 Review Article
Review Article
Treatment of Infected Tibial Non-union: A Systematic Review and Meta-Analysis
Mohammed Anter Meselhy*, Gamalahmed Hosny, Adelsamyelhammady and Peter MamdohZaki
Department of Orthopedics, Benha University, Egypt
Mohammed Anter Meselhy, Department of Orthopedics, Benha University, Egypt.
Received Date:July 24, 2020; Published Date: September 17, 2020
Abstract
Objectives: The aim of this work is to systematically review and make meta-analysis for treatment of the infected non-union of the tibia.
Methodology: A systematic review was completed, Study objective and comprehensive literature search were performed from the SCI, PubMed, Cochrane Library; and Embase between January 2000 and Feb. 2019. Some major data were statistically analyzed including number of patients, manage, external fixation time, Searches will be performed in the MEDLINE, Life Science Citations, PubMed, Google Scholar and EMBASE Biochemical (http://www.embase.com) databases will be accessed to search studies with no limits set during research, Terms aimed at capturing the target diagnosis, such as “infected tibial nonunion” and “fixation” were combined using the Boolean operator “or” and MeSH terms.
Result: 318 abstracts were identified during the search, 10 were excluded, 308 full articles were fully reviewed, 295 articles were excluded, 13 studied matched the inclusion criteria and were included in this review, 2 additional articles were identified during searching, a total 652 patients of 15 studies were presented in this systemic review.
Conclusion: Radical debridment of the infected non-union is mandatory, a satisfactory bone results and functional results were obtained. On the other hand Ilizaov technique proved as the most useful method in the treatment of the infected non-union of the tibia.
Keywords: Tibial; Nonunion; Infected; Ilizarov
Introduction
Tibial shaft non-union is considered the commonest type of long bone non-union, the aetiological factors are due to high incidence of severe open fractures, high energy trauma associated with vascular and soft tissue compromise, infection and bone devitalization and segmental bone loss [1-5]. In this review, analysis of the different methods for the treatment of the infected non-union of the tibia and the results to find the most successful technique with a satisfactory outcome.
Subjects and Methods
Study objective and comprehensive literature search were performed from the SCI, PubMed, Cochrane Library and Embase between January 2000 and Feb 2019. Some major data were statistically analyzed, including number of patients, manage, external fixation time, Searches will be performed in the MEDLINE, Life Science Citations, PubMed, Google Scholar and EMBASE Biochemical (http://www.embase.com/) databases will be accessed to search studies with no limits set during research, Terms aimed at capturing the target diagnosis, such as “infected tibial nonunion” and “fixation” were combined using the Boolean operator “or” and MeSH terms.
Selection criteria
1) Prospective or retrospective studies discussing treatment of infected Tibial nonunion.
2) Journal articles, studies and papers are all involved.
3) Clinical studies within last 18 years.
Exclusion criteria
i. Non-human studies and case reports.
ii. Cadaveric studies.
iii. Reviews, Commentaries and general discussion papers not presenting data on impacts.
Statistical analysis
The collected data will be presented as suitable tables and illustrated as suitable figures. Analysis of data will be with the aid of software package of SPSS using suitable statistical tests. For all studies, patient selection, study inclusion and exclusion criteria, patient characteristics, procedure, protocol and outcomes measured were extracted using standardized data extraction forms. Outcomes were also extracted from each study. During data extraction, each included study was assessed for quality using the Cochrane Risk of Bias Checklist.
Results
318 abstracts were identified during the search, 10 were excluded, 308 full articles were fully reviewed, 295 articles were excluded, 13 studied matched the inclusion criteria and were included in this review, 2 additional articles were identified during searching [6-20], a total 652 patients of 15 studies were presented in this systemic review (Table 1).
1) The studies included are retrospective and prospective, Outcome measures were reported in most of the studies according to ASAMI score. This includes mainly bone results and functional outcome. Some papers reported further data.
2) Study designs, study period and outcome measures are shown in (Table 2).
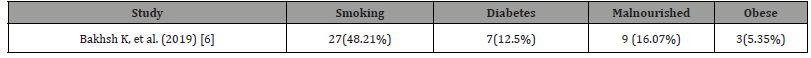
Regarding the type of bacteria causing the bone infection was not mentioned in studies [7-9,11,13,15,18]. While Madhusudhan TR, et al. [12] reported mixed bacterial growth (Table 3). Associated comorbidities were not mentioned in the majority of studies (Table 4). Only Bakhsh K, et al. [6] reported Smoking, Diabetes, malnourishment and obesity as associated comorbidities.
Table 1: Characteristics of included studies.
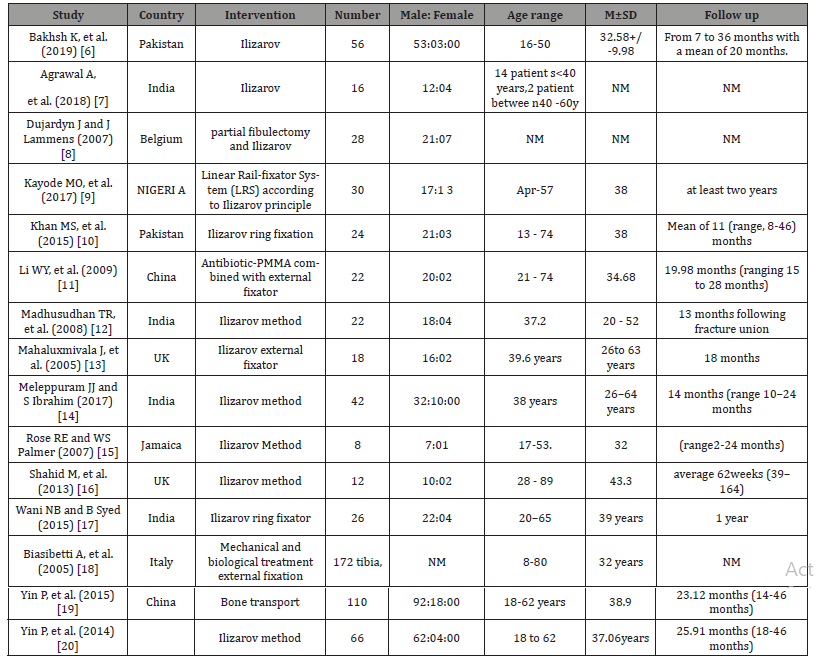
Table 2: Study design and outcome measures.
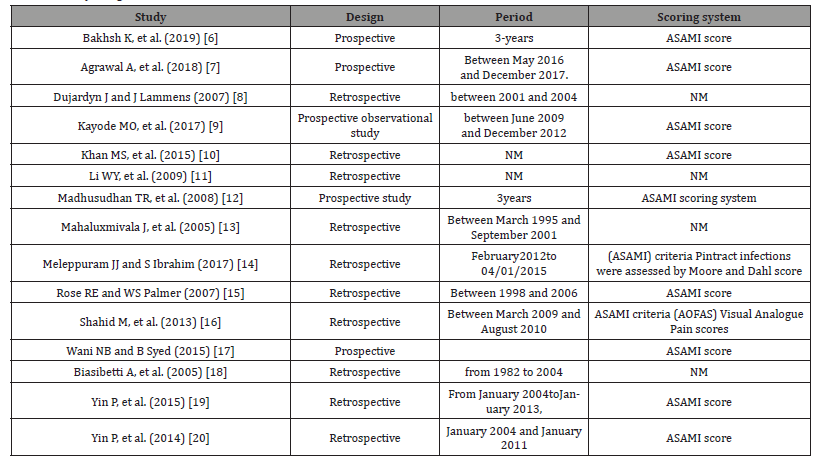
Table 3: Bacteria causing bone infection.
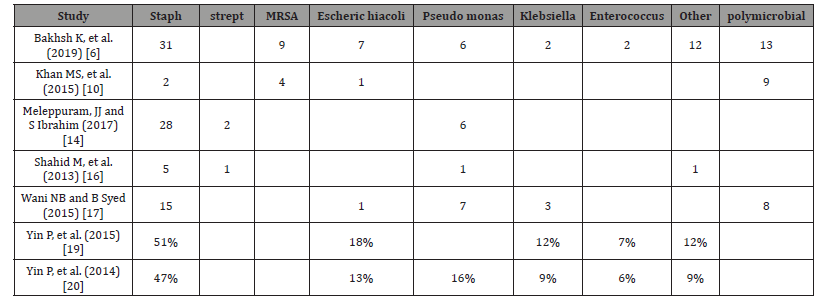
Table 4:Associated comorbidities.
Bone results and functional results
I. The criteria are commended by ASAMI were adopted to evaluate bone results and functional results in the studies [6,7,10,12,14-17,19,20]. Bone results were evaluated by 4 criteria: union, infection, deformity and limb-length discrepancy.
II. Functional results were evaluated by 5 criteria: active, limp, minimum stiffness (knee or ankle joint), reflex sympathetic dystrophy and pain.
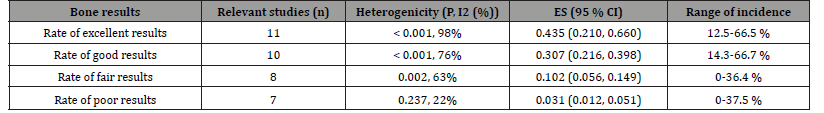
III. Bone results were evaluated in12 studies by ASAMI [6,7,10,12,14-17,19,20] Random effects meta-analysis showed that the weighted frequency of excellent rate, good rate, fair rate and poor rate in bone results were listed in (Tables 5,6,7).
Table 5:Bone results.
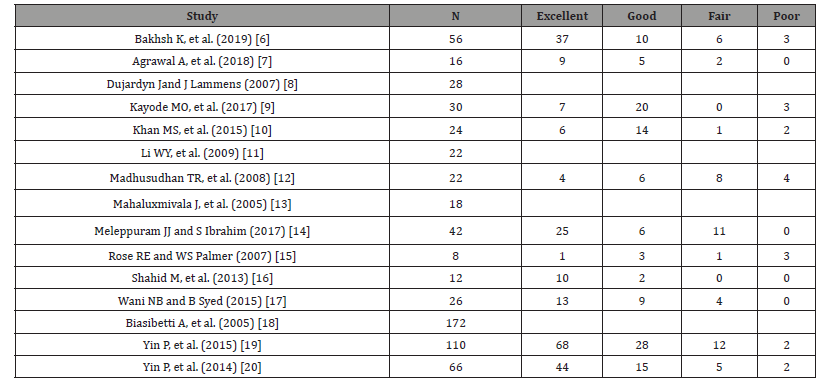
Table 6:Functional outcome.
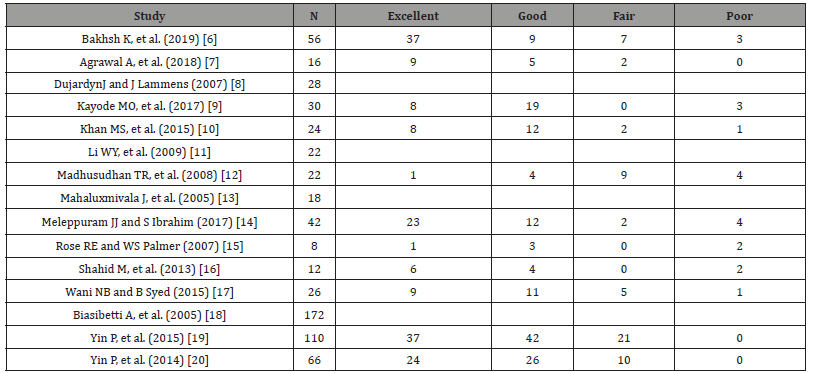
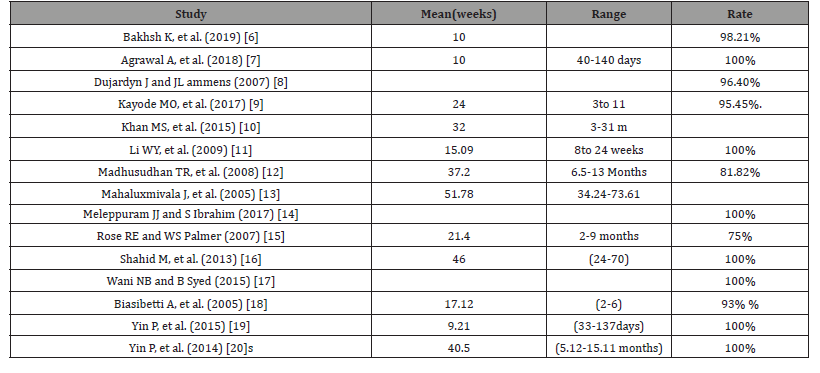
Table 7:Bone union.
External fixation index
The external fixation index denotes the number of days the external fix at or is attached to the bone per centimeter of length gained. Using conventional Ilizarov fixation, this index is typically thirty days per centimeter of length gained (Table 8). However, the rate differs based on variables such as patient age, osteotomy site and amount of lengthening [20,21]. In the selected studies, it was not reported in all. Ranged between 1.2 and15.7 [6,10].
Complications
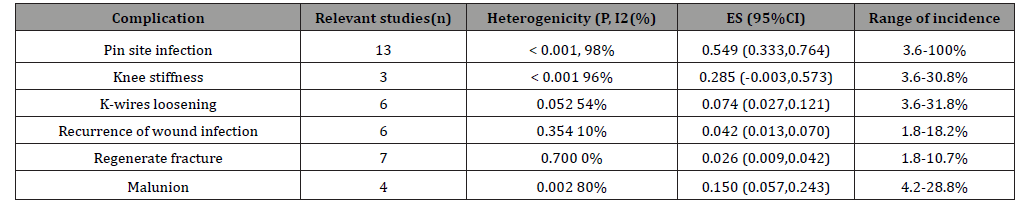
Pinsite infection, kneestiffness, K-wires loosening, recurrence of wound infection, regenerate fracture, Malunion, paraesthesia, softtissue impingement and Mortality was reported. Pintract infection was the most common complication and it was managed by antibiotics in all studies. Mortality was reported in one case by Khan, et al. [10]. Complications are listed in (Table 9). According to Bakhsh, et al., the associated soft tissue defect shealed by soft tissue transport, VAC dressings and fasciocutaneous flaps [6].
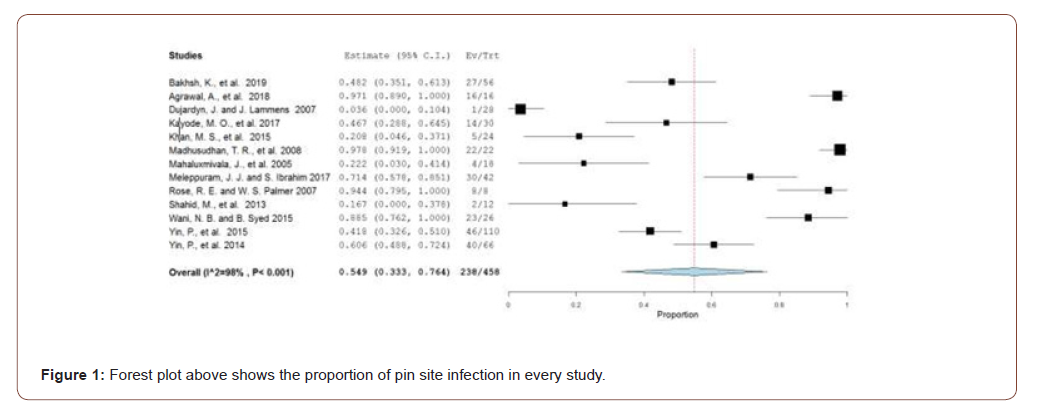
Meta-analysis of bone results
Rate of excellent, good, fair and poor bone results are shown in Table 10 (Figure 1).
Table 8:External fixation Index.
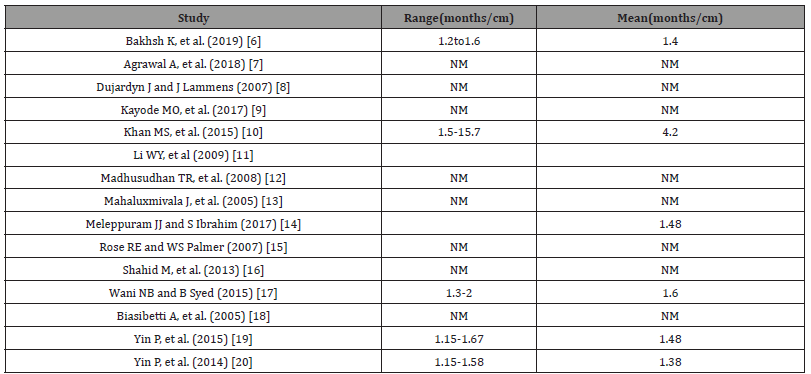
Table 9:Post-operative complications.
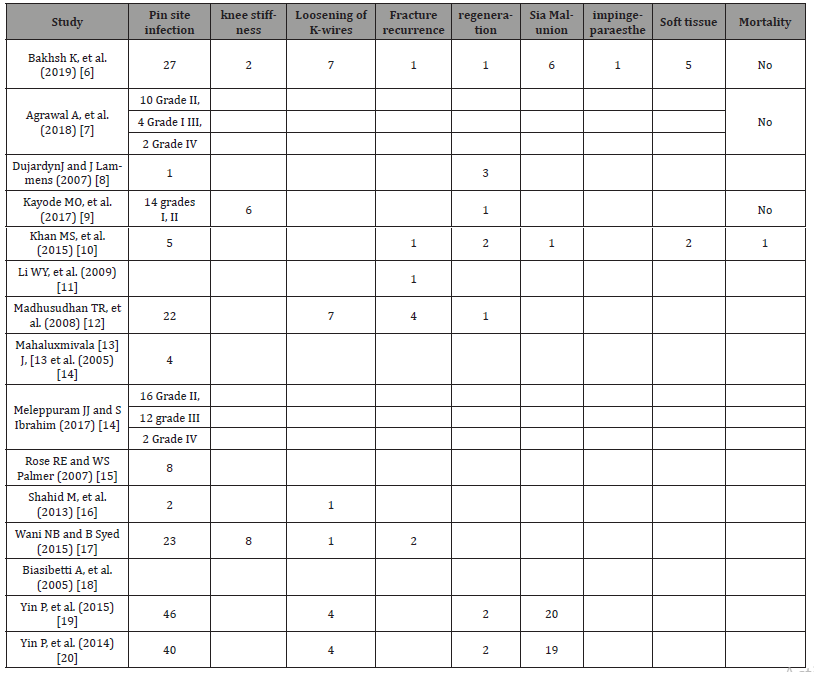
Table 10:Meta-analysis of bone results.
Discussion
Infected non-union of the tibia is still challenging, especially with presence of bone and soft tissue defect, it was proved that Ilizarov external fixator show a high rate of success in the treatment of such difficult cases [20]. Debridment of devitalized bone and soft tissue, antibiotic therapy and antibiotic impregnated beads can lead to acceptable cure rate in less virulence infection, while in sever type of bone infection radical debridment, stable external fixator and bone transport or compression distraction are mandatory to gain bone union [21,22]. Papineau technique, tibiofibular synostosis, other bone substitutes is of limited ability to reconstruct the limb length discrepancy and to correct the limb deformity [22]. in addition to lack of limb movement [23].
Ilizarov and his follows since 1950 have employed new biological techniques and a different system of external fixation to achieve union, correct deformity eradicate infection, limb length restoration, in association of maintaining of limb function [22,23]. Ilizarov apparatus is a very good tool to treat large bone defects due to radical debridment in infected nonunion [22,23]. It can be done either by trifocal osteosynthesis or bifocal osteosynthesis, or by gradual fibular transfer [24].
This is a systematic review of the treatment of infected nonunion of tibia. The majority of the studies used Ilizarov method. This systematic review included 15 studies, and we conducted a meta-analysis of 11 studies to evaluate the efficacy of fixation method in the treatment of infected nonunion of tibia. The poor rate in bone results and functional results was 4.6% (95%CI, 0.012, 0.051; I2 = 22%, P = 0.237) and 4.9% (95%CI, 0.057, 0.243; I2 = 80%, P = 0.002). The data were not statistically heterogeneous. So, these results showed that the patients with infected nonunion of tibia treated by Ilizarov methods had a low rate of poor bone and functional results.
We did a meta-analysis of complication in patients with infected nonunion of tibia treated by Ilizarov method. Statistically homogeneity was found in most of the complications (Tables 11,12). Pin-track infection is the most common complication by using Ilizarov methods, and significant statistically heterogeneity was found in the complication. The rate of pin-track infection was 3.6-100% among included studies in our systematic review. Hence, we considered that careful pin care was the key to reducing the complication. The data of infected tibia nonunion could be found in (Tables 5,6). The poor rate in bone results and functional results was was 4.6% (95%CI, 0.012, 0.051; I2 = 22%, P = 0.237) and 4.9% (95%CI, 0.057, 0.243; I2 = 80%, P = 0.002). The rate of Pin site infection, knee stiffness, K-wires loosening, recurrence of wound infection, regenerate fracture, Malunion, paranesthesia soft tissue impingement and Mortality were respectively 36.50%, 2.45%, 3.68%, 1.38%, 1.84%, 7.06%, 0.15%, 1.07% and 0.15%. These data were not statistically heterogeneous.
Table 11:Meta-analysis of functional results.
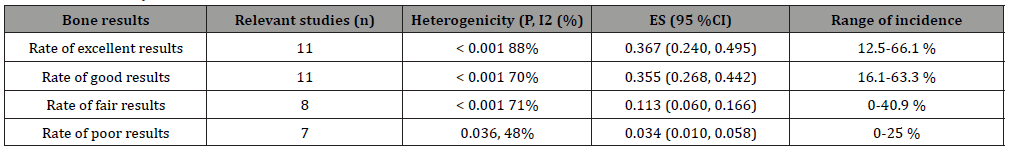
Table 12:Meta-analysis of complications.
We also conducted meta-analyses of bone and functional results in our systematic review. High heterogeneity existed in several pooling data in our study, and we thought the heterogeneity was probably resulted from the different research quality, various surgeons’ experience and diversity of rehabilitation nursing. Failure to include the non-English language studies in our article could have resulted in missing data and our estimates of effect size might have been biased, nevertheless, 15 studies were included in our article and they were not excessively affected by significant statistical heterogeneity. The data of the present review were extracted from observational studies, which are likely to cause both systematic and random errors. Therefore, more prospective randomized controlled trials are needed to overcome the limitation of this study.
Conclusion
In conclusion, our systematic review showed that the patients with infected nonunion of tibia treated by Ilizarov methods had a low rate of poor bone and functional results. Therefore, Ilizarov methods may be a good choice for the treatment of infected nonunion of tibia.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Phieffer LS, Goulet JA (2006) Delayed unions of the tibia. J Bone Joint Surg Am 88(1): 206-216.
- Fenton P, Bose D (2014) Patient-reported outcomes following treatment of tibial non-union with circular frames. Strategies Trauma and Limb Reconstr 9(1): 33-35.
- Deng Z, Cai L, Jin W, Ping A, Wei R (2014) One-stage reconstruction with open bone grafting and vacuum-assisted closure for infected tibial non-union. Arch Med Sci 10(4): 764-772.
- Said G, El Sharkawi M, Said H, Refai OA (2011) Fibula-pro-tibia in plating tibial non-unions. Int Orthop 35(11): 1713-1718.
- Salih S, Blakey C, Chan D, Mc Gregor Riley JC, Royston SL, et al. (2015) The callus fracture sign: a radiological predictor of progression to hypertrophic non-union in diaphyseal tibial fractures. Strategies Trauma Limb Reconstr 10(3): 149-153.
- Bakhsh K, Atiq Ur Rehman, Faridullah Khan Zimri, Eid Mohammad, Wazir Ahmed, et al. (2019) Presentation and management outcome of tibial infected non-union with Ilizarov technique. Pak J Med Sci 35(1): 136-140.
- Agrawal A, H Sakale, B Kar (2018) Management of infected nonunion of tibia by Ilizarov technique. Journal of Orthopedics, Traumatology and Rehabilitation 10(1): 1-6.
- Dujardyn J, J Lammens (2007) Treatment of delayed union or non-union of the tibial shaft with partial fibulectomy and an Ilizarov frame. Acta Orthop Belg 73(5): 630-634.
- Kayode MO, OA Adewole, MO Shoga, SO Giwa (2017) experience with managing complicated fractures using Ilizarov principals in Lagos, Nigeria. J West Afr Coll Surg 7(3): 24-43.
- Khan MS, Haroon Rashid, Masood Umer, Irfan Qadir, Kamran Hafeez, et al. (2015) Salvage of infected non-union of the tibia with an Ilizarov ring fixator. J Orthop Surg (Hong Kong) 23(1): 52-55.
- Li WY, Bo song Zhang, Long Zhang, Wang Zheng, Shu hui Zheng, et al (2009) Antibiotic-PMMA beads combined with external fixator for treating the infected fracture nonunion. 22(2): 90-92.
- Madhusudhan TR, Balasundaram Ramesh, Ks Manjunath, Harshad M Shah, Dabir C Sundaresh, et al. (2008) Outcomes of Ilizarov ring fixation in recalcitrant infected tibial non-unions - a prospective study. J Trauma Manag Outcomes 2(1): 6.
- Mahaluxmivala J, R Nadarajah, PW Allen, R A Hill (2005) Ilizarov external fixator: acute shortening and lengthening versus bone transport in the management of tibial non-unions. Injury 36(5): 662-668.
- Meleppuram JJ, S Ibrahim (2017) Experience in fixation of infected non-union tibia by Ilizarov technique - a retrospective study of 42 cases. Rev Bras Ortop 52(6): 670-675.
- Rose RE, WS Palmer (2007) The Illizarov method in infected non-union of long bones. West Indian Med J 56(3): 246-251.
- Shahid M, Abid Hussain, Phillipa Bridgeman, Deepa Bose (2013) Clinical outcomes of the Ilizarov method after an infected tibial non-union. Arch Trauma Res 2(2): 71-75.
- Wani NB, B Syed (2015) Ilizarov ring fixator in the management of infected non-unions of tibia. Sicot j 1: 22.
- Biasibetti A, Domenico Aloj, Giuseppe Di Gregorio, Alessandro Massè, Carlo Salomone (2005) Mechanical and biological treatment of long bone non-unions. Injury 36 Suppl 4: S45-S50.
- Yin P, Lihai Zhang, Tongtong Li, Li cheng Zhang, Guoqi Wang, et al. (2015) Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg Res 10: 49.
- Yin P, Q Zhang, Z Mao, T Li, L Zhang, et al. (2014) The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods. Acta Orthop Belg 80(3): 426-435.
- Arora S, Sumit Batra, Vikas Gupta, Aman Goyal (2012) Distraction osteogenesis using a mono lateral external fixator for infected non-union of the femur with bone loss. J Orthop Surg (Hong Kong) 20(2): 185-190.
- Samanta A (2016) Ilizarovring fixator intreatment of infected nonunion of tibia. Saudi Journal of Sports Medicine 16(2): 159-161.
- McKee MD, Dennis J DiPasquale, Lisa M Wild, David JG Stephen, Hans J Kreder, et al. (2003) The effect of smoking on clinical outcome and complication rates following Ilizarov reconstruction. J Orthop Trauma 17(10): 663-667.
- Meselhy MA, M Singer, Halawa A, Hosny GA, Adawy HA, et al. (2018) Gradual fibular transfer by Ilizarov external fixator in post-traumatic and post-infection large tibial bone defect. Arch Orthop Trauma Surg 138 (5): 653-660.
-
Mohammed Anter Meselhy. Treatment of Infected Tibial Non-union: A Systematic Review and Meta-Analysis. 1(2): 2020. APHE. MS.ID.000508.
-
Tibial, Nonunion, Infected, Ilizarov, Bone devitalization, Pain, Paraesthesia, Tibiofibular synostosis.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






