 Research Protocol
Research Protocol
Posterior Reversible Encephalopathy Syndrome: Is it Always Posterior and Reversible?
Vazquez-Guevara D, Orozco-Narvaez A, Rubio-Hernandez M, Monternach-Aguilar F and Rodríguez- Leyva I*
Neurology Service, Hospital Central “Dr. Ignacio Morones Prieto”, San Luis Potosi, SLP, Mexico
Rodriguez-Leyva I, Neurology Service, Hospital Central “Dr. Ignacio Morones Prieto”, San Luis Potosi, SLP, Mexico.
Received Date: February 21, 2020; Published Date: March 06, 2020
Abstract
Posterior reversible encephalopathy syndrome is a clinical and imagological acute problem characterized by impairment of consciousness, headache, cortical blindness and, epileptic seizures associated with grey and white edema principally localized in temporal-parietal-occipital areas, frequently related hypertensive pregnancy disease. However, not all the cases are associated with pre-eclampsia and eclampsia, and not all of them are related to posterior cerebral edema changes. In this paper is showing ten cases from a Mexican hospital, not all related to pregnancy, neither to posterior vasogenic edema in the image. The immunological patterns were an holo-hemispheric watershed, superior frontal sulcus pattern, dominant parietal-occipital pattern, and a partial or asymmetric abnormality in occipital region bilaterally. Besides the hypertensive disease of pregnancy, we found and hypertensive emergency, renal disease, sepsis, autoimmune illness as etiology. The most had a satisfactory evolution however one was discharged with the minimally conscious state, and another died with a final diagnosis of vasculitis associated with tuberculosis. Therefore, the final result is not always reversible, and neither the image shows a posterior characteristic vasogenic edema.
Keywords: Posterior reversible encephalopathy syndrome; Vasogenic edema; Hypertension; Hypertensive disease of pregnancy
Introduction
Posterior reversible encephalopathy syndrome (PRES) is a clinical-radiological syndrome characterized by acute neurological symptoms (altered mental status, headache, seizures, visual disturbances) and by neuroimaging findings of vasogenic edema in magnetic resonance imaging (MRI) [1]. The are several conditions related to PRES such as hypertension, preeclampsia or eclampsia, kidney disease, immunosuppressive therapy [2]. All of them have in common an injury of the endothelium [3].
Epidemiology. The classic clinical and radiologic presentation of PRES is posterior (i.e., parieto-occipital) [4] and usually these manifestations are reversible, however, has been described other patterns besides the classics [5]. There is no specific treatment for PRES, and sometimes, it is a challenge to eliminate or treat the related condition [1]. Mostly, PRES has excellent short and longterm prognosis [6].
This study aims to describe the clinical and imaging findings and prognosis in the Mexican population.
Methods
Patients who were diagnosed with PRES at Neurology Service at Hospital Central “Dr. Ignacio Morones Prieto” in México were enrolled in PRES database. Data were collected from medical records from 2016 to 2018 on demographics, PRES-related conditions, clinical manifestations, blood pressure measurements at arrival and during hospitalization (defining a hypertensive emergency as an arterial pressure above 180/120), neuroimaging, and clinical recovery time.
Neuroimaging
The radiological PRES patterns were reported on basis patterns reported by Bartynski 2007. There is Holohemispheric watershed pattern (HWP) characterized by vasogenic edema located in the frontal, parietal, and occipital lobes, with lesser involvement of the temporal lobes. Superior frontal sulcus pattern (SFSP): vasogenic edema is located along the mid to posterior aspect of the superior frontal sulcus. Dominant Parietal-Occipital pattern (DPOP): vasogenic edema is located (involved) on the parietal and occipital cortex and white matter with variables involvement of the temporal lobes. Partial or Asymmetric expression (PE) of the primary patterns defined as the absence of signal intensity abnormality in either the parietal lobes bilaterally or the occipital lobes bilaterally [7].
Results
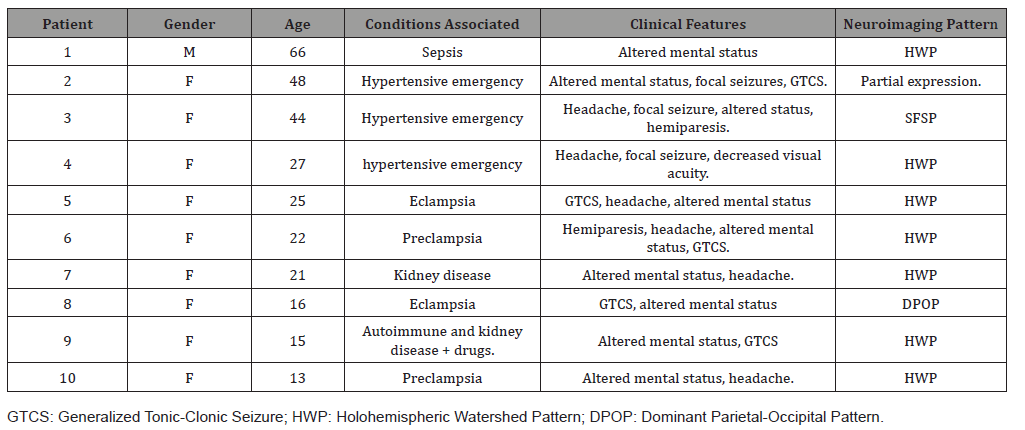
We identified ten diagnosed cases, nine female and one male. Patients age ranged from 13 to 66 years (mean = 29.7). None of these patients had previous episodes of PRES.
Conditions associated with PRES
Drugs (n=1 [10%]); which were tracolimus and mycophenolate mofetil, preeclampsia or eclampsia (n=4 [40%]); all women were in their first pregnancy, hypertensive emergency at arrival (n=3 [30%]), kidney disease (n=4 [40%]), sepsis (n=1 [10%]), autoimmune disease (n=1 [10%]) which was systemic lupus [8].
Clinical manifestations
The most frequent manifestation was altered consciousness on nine patients (90%) with somnolence or stupor. Headache was presented by six patients (60%), the pain was reported bilateral and diffuse in all of them. Seizures were present in 7 patients (70%), generalized in 62.5% and focal in 37.5%. There was one patient with status epilepticus. Focal neurological deficit was present in three patients (30%), one patient with blurred vision and two with hemiparesis [9-12].
Neuroimaging
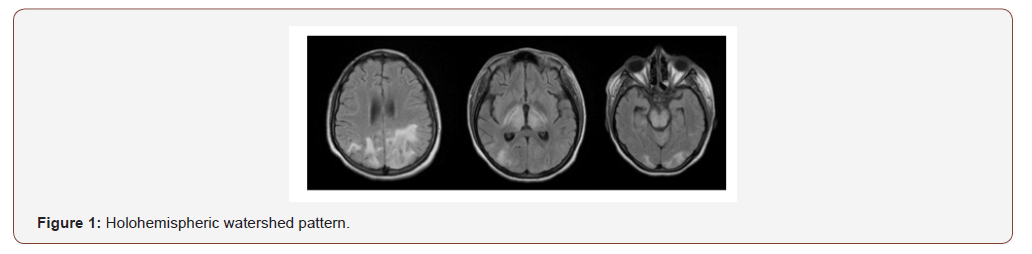
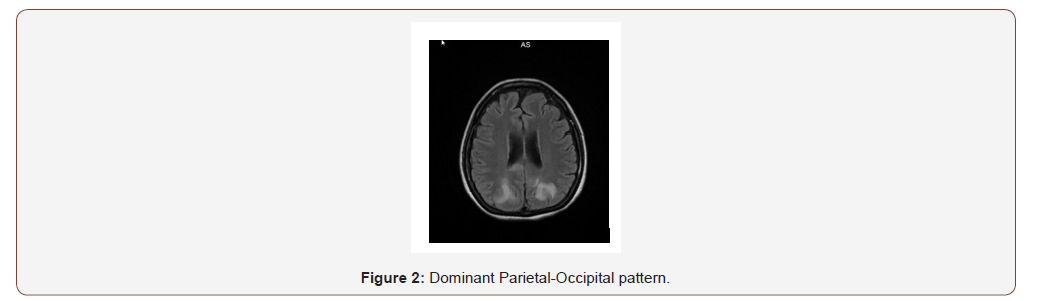
The four patterns of PRES were found. The holohemispheric watershed pattern was the most frequent on seven patients (70%) Figure 1; the other three patterns were found in one patient each (Figure 2). The neuroimaging pattern observed on those who developed preeclampsia was holohemispheric in all of them (Figure 1 & 2) [13-17].
Description of two cases
Case 1
A 25-year-old female with 30 weeks of her first pregnancy presented to the emergency department with generalized seizures, one day before the admission developed sudden-onset of severe headache with duration of about 12 hours. Initially the diagnosis was Eclampsia during the management the blood pressure received aggressive treatment, despite of it persisted with somnolence and the MRI showed PRES with holohemispheric pattern. The patient was discharged home asymptomatic.
Case 2
A 48-year-old female with a medical history of diabetes, hypertension, pulmonary tuberculosis, chronic kidney disease; who was admitted to the hospital for two weeks with fluctuant somnolence and hallucinations. At the day of hospital admission, the patient presented generalized seizures. CT of the brain was not relevant. The lumbar puncture unremarkable, the high blood pressure was difficult to control, developed a refractory status epilepticus and finally died. Her MRI showed a PRES with a holohemispheric watershed pattern. The final postmortem diagnosis was meningitis tuberculosis, there was no evidence of vasculitis (Table 1).
Table 1:General characteristics of the population showed.
Discussion
PRES has many faces and is not always posterior neither reversible. The clinical characteristics associated with arterial hypertension and encephalic dysfunction do not necessarily correlate with the location of the vasogenic edema seen on MRI, which usually has four characteristic patterns.
The description of the two cases emphasized the alteration of the mental state and the presence of seizures were the main clinical presentation, and in both, it was necessary to make a myriad differential diagnosis. The neuroimaging pattern was not the classic parietal occipital, and the prognosis in one of the cases was the worst with irreversible symptoms.
Also, we found a possible association between preeclampsia/ eclampsia and holohemispheric watershed pattern.
There are many questions about the association between the pathophysiology PRES and its neuroimaging and prognosis; It is essential to conduct more studies with a more significant population.
Conclusion
Since PRES is an evolving concept with an underestimated diagnosis, we have to study our patients deeply. A lack of an MRI posterior pattern does not discard this syndrome.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Fugate J, Rabinstein A (2015) Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. The Lancet Neurology 14(9): 914-925.
- Johnson EK, Lin MY (2015) Posterior Reversible Encephalopathy Syndrome. Hosp Med Clin 4: 358-367.
- Gao B, Lyu C, Lerner A, McKinney AM (2018) Controversy of posterior reversible encephalopathy syndrome: what have we learnt in the last 20 years? Journal of Neurology, Neurosurgery & Psychiatry 89: 14-20.
- Brady E, Parikh NS, Navi BB, Gupta A, Schweitzer AD (2018) The imaging spectrum of posterior reversible encephalopathy syndrome: A pictorial review. Clin Imaging 47: 80-89.
- Fischer M, Schmutzhard E (2017) Posterior reversible encephalopathy syndrome. J Neurol 264: 1608-1616.
- Roth C, Ferbert A (2010) Posterior reversible encephalopathy syndrome: long term follow up. J Neurol Neurosurg Psychiatry 81: 773e777.
- Bartynski WS, Boardman JF (2007) Distinct Imaging Patterns and Lesion Distribution in Posterior Reversible Encephalopathy Syndrome. AJNR Am J Neuroradiol 28: 1320-1327.
- Hugonnet E, Da Ines D, Boby H, Claise B, Petitcolin V, et al. (2013) Posterior reversible encephalopathy syndrome (PRES): Features on CT and MR imaging. Diagnostic and Interventional Imaging 94: 45-52.
- Hinchey J, Chaves C, Appignani B, Breen J, Pao L, et al. (1996) A reversible posterior leukoencephalopathy syndrome. N Engl J Med 334: 494-500.
- Granata G, Greco A, Iannella G, Granata M, Manno A et al. (2015) Posterior reversible encephalopathy syndrome—Insight into pathogenesis, clinical variants and treatment approaches. Autoimmunity Reviews 14: 830-836.
- Rykken J, McKinney A (2014) Posterior Reversible Encephalopathy Syndrome. Semin Ultrasound CT MRI 35: 118-135.
- Bartynski WS (2008) Posterior Reversible Encephalopathy Syndrome, Part 1: Fundamental Imaging and Clinical Features. American Journal of Neuroradiology 29(6): 1036-1042.
- Bartynski WS (2008) Posterior Reversible Encephalopathy Syndrome, Part 2: Controversies Surrounding Pathophysiology of Vasogenic Edema. American Journal of Neuroradiology 29(6) 1043-1049.
- Liman T, Siebert E, Endres M (2019) Posterior reversible encephalopathy syndrome. Curr Opin Neurol 32: 25-35.
- Ganesh K, Nair R, Kurian G, Mathew A, Sreedharan S, et al. (2018) Posterior Reversible Encephalopathy Syndrome in Kidney Disease. Kidney Int Rep 3: 502-507.
- Chen Z, Zhang G, Lerner A, Wang AH, Gao B, et al. (2018) Risk factors for poor outcome in posterior reversible encephalopathy syndrome: systematic review and meta-analysis. Quant Imaging Med Surg 8(4): 421-432.
- Liman TG, Bohner G, Heuschmann PU, Endres M, Siebert E (2012) The clinical and radiological spectrum of posterior reversible encephalopathy syndrome: the retrospective Berlin PRES study. J Neurol 259: 155-164.
-
Vazquez-Guevara D, Orozco-Narvaez A, Rubio-Hernandez M, Monternach-Aguilar F, Rodríguez-Leyva I. Posterior Reversible Encephalopathy Syndrome: Is it Always Posterior and Reversible?. Arch Neurol & Neurosci. 7(3): 2020. ANN.MS.ID.000664.
-
Posterior Reversible Encephalopathy Syndrome; Vasogenic Edema; Hypertension; Hypertensive Disease Of Pregnancy, Mental Status, Headache, Seizures, Visual Disturbances, Hypertension, Preeclampsia Or Eclampsia, Kidney Disease, Immunosuppressive Therapy.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






