeling. It is well-known that conventional enteric dip coating of capsules in community pharmacies CP or hospitals is a time-consuming process which is characterized by erratic efficacy. Fused-deposition modeling was selected as a potential 3D printing method due to its ease and low-cost implementation LCI. Before starting to print the capsules, an effective sealing system was designed via a computeraided design program. Hot melt extrusion was used to make printable enteric filaments. They were made of the enteric polymer, a plasticizer and a thermoplastic polymer, namely Eudragit® L100- 55, polyethylene glycol 400 and polylactic acid, respectively.
Riboflavine-5′-phosphate was selected as a colored drug model to compare the efficacy of the 3D printed capsules to that of enteric dip coated capsules as they are currently produced in community pharmacies and hospitals HP. Different parameters of fabrication which could influence the dissolution profile of the model drug, such as the layer thickness or post-processing step, were studied. It was demonstrated that our 3D printed enteric capsules did not release the drug for 2 h in acid medium (pH 1.2). They completely dissolved within 45 min at pH 6.8 which allowed the release of a minimal amount of 85% w/w of drug as it was recommended by the European Pharmacopoeia EP 9th Edition for enteric products” [16] (Figure 3).
Practical project
In this part are analyzed the Italian normative rules named
NBP and simplified as DM Salute 18.11.2003 normed di buona
preparazione” applied by law as mandatory in the galenic
laboratory setting inside the pharmacy (public or private – hospital
and community).
NBP or GMP good manufacturing practice
The GMP philosophy are based on:
documentation of the process, registrations, every phase of the
process, activity and single operations.
- team must receive adeguate training
-responsibility clearly identified
-Quality of API and excipients
- cleaning and sanitization procedure
-Regular check of the instruments
- process validation
- NC nonconformity management
So, in Italy by law the pharmacist that work in a galenic laboratory according to DM 22/06/05 must follow or the FULL NBP of ITALIAN FU (more complex) or DM Salute 18.11.2003 (if not sterile magistral preparations or officinal reduced scale) Pharmacy that prepares nonsterile magistral formula or officinal reduced scale can follow or full NBP or simplified NBP. Instead, if prepared sterile products, or toxic preparate, anticancer drugs and radio drugs, it must be used biological hood: it is mandatory to follow full NBP. For non-sterile products it is possible in Italy to deviate from full NBP and to follow the simplified rules if it is possible to keep under control all the process, proving it. (quality efficacy, safety depends on organization and consistent control). First NBP was introduced in (FU IX ed.) in 1989. In the chapter 795 USP, pharmaceutical compounding of non-sterile products, related the difficulty of the preparations, its stability, storage conditions, dosage form, complexity in calculations, systemic, topic use, risk level for pharmacist, damage risk for patients are classified 3 situations: simple compounding, moderate and complex compounding. It is requested to produce the master formulation records and the compounding record. Like NBP the USP rules are based on the quality of final products and on the documentation of all process. Some preparations at high microbiological quality need to be prepared in zone with HEPA FILTER. A translation of Simplified NBP and its philosophy (DM Salute 18.11.2003) and their meaning are reported
Results
Translation of the meaning of the NBP procedure simplified
DM 18/11/2003 Application field :( nonsterile magistral and
officinal forms reduced lots) for hospital and community pharmacy
medical prescription for magistral formula and Pharmacopeia for
Officinal reduced scale production) Preliminary evaluation about
opportunity -possibility to prepare the galenic requested or needed
definitions: magistral formula, officinal, reduced batch laboratory
hygienic written procedure, frequency (provided by director of the
pharmacy or lab. Responsible). lab area: it must be adequate for
the kind of galenic products produced, ceiling and walls wahable.
It can be in a separate room, separate or not separate inside the
pharmacy. Instruments: mandatory according PHARMACOPEA
uff. ITALIAN table n. 6, the measure instrument must be verified
in regular way. The refrigerator must be cleaned. Containers (and
related certificate of conformity to pharmacopeia requirement of
the primary containers). Raw material: chemical denomination,
date of arrive in pharmacy, batch number, expiration date or date
of reticulation, certificate of analysis signed by producer (according
to pharmacopeia quality requirement), conservation condition
or use, date of first use. (necessary a register of raw materials,
excipients and API, with a progressive numeration). The empty
container of raw material must be kept for 6 months after final
use. Fulfillments (preventive and after setup) to the preparations.
Prescription verifies, normative requirement, sign of the physician,
iperdosages verify (according to table n. 8 pharmacopeia Italy),
Incompatibility verify, the possibility to prepare in lab. After setup:
to be written on the prescription the progressive number of the
preparation, date of the preparation, expiration date, excipients
used, precautions and cautions, label must be attached. Sign of
the pharmacist in the label, on the prescription or on the working
sheet Labeling etcetera – batch number and expiration date,
composition qualitative quantitative, API Excipients, date limits for
use, precautions, Price (community pharmacy) Documents storage
-conservation documentation (time), empty bottle. The written
prescription must be kept in the pharmacy for 6 months and the
same working sheet. (working sheet). The prescription of narcotics
must be kept in pharmacy for the time required by normative rules.
Quality control: right following of the procedure, organoleptic
characteristics, control of the packaging, sealing of the container,
right label copilation, mass uniformity, acceptation limits. A copy
of the label must be attached to the working sheet Documentation:
of the working space, instruments, raw materials Expiration time
of the drugs prepared: according to FU requirement: 30 days
that can be prolonged to 6 months according chemical -physical
microbiological stability documented by official information’s.
Mandatory equipment and tools utensil in pharmacy a (TABLE N 6
pharmacopeia Italian in force)
1. balance sensitivity to the mg, scale = 0,001 g, loading
capacity at least 500 g or in alternative way two different
balances, one with sensitivity at the mg (d=0,001g) with
loading capacity at least 50 g and the other with sensitivity at
0,50 g (d=0,50 g) with carry load at least of 2 kg.
2. Bain Marie or other equipment that can assure, in heating,
temperature since to 100 °C.
3. Fridge able to assure the right storage conditions
according pharmacopeia requirement
4. Point of fusion equipment. (to test the raw material)
5. chemical glassware, also graduated sufficient for the
execution of the preparation.
6. percolator – at empty Concentrator (1).
7. encapsulate (2)
8. Tablet press (3).
9. powder Aspiration system (4).
10. molds or plastic valves for ovules and suppositories (5).
11. 11.tools and devices necessary to guarantee sterility of
the preparation (6)
Beyond the reported instruments, the pharmacy must have
all other instruments, equipment’s, tools, materials, products
and reactive adequate to the number end to the nature of the
preparations usually performed and of suitable tools for their check
to be done according to the Pharmacopeia indications. Pharmacy
that executes injectable preparations must have also materials,
equipment, and tools essential to these preparations and for all
the control expected by pharmacopeia for this specific kind of
preparation.
Note:
1. mandatory for pharmacy that prepare extracts. They
must be of materials and adequate dimension to the volume
and related the preparation to be executed.
2. mandatory for the pharmacy that prepares capsules.
3. mandatory for the pharmacy that prepares tablets.
4. mandatory for pharmacy that prepare tablets, capsules,
capsule, teas or sachets.
5. mandatory for pharmacy that prepare suppositories and
ova.
6. for pharmacy that prepares sterile products.
Experimental Project
In order to evaluate the application of REDUCED NBP in an hosp. galenic lab PC AREA are reported All official nonconformity registered from 2008 to 2023. (the internal production) Results: no major nonconformity registered related to the preparation activity. (for the non serile galenic activity), only 2 secondary- minor NC due by an excipient to be modified to increase solubility of an API and related a closing system for an oral power.
Discussion
As reported in this work are clear the advantages to produce some kinds of drugs in a galenic laboratory. Even the industrial epoca, with the pharmaceutical industry increase, the industrial production of drugs Was rapidly developed and so reduced or stopped the production in the galenic laboratory: this process was due to the complexity process to produce with high quality the finished drugs in the amount requested by the hospital and the patient. But the same some condition needed to manteign this procedure: for magistral prescription single patient based and for the production of disinfectants, reagents or other product. It must also to be remembered that during LAST COVID-19 PANDEMIA one of the main producers of antiseptic gel hands and alcoholic solution was the hospital pharmacy in their lab as well as in the private pharmacy. The industry in this situation was not able to provide ready to use great amount of this product in few times as needed for the public safety. (3) The galenic hospital laboratory in the public hospital was able to guarantee this production and the safety of the patient and healthcare professional. The results of practical experience reported show also in a specific setting the goodness of this rules NBP even if simplified. The technological innovation makes possible to better cover the need for drugs shortcomings. Comparing full NBP to the reduced DM 10nov 2003 it is possible to verify that NBP requires separate or separable locals, check by another pharmacist vs the one that prepares the drug in lab. and required as mandatory written procedures accredited. For DM it is not mandatory to have complex quality checks on the final products, no mandatory written procedure is needed (even if suggested). In this work it is also submitted a new technology useful in galenical laboratory: the 3D PRINTING SYSTEM As an innovation for quality and efficiency of the process.
Conclusion
As conclusion it is possible to say that observing the Italian Reduced NBP rules in an advanced country can be applied also in non-advanced countries with great benefit for healthcare of the patients. Related to the specific preparation requested by the clinicians. These rules report general behavior and procedure to be followed to be sure that the drugs produced are safe and useful for the patients. Not all laboratories in the world have the same instruments or complex laboratory, but in every laboratory. It is crucial to know the responsibility as well as procedure adopted (quality control of raw material, active substantive, qualification of the pharmacist, traceability of the lots and other). For this reason, it is opinion of the author that these rules must be translated in their general meaning from Italian to English languages as reported in this work. The authors submit to the researchers and pharmacists a new innovative tool: the 3D PRINTING systems for galenic laboratory use: a system to increase global efficiency of the preparation of capsules or other pharmaceutical form during a period of drug shortages.
Acknowledgement
None.
Conflict Of Interest
No conflict of interest.
References
- Luisetto M (2017) Editorial the Clinical Pharmacists Main Focus. Journal of Applied Pharmacy 9(4).
- Mauro LUISETTO, Francesca CARINI, Giovanni BOLOGNA, Behzad Nili-Ahmadabadi (2015) RESEARCH ARTICLE Pharmacist Cognitive Service and Pharmaceutical Care: Today and Tomorrow Outlook UK Journal of Pharmaceutical and Biosciences 3(6): 67-72.
- Fiazza C, Ferraiuolo A, Luisetto M, Sahu R (2020) Galenic hospital laboratory during COVID-19 emergency: A practical experience in an advanced country. Int J Clin Virol 4: 118-125.
- Mauro Luisetto (2017) RESEARCH ARTICLE Attitudes and Skills in Business Working Settings: A HR Management Tool Business and Economics Journal Mauro, Bus Eco J 8(1).
- M Luisetto (2016) RESEARCH ARTICLE management instrument in pharmaceutical care and clinical pharmacy Intern. journal of economics and management sciences Luisetto et al., Int J Econ Manag Sci 5:5.
- V Damuzzo, Riccardo B, Daniele M, M Chiumente, Melania R, et al. (2023) Hospital Pharmacy Response to Covid-19 Pandemic in Italy: What We Learned from the First Outbreak Wave J Pharm Pract 36(1): 87-95.
- Francesca B, Antonio G, Gaetano DL, Richard P, Paola B, et al. (2014) Establishment of galenic laboratories in developing countries to produce high quality medicines: results of Aid Progress Pharmacist Agreement (A.P.P.A.®) Project Journal List Croat Med J v Croat Med J 55(6): 662-668.
- Géraldine LB, Christel C, Clarisse RM, Sophie B, Sandrine A, et al. (2018) Impact of collaborative pharmaceutical care on in-patients' medication safety: study protocol for a stepped wedge cluster randomized trial (MEDREV study) Trials 19(1): 19.
- Johannes Wohlrab (2016) Topical preparations and their use in dermatology. J Dtsch Dermatol Ges 14(11): 1061-1070.
- Marija Dj, Jovović, Maja M Ribar (2015) Information on the Quality of Substance for the Preparation of Pharmaceutical Drugs in Terms of Hospital Pharmacy Hospital Pharmacology 2(1): 220-224.
- Agueda Cabral de SP, Elaine SM, Selma RC, Débora OF, Lenise AT, et al. (2016) Magistral drugs in hospitalized newborns and children Medicamentos magistrais em recém-nascidos e crianças hospitalizados 34(4): 403-407.
- Dooms M, Carvalho M (2018) Compounded medication for patients with rare diseases. Orphanet J Rare Dis 13(1): 1.
- Nataša JL, Aleksandra JG, Svetlana S, Nikola J, Slobodan G, et al. (2021) Medicine Shortages in Serbia: Pharmacists’ Standpoint and Potential Solutions for a Non-EU Country Umberto Musazzi Pharmaceutics 13(4): 448.
- Guendalina Z, Silvana A, Danilo M, Valentina I, Paola B, et al. (2022) Mini-Tablets: A Valid Strategy to Combine Efficacy and Safety in Pediatrics Pharmaceuticals (Basel) 15(1): 108.
- Seoane-Viaño, Sarah J Trenfield, Abdul W Basit, Alvaro Goyanes (2021) Translating 3D printed pharmaceuticals: From hype to real-world clinical applications Advanced Drug Delivery Reviews 174: 553-575.
- Christoph N, Giuseppe M, Emeric C, Jean-MR, Samira B, et al. (2019) Feasibility study into the potential use of fused-deposition modeling to manufacture 3D-printed enteric capsules in compounding pharmacies International Journal of Pharmaceutics: 569(5).
-
Luisetto M*, Khaled Edbey, Fiazza C, Mashori Gulam Rasool, Nili B Ahmadabadi, Cabianca L and Oleg Yurevich. Non-Sterile Clinical GALENIC LABORATORY: A Scientific Discipline Between Laboratory Practice Clinical Pharmacy and Personalized Pharmacological Therapy. Arch Phar & Pharmacol Res. 4(2): 2024. APPR.MS.ID.000579.
-
Non-Sterile, Clinical Pharmacy, Pharmacological Therapy, Galenic Laboratory, Pharmaceutical Care, 3D Printed Capsules, Control Process, Magistral Formula, Medicine Shortage, Rare Disease, Official Pharmacopeia
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






