 Opinion
Opinion
Static Automated Perimetry: Hand in Hand with the Neurologist
Iman M Eissa, Assistant Professor of Ophthalmology, Cairo University, Egypt.
Received Date: May 09, 2019; Published Date: May 16, 2019
Opinion
With the development of science and the rapidly evolving imaging techniques, patients with neurological deficits are more readily and accurately diagnosed nowadays. Be it a stroke, intracranial hemorrhage, demyelinating disease or an intracranial tumor. While the general ophthalmologist may not encounter these cases on daily basis, it is essential that he be aware of the neurological deficit symptoms which present with each and every cause. Knowing when to refer to a neurologist and when to suspect an intracranial pathology can be lifesaving. While cases of demyelinating disease and / or intracranial tumors may sometimes first present to an ophthalmologist (About 30 % of MS cases present with optic neuritis as a first presentation)[1], they are more commonly referred to the ophthalmologist by a neurologist for visual assessment, fundus and optic nerve head examination, and/ or field testing. Testing the patient’s field of vision (perimetry) as well as his visual evoked potential (VEP) are essential steps in the assessment of an initial attack of optic neuritis. ON is one of the most common initial clinical presentations of MS in patients without any previous history of a demyelinating event. When a patient is referred to neurology with ON, one of the most common questions would be the possibility of conversion to MS and thus long-term management.
While most ophthalmologists will order a field test for the follow up of glaucoma, perimetry is surprisingly equally informative if not diagnostic in patients with neurological problems. Currently the most used technology to test for the visual field is automated static perimetry; which is a computer-based program. With most automated perimeters, the stimuli are static: stimuli (usually Goldmann standard size III white) are randomly presented at predetermined locations within a specified region of the visual field. Testing is typically restricted to the central 24° or 30° for speed and patient compliance but equally important, because of the overwhelming representation of the central visual field in the human striate cortex. The central 24° tests 80% of the visual cortex, whereas the central 30° tests 83% of the cortical area [2].
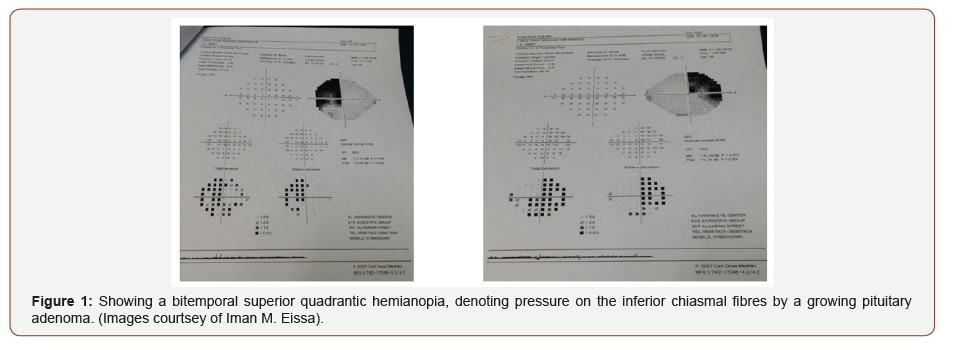
Of cases presenting with a very characteristic pattern of visual field loss on perimetry, are patients with a pituitary adenoma. As a benign adenoma enlarges, it presses on the overlying crossing visual nerve fibres of the optic chiasm. These are the axons of the ganglion cell layer coming from the nasal retina of both eyes. Thus, when interrupted by a growing pituitary adenoma, a characteristic “bitemporal hemianopia” respecting the vertical meridian visual loss results (Figure 1). This is because the two temporal halves of the visual field of both eyes are blurred or lost depending on the severity of the lesion. Here, field testing is conclusive and can be used for follow up after treatment of the pituitary adenoma (Figure 1).
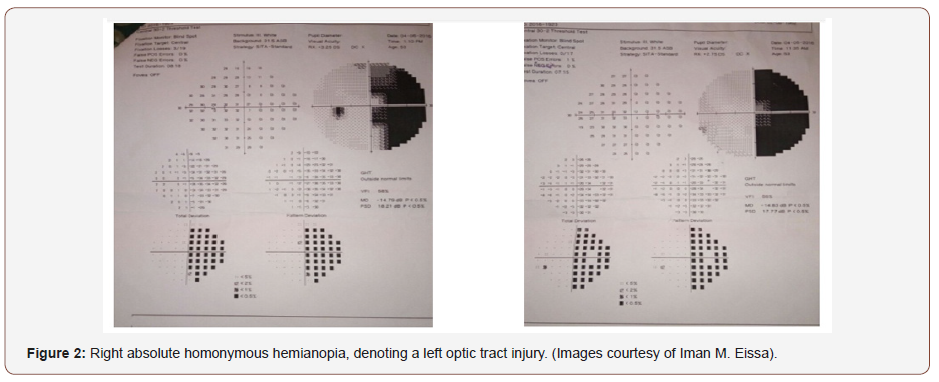
However, if the neurological lesion (be it a stroke, a demyelinating plaque or a growing mass) is causing pressure on the optic tract, which lies more posterior in the visual pathway to the optic chiasm, and which typically carries visual impulses from the contralateral hemifield (ie the right half of the field to the left optic tract and vice versa), a visual field defect known as “a contralateral hemianopia” will occur (Figure 2). This lesion typically involves the same half of the field in each eyes (eg, the right half of the field of the right eye and the right half of the field of the left eye). This characteristic pattern of visual field loss helps localize the lesion. The lost side of the field lies opposite to the injured optic tract (Figure 2).
A patient with retrobulbar neuritis caused by MS gives a characteristic centrocecal scotoma on visual field testing. Similarly, tumors involving the optic nerve as it enters the optic chiasm give a characteristic junctional scotoma, and the list goes on. Despite the availability of highly accurate and advanced brain imaging techniques, visual field testing by automated static perimetry remains a simple, cheap and informative tool used by ophthalmologists and neurologists to diagnose, and confirm suspected visual pathway lesions which in turn, can help localize the level of the neurological insult. The nature of the neurological insult however, remains to be diagnosed by its specific clinical picture as well as by other imaging tools as MRI, and CT.
Acknowledgemnet
None.
Conflict of Interest
No conflict of interest.
References
- Kale Nilufer (2016) Optic neuritis as an early sign of multiple sclerosis. Eye and brain 8: 195-202.
- Abou Zeid N, Bhatti MT (2008) Acute inflammatory demyelinating optic neuritis: evidence-based visual and neurological considerations. Neurologist 14(4): 207-223.
- Adams DL, SincichLC, HortonJC (2007) Complete pattern of ocular dominance columns in human primary visual cortex. J Neurosci 27(39): 10391-10403.
-
Iman M Eissa. Static Automated Perimetry: Hand in Hand with the Neurologist. Arch Neurol & Neurosci. 3(3): 2019. ANN. MS.ID.000565.
-
Neurologist, Static Automated Perimetry, Ophthalmology, Neurological, human striate cortex, Visual field, Pituitary adenoma, Stroke.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






