 Research Article
Research Article
Correlation Between Functional Strength of Lower Limb, Sit to Stand and Functional Ambulation Capacity in Stroke Patients: an ICF Perspective
Rucha Gadgil1 and Isha Akulwar Tajane2*
1MPT Neuro Physiotherapy, K J Somaiya College of Physiotherapy, India
2Associate Professor in Kinesiotherapy and Physical Diagnosis, K J Somaiya College of Physiotherapy, India
Isha Akulwar-Tajane, MPTh Neurosciences, Associate Professor in Kinesiotherapy and Physical Diagnosis, K J Somaiya College of Physiotherapy, Mumbai, India.
Received Date: August 10, 2021; Published Date: May 03, 2022
Abstracts
Background: Stroke is one of major global public health problems responsible for increased morbidity, predisposing an individual to disability.
The International Classification of Functioning, Disability and Health (ICF) is the classification of health and health-related domains and has been
commended as a framework to structure rehabilitation establishing a common language between different health professions. Supporting evidence
linking the three domains of ICF will help in improving the compliance of therapists towards ICF. This study aimed to determine an association
between functional strength, sit to stand and functional ambulation capacity as domains of ICF thereby interlinking the three domains.
Methodology: This was a cross-sectional observational study conducted in the physiotherapy department of a tertiary care hospital in
community-living stroke patients over a period of 18 months. 33 samples participated in the study. Outcome measures used were Upright Motor
Control Test (UMCT), Sit to Stand (STS) on Balance Master and Functional Walking Categorization (FWC).
Results: The data was analysed using Spearman’s correlation Test. The results showed no significant relationship between UMCT and STS
(p>0.05, rs -0.186), a significant negative correlation between FWC and STS (p<0.05, rs -0.355) and a significant high correlation between UMCT and
FWC (p<0.001, rs 0.6474).
Conclusion: Our research established a link between the three domains of ICF viz. impairments, activity and participation in the context of
functional ambulation in patients with stroke.
Keywords:ICF; Stroke; Upright motor control test; Sit -to-stand; Functional walking category; Impairments; Participation; Activity limitation
Abbreviations:ADL: Activities of Daily Living; ICF: International Classification of Functioning, Disability and Health; UMCT: Upright Motor Control Test; STS: Sit-To-Stand; FWC: Functional Walking Category; MMSE: Mini Mental State Examination
Introduction
Stroke is the third leading cause of adult disability in the world and also being the leading cause of long-term disability, it has significant disability-adjusted years of life in both developed and developing countries [1,2]. Motor impairments like hemiparesis are very common and persistent impairments in strength, balance and coordination have been associated with reduced mobility post stroke [3]. The limited walking ability that follows a stroke restricts a patient’s independent mobility around the home and community causing a significant social handicap. Regaining the ability to walk independently is the most important functional goal in rehabilitation of stroke patients; and also, considered as the most meaningful outcome of stroke. The ability to “get out and about” in the community was perceived to be either ‘essential’ or ‘very important’ by 75% of the patients with stroke [4]. Despite the efforts taken to achieve good mobility outcomes, most of the patients with stroke do not get out in the community; more than 80% have difficulty in functional ambulation and are unable to completely reintegrate into the society [4]. It is important that the assessment of stroke recovery not only be limited to nervous system symptoms and functional outcome, but also encompass psychological, physiological, and social function. Typically, during rehabilitation, the assessment of functional status is performed by a number of different observers with various points of view. The International Classification of Functioning, Disability and Health (ICF) as explained by the World Health Organisation (WHO) has been commended as a framework to structure rehabilitation [5]. It aims to provide a way to understand health, health-related states, determinants and outcomes; while also establishing a common language between different health professions [6]. It provides a common concept and standard language for physiotherapy and other rehabilitation disciplines to describe function for patients for conditions like stroke [7]. It was officially endorsed by all 191 WHO Member States in the Fifty-fourth World Health Assembly in 2001 as the international standard to describe and measure health and disability [8]. A “biopsychosocial” model of this type is being increasingly applied in clinical medicine and research, especially in the field of rehabilitation medicine. Such a “biopsychosocial” model is increasingly believed to be the most rational medical approach and use of the ICF as a stroke assessment framework can better reflect and promote this approach [9]. The ICF checklist is a new rehabilitation assessment instrument that is compatible with commonly used clinical assessment scales for stroke and can be used in combination with these scales [9].
Functioning and disability have been devised as multidimensional concepts associated with the body functions and structures of people, their activities, the arenas of life in which they participate [10]. As explained by WHO, ICF encompasses what a person does do or can do, covering not just body functions and structures but also activities and participation together with environmental and other contextual factors. Thus, the ICF focuses on the individual, societal and environmental levels of a person. These components highlight the importance of the interplay and influence of both internal and external factors to each individual’s health status.
The figure below gives a succinct representation of the ICF and its classification as put forth by the World Health Organization [11] (Figure 1):
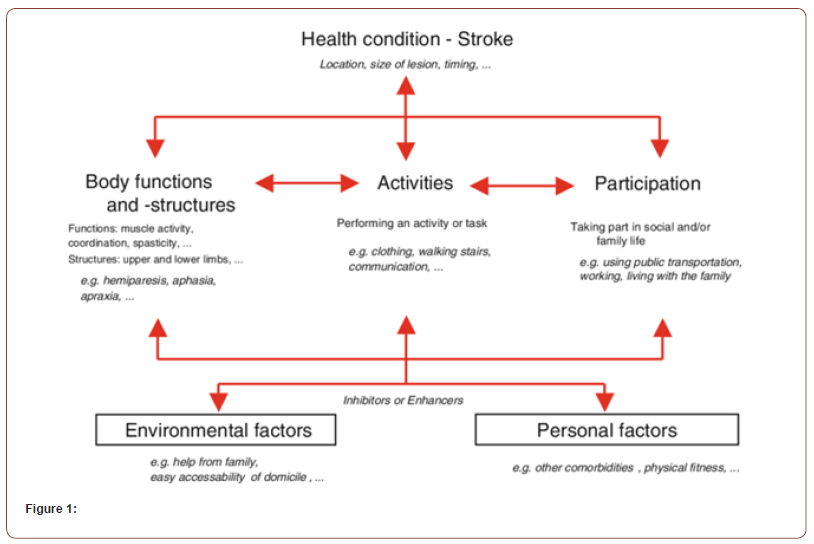
Thus, ICF is a classification of health and health-related domains. Previous studies have shown association within the sub-domains of ICF or association linking any two main domains; e.g. links between capacity and performance; body structure and function. However, literature establishing a relationship between all the three main domains of ICF remains almost non-existent. Though an interdependence of the three can be theoretically rationalised, supporting clinical evidence is required which will help in improving the compliance of therapists towards ICF; determining the clinical & functional outcomes; targeting appropriate treatment for stroke rehabilitation; and to endorse the ICF model in clinical practice. This study was undertaken to determine an association between functional strength; sit-to-stand; and functional ambulation as interlinking domains across the ICF continuum in the context of functional ambulation in patients with stroke.
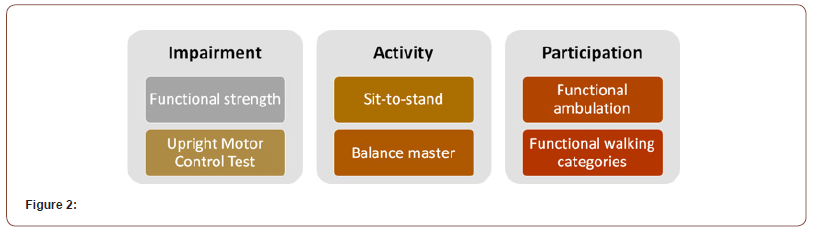
Exploring these domains further, following descriptions aim to provide the context of the study. Clinical experience suggests that one of the most important measures of impairment in determining walking ability is muscle strength. Significant impairment is noted in the lower limb strength after a stroke and may persist in all muscle groups years after the stroke. Research states that there exists a relationship between muscle weakness and post-stroke functional disability in performing mobility tasks like getting out of a chair, standing, walking, and negotiating stairs [12,13]. Precise evaluation of lower limb muscle weakness is therefore an essential component of effective stroke rehabilitation. Within the ICF, it is specifically covered under the Neuromusculoskeletal and Movement related Functions domain.
In activities of daily life, the sit-to-stand (STS) activity is one of the most frequently occurring movements [14]. It is related to functioning and mobility and is a prerequisite for walking. It can be defined as a transitional movement to the upright posture requiring movement of the centre of mass from a stable to a less stable position over extended lower extremities [15]. A stroke can lead to multiple changes in the execution of the STS movement in the acute phase as well as in the chronic phase resulting in a distorted execution of STS movement. It is an important determinant and predictor of clinical and functional outcomes and can be used to assess the measures of self-care and mobility, independent functioning, participation, and quality of life in stroke. In the perspective of the ICF, the STS movement can be primarily positioned in the domain ‘Activities’.
It is seen that although patients achieve walking after a rehabilitation course, they have difficulty in returning to a premorbid life. Only a few patients can perform functional ambulation without any trouble and have to use manual assistance or aids such as a cane or walker to compensate for their impaired walking function [16]. For the same reason, within the ICF, walking ability is considered both an activity and a domain of participation in the environment. Quantitative measures like gait velocity have been shown to relate to strength, however, these measures do not correlate with home and community independence. Functional ambulation is a broader term and is the capability of a person to walk with maximal independence while spending the shortest time under varied environmental circumstances. Based on this theoretical rationale we hypothesised that there exists a significant correlation between functional strength of lower limb (impairment), sit-tostand (activity) and functional ambulation capacity (participation) in stroke patients. This study aimed to establish clinical evidence for the theoretical construct regarding the above three components as interlinking domains across the ICF continuum in the context of functional ambulation in patients with stroke and to determine whether such derived measurement is consistent with estimates obtained from well-known clinical assessment instruments which purport to measure the same constructs. Figure 2 depicts our research question when structured into the framework of ICF.
Methodology
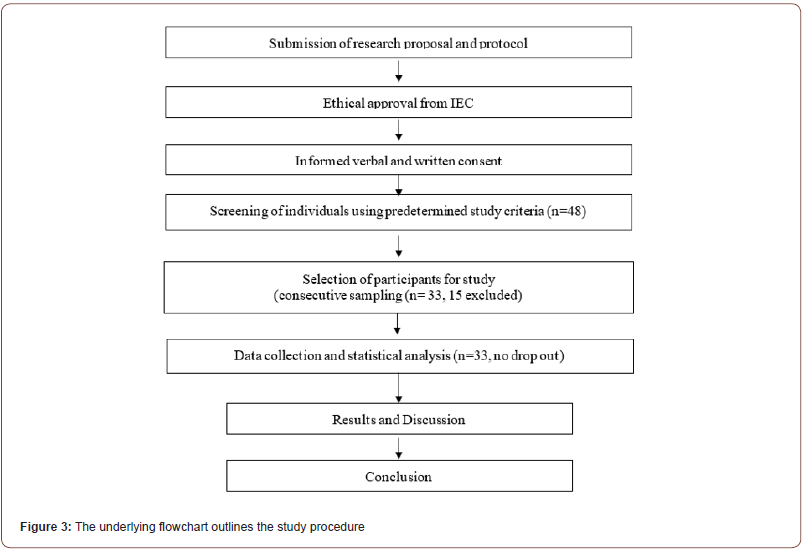
This was a cross-sectional observational study conducted in the physiotherapy department of a tertiary care hospital over a period of 18 months. Ethical approval was taken from the institutional review board of K J Somaiya College of Physiotherapy. A convenient sample of stroke patients visiting the centre for Physiotherapy who were discharged from the inpatient rehabilitation and living in the community (not-institutionalised) was the target population. They were invited to participate and were recruited in the study after a baseline screening assessment as per the study’s predetermined eligibility criteria. A sample size of 33 was calculated statistically following a pilot study. The participation in the study was voluntary and the participants had the right to withdraw from the project for any reason (or no reason at all), at any time, without penalty of any sort or loss of benefit to which he/she would otherwise be entitled. The data collected on the participant to the point of withdrawal remained part of the study database. Individuals with stroke (n=33) having unilateral hemiplegia in the age group 18-60 years of either gender with an ability to follow at least 3 unrelated commands (MMSE score >24/26) [17]; ability to maintain standing for more than 10 seconds; an ability to perform sit-to-stand without physical assistance were included. The exclusion criteria set was patients having any neuromuscular condition other than stroke, major sensory deficits in lower limbs (Fugl-Meyer lower extremity scale sensory component score- 6-12); uncorrected visual or hearing impairments; vestibular dysfunction; any musculoskeletal condition which might affect balance and mobility, non-stroke related disabilities; or patients who were medically unstable. The underlying flowchart (Figure 3) outlines the study procedure (Figure 3).
Outcome measures assessed in the study are as follows.
1. Functional strength: Stroke being a lesion of the central nervous system, measurement of strength by manual muscle testing and dynamometry may prove to be insufficient. The Upright Motor control test (UMCT) was developed by Rancho Los Amigos in 1984 as a measure of voluntary control and functional strength of hemiparetic lower limb in standing position in patients with stroke [18]. The very construct of it overcomes the limitations of both manual muscle testing and dynamometry and identifies stroke-specific weakness. UMCT has been designed to incorporate the effects of upright posture and weight bearing and it simulates the activity required for walking. It consists of two major sections: Flexion component: to ascertain flexion control of the non-weightbearing extremity (i.e., for limb advancement- in the swing phase of gait and assessing factor of speed). Extension component: to ascertain the extension control of a single weight-bearing extremity (i.e., assessing joint stability for single-limb stance in gait). Both flexion and extension components have sub-components at hip, knee and ankle graded as 3, 2 or 1. A total Score 6-18 is thus reflective of total voluntary control of the lower limb, and higher the score better is the control. The UMCT may also successfully capture the ability of patients to accept load on the more affected lower extremity, which is an important dimension of sit‐ to‐stand performance, thus further justifying its use in our study context.
Measurement properties of the UMCT for adults with stroke have been well established. The inter-rater reliability is substantial for both UMCT- Knee flexion component (UMCT-KF) and UMCTKnee Extension (UMCT-KE) as 0.63-0.67, 95% CI and, inter-tester reliability: flexion component: 96%; extension component: 90%. The test-retest reliability- substantial to almost perfect for all components was 0.75-0.82,95% CI and its sensitivity and specificity placed at 98%, 67% respectively. The criterion validity showed 78% accuracy, 78% agreement and it was easy to administer [18]. A recent systematic review has reported its clinical utility and practical advantages too. A recent systematic review (2016) has reported its clinical utility and practical advantages too (4). After this review, more research studies were conducted (in 2017, 2019) to test the psychometric properties of UMCT which showed that UMCT has moderate accuracy and is a valid method of assessing voluntary total limb control in standing [18]. UMCT is consistent with well-established clinical instrument tools, some of which are objective too. UMCT subtest of the knee can predict walking ability. Substantial number of studies have used UMCT as an assessment tool.
As per the original description, the test is performed with the assistance of the therapist. All the studies which have used UMCT have provided manual assistance to the patient (figures in some of the studies show assistance provided by two people too). Assistance is provided to substitute for the impaired balance ability and not to substitute for the impaired movement control function of the paretic lower limb. It was provided at a distant body part and not directly at any part of the lower extremity.
The amount of assistance to be given is not specified in the description of UMCT. In our study, minimal assistance was provided by the therapist. As per the definition given in FIM, Minimal (contact) assistance (FIM 4) is ‘Patient requires small amount of help to accomplish activity; patient requires no more help than touching and expends 75% or more of the effort. Patient is able to assume all of his body weight, but requires guidance for initiation, balance, and/or stability during the activity.’ Minimal assistance as defined here was used for assessment of UMCT. This operational definition was used to add to the uniformity of the assessment procedure and standardization of the data. The distance between the therapist and patient while performing the test was approximately an arm length apart so that the patient does not lean forward excessively and at the same time tries to maintain the trunk erect by himself/ herself (as required for hip extension control subtest of UMCT). Thus, the assistance was provided to support the patient for body imbalance and at a distant body part and not directly at any part of the lower extremity. Scoring criteria is descriptive (uses an ordinal scale) and qualitative differences in terms of performance of movement control are graded accordingly. While assigning a score, the movement of the specified part or the adjacent body part (e.g. trunk for assessing hip control) are the focus. Thus, lack of movement control (irrespective of the manual assistance provided) could be sensitively identified by the assessor.
2. Sit-to-stand (STS): STS performance was assessed on NeuroCom© Balance Manager® System (version 8.6.0). The STS assessment quantifies the patient’s ability, on command, to quickly rise from a seated to a standing position. Key components of this task include shifting the body COG forward from an initial position over the seat to a location centered over the base of support, followed by extension of the body to an erect stand while maintaining the centered COG position. The measured parameters were weight transfer time, rising index (force exerted to rise), sway velocity after rising phase, and left/right symmetry of the rising force. It gives a comprehensive report of the parameters as described below.
1. Weight Transfer (in seconds) is the time in seconds required to
voluntarily shift COG forward beginning in the seated position
and ending with full weight bearing on the feet.
2. Rising Index is the amount of force exerted by the legs during
the rising phase. The force is expressed as a percentage of the
patient’s body weight.
3. COP Sway Velocity (degrees/second) documents control of the
COP over the base of support during the rising phase and for
5 seconds thereafter. Sway is expressed in degrees per second.
4. Left/Right Weight Symmetry (percentage of body weight)
documents differences in the percentage of body weight borne
by each leg during the active rising phase.
In the test, the participant was asked to sit in front of the monitor screen on a stool with arms on thighs, hip-knees in flexion, both feet completely supported on the ground. The participant was explained the task and a video of the same was shown on the screen. The participant was then asked to perform the test with three repetitions following the instructions on the screen. On seeing the prompt GO on the screen, he/she performed the STS movement and maintained the final position for 5 seconds. All the assessment protocols are consistent with the WHO ICF and have been validated by extensive scientific & clinical research. The inter-rater and testretest reliabilities were reported high (0.967, 0.858 respectively) with intra- class correlation coefficient; 95% CI [19].
3. Functional ambulation: Ambulation classification, originally given by Hoffer, modified and further expanded by Perry et al (1995) is used to categorize patients into six ambulatory capacities using descriptive criteria based on their abilities. This classification system has been critically modified by experts to reflect the threshold levels of performance. Each patient is assigned to one category according to these criteria. These six categories include physiological walker, limited household walker, unlimited household walker, most limited community walker, least limited community walker, and community walker. From the literature search conducted for the present study, it is evident that Perry’s classification is the most appropriate amongst all the functional ambulation measures available. Each level in the classification is self-explanatory and that there are minimal or no chances of mistakes in assigning a level to the patient.
For the present study, the patient’s gait was examined and certain data were obtained by questioning the subject regarding the level of functional walking ability at home and in the community. The degree of walking independence, agility, and safety was assessed, as was information obtained directly from both patients and their relatives. Attention was given especially to the patient’s ability to deal with different surroundings. Only the patient’s usual walking level was considered, not the level he/she could potentially achieve. Patients in each higher category performed all activities of the previous group as well as the additional level of challenge listed.
Walking ability included the management of three variables (i) Changes in level and terrain irregularity, (ii) obstacle avoidance, and (iii) increase in distance. These variables are encountered during ambulation in the community and thus justify our inclusion of this classification/scale for assessing functional ambulation in a broader sense. FWC considers walking dysfunction post stroke as a social handicap. Thus, we can consider it to reflect it as a participation restriction in the ICF classification. The psychometrics properties of FWC are well established in the literature. Its predictive validity is AUC – 89%, sensitivity- 100%; specificity – 78%, test- retest reliability being 0.950; and inter-rater reliability 0.905 [20].
All the three outcome measures related assessments were performed in a random order, on the same day with sufficient rest given between tests to avoid fatigue. The participants were assessed and scored by a single therapist and in an identical manner. Data analysis: The data was analysed using Graph Pad software version 8.4.3. Descriptive statistics using mean and standard deviations for the quantitative variables and percentage frequencies for the categorical variables were calculated. Correlational analysis was done between UMCT and STS; STS & FWC; and UMCT and FWC. As the data type was ordinal, a non-parametric test (Spearman’s rank correlation test) was used. P value less than 0.05 was considered statistically significant for all the analyses. The demographic variables of the participants are as shown in table 1. The data analysis obtained was then represented on multiple scatter plots.
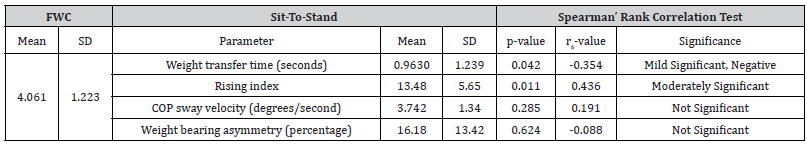
The results of analysis (Table 2) show that there is a mild significant correlation between UMCT score and weight bearing asymmetry during STS; significant, negative, moderate correlation between STS and FWC and a significant positive, high correlation between UMCT score and FWC (Table 1-4).
Table 1: Demographic characteristics of the participants.
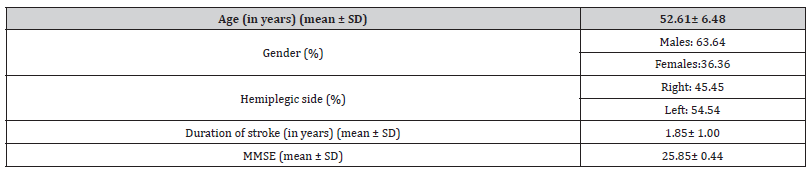
Table 2: Correlation between UMCT and Sit-to-stand.
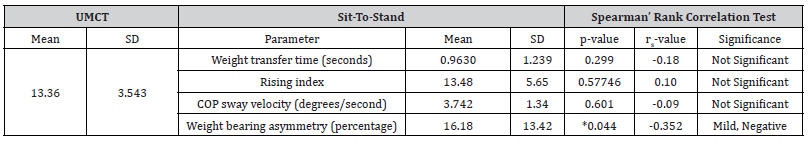
Table 3: Correlation between sit-to-stand and functional walking category.
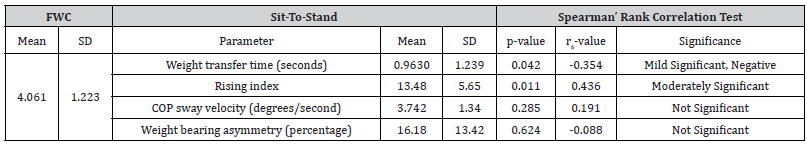
Table 4: Correlation analysis of the UMCT with functional walking category.
Discussion
This study aimed to determine the correlation between functional strength of lower limb, sit-to-stand and functional ambulation capacity in individuals diagnosed with stroke as assessed using Upright Motor Control Test, Sit-to-Stand and Functional Walking Category respectively. This study categorised Upright Motor Control Test, Sit to Stand and Functional Walking Category under the headings of impairment, activities and participation respectively in the ICF format. UMCT tested the functional strength of the paretic lower limb in 6 component tests and a total score was obtained. The UMCT score was 13.36 ± 3.543 (mean ± SD) out of a total 18 which demonstrated that the voluntary muscle activation was moderately affected in the paretic lower limb causing impaired functional performance in patients after stroke. This finding can be attributed to the inappropriate recruitment and timing of their activation (Kooistra et al., 2007), or damage to the descending motor tracts following stroke (Ward, 2004). It could also be because of impaired neural control (Newham & Hsiao, 2001), decreased number and firing rates of motor units (Di Fabio and Badke, 1991), or atrophy of type II muscle fibres and fatigue (Collin and Wade, 1990).
The sit-to-stand (STS) movement can be described as biomechanically demanding, and requiring more lower extremity joint torque and range of motion than walking or stair climbing [21]. Weight-transfer time of the sit to stand task, indicated by time taken by movement of the centre of pressure or centre of mass during voluntary weight shifts in a standing position to attain stability, has been proven to relate to various measures of standing balance and gait [22]. Though STS is a major focus of rehabilitation training for patients with hemiparesis, very few studies have focused specifically on this component [23]. For the purpose of this study we have considered the weight transfer time component of the Sit to Stand task as our out-come measure.
The participants were categorised into one of the six components according to FWC classification on observing the patient in their environment and getting a judgement on their capacity to adapt to their surroundings (ability to negotiate obstacles and move over different terrains functional ambulation performance).
1. Correlation Analysis Between Upright Motor Control Test and Sit to Stand test:
The results found that there was significant correlation between UMCT and weight bearing asymmetry parameter of STS activity in stroke patients (p=0.04, rs=-0.3). No significant correlation was observed with other parameters of STS movement in stroke patients. This finding was supported by a study done in 2004 stating paretic hip extension strength did not relate to STS performance in Stroke patients [24]. Another study conducted by Bohannon [25] explained that any increase in strength will not prove useful until a threshold is reached. Only after that threshold is crossed, improvement in performance at the functional activity is seen. As functional activities place different demands on individuals, the point at which strength begins to affect the activity performance varies accordingly. This could be a probable reason why this study found no relationship between the two components.
In our study, we focused on the kinematic variables of the whole affected limb as opposed to the kinetic variables like joint/ muscle torques of individual muscles and did not take the timing of muscle fibre firing into account.
Another factor contributing to the results of this analysis could also be the discrepancy in the recovery rate of strength required for UMCT and motor control required to perform the STS task. A recent study has shown that the strength recovers at a faster rate than motor control in individuals with stroke and hypothesised that recovery of these two components could occur in parallel as a result of similar tissue repair mechanisms post stroke, but they can be construed as independent modules [26].
Stroke also affects the central regulation of an individual along with motor coordination which alters the relationship between strength and activities like sit to stand as compared to normal individuals, which could explain the results of our study [27]. It has also been found that sit to stand performance is also influenced by multiple sensorimotor, balance, and psychological processes and represents a particular transfer skill with strength contributing to only a part of it [28].
These results also provide a perspective supporting taskoriented movement rehabilitation as opposed to targeting singular impairments when mapping out a rehabilitation programme.
2. Correlation Analysis between Sit to Stand and Functional Walking Category:
We found that there exists a moderate negative significant correlation between the STS and FWC (p <0.05, r= -0.3550). The findings suggested an inverse relationship between the two concurring that better the person’s functional ambulation capacity, lesser is the time required to attain stable weight bearing on both legs from the sitting position. Studies have shown that chronic hemiparetic subjects with different levels of functional performance differ in parameters related to balance during the sit-to-stand movement assessed by the Balance Master [29,30]. Pinheiro et al in 2019 conducted a study that concluded that chronic hemiparetic individuals having low functional performance levels (household ambulation) took more time to perform sit to stand with less weight transfer on both lower limbs which aligns with the results of our study [29].
Previous studies show significant negative correlation between sit to stand and gait velocity [31] and there is literature stating that sit to stand can be considered a valid measure to predict community ambulation of stroke patients [32]. Both of these align with the findings of our study showing a relationship between sit to stand functional ambulation in stroke patients and infer that training one aspect may show effect on the ambulatory capacity of an individual affected by stroke.
3. Correlation analysis between Upright Motor Control Test and Functional Walking Category:
There was a significant, high, positive correlation between FWC and UMCT (p<0.0001, r=0.6474). We inferred that functional strength of the lower limb has a direct relationship with the ambulation level of a stroke individual.
Our findings indicated that muscle strength and walking distance are contributing factors in community ambulation for patients with chronic stroke. There is research present that states muscle strength as one of the major components responsible for functional ambulation in stroke patients. Daniellson et al. conducted a study comparing physical activity in stroke population with a control group and they found a low association between strength and FWC. They concluded that there were multiple factors responsible for improving functional ambulation in stroke patients and a multidisciplinary program is always needed [33]. This reasoning supports the findings of our study.
A previous study examined the relationship between isometric paretic lower limb muscle strength and the tasks of gait ability, balance and motor skills in hemiparetic patients. The study found none of the muscle groups’ isometric strength was correlated with gait ability of hemiparetic patients’ in the chronic stage of disease except for hip abductors which indicated a low correlation [34]. Our results dispute these findings and establish a strong relationship between functional strength and FWC
This relationship between UMCT and FWC reinforced the statements made by previous studies that:
1. global strength measured by a single index incorporating all the lower-limb muscles strongly associated with distance walked by an individual with stroke [35]
2. reiterated strength and sensation as two major factors contributing to gait capacity [36] in individuals with stroke.
The positive or negative direct relationship between scores on all these domains, suggests that these tests assess related constructs of the ICF.
It can be inferred that better the functional strength of the individual, better is sit to stand activity and better is the participation in terms of functional ambulation in the society. The results of this component strongly reiterate the findings of previous studies that have individually stated that global strength measured by a single index incorporating all the lower-limb muscles and sit to stand strongly associates with distance walked by an individual with stroke. The findings our study concurred with the findings of a review done in 2007 that stated paretic limb weight-bearing, aerobic, functional strengthening and balance to be critical components to improve walking ability and reiterated that strengthening appears to be most effective when incorporated in functional activities (repetitive sit to stand) to see improvement in the community participation of individuals with stroke [37].
However, we acknowledge several limitations of our study. One limitation of this study was that the study design was cross-sectional; there were no primary and secondary endpoints. Another limitation was that the focus was on ICF items and clinical assessments; details of patient demographic data were not analysed. We did not analyse the data with respect to the dominance, perception, area of affection, type and duration of stroke which could have played a role in the results of the study. As per the study criteria, subjects were required to do sit to stand independently, however, patients with lower functional abilities may exhibit a different phenomenon. A more objective method could have been used to measure functional strength and functional ambulation. Confounding factors, other physical impairments, endurance, cognitive impairments, inter hemispheric differences, etc. are not considered in the analysis.
Conclusion
This study provides evidence of correlation of functional strength of lower limb sit to stand and functional walking category in stroke patients endorsing the importance of ICF model in assessment and rehabilitation programme for stroke patients. The results of this study offer a quantitative method of relating the social disadvantage of stroke patients to the impairment and disability sustained. The ICF plays a vital role in the functioning and health of patients with stroke. In a clinical setting, ICF helps in planning the assessment and treatment procedure. The measurement of therapeutic outcome in relation to the social advantage for the patient would allow more efficient standardization of treatment and services. This study illustrates the potential of building quantitative measurement by aggregating ICF categories and their respective clinical assessments into meaningful domains. Our research has established a link between all the domains of ICF viz. impairments and participation; activity and participation, and between impairment and activity domain using clinical assessment tools. Clinicians should undertake intervention programmes that target all the components (multidisciplinary rehabilitation programmes) mentioned under ICF. Task oriented training along with treatment for impairments will yield positive results in stroke population and improve their participation in society. It can be implied that a strength training program and training the sit-to-stand activity is essential for successful functional ambulation of stroke patients.
Future Implications
This study provides preliminary data for the design and implementation of larger randomized clinical trials and highlights the need for future research. Use of the ICF as an assessment system for stroke rehabilitation patients can be combined with the use of other existing assessment scales and objective assessment tools to gauge functional status more comprehensively. The results of this type of assessment will possess great practical value and can facilitate even more effective rehabilitation. The biopsychosocial model is increasingly believed to be the most rational medical approach and use of the ICF as a stroke assessment framework can better reflect and promote this approach. Further threads of this discussion will prove to be interesting to follow.
Declaration Statements
Acknowledgement: The authors acknowledge the valuable contribution of the participants; and support of the principal and faculty of the institute in the conduct of the study.
Conflict of Interest
The authors declare that there is no conflict of interests
Funding
The authors have not received any kind of financial support in the conduct or publication of this research.
References
- Singla S, Singla R (2016) Stroke in India: Bio-socioeconomic determinants. J Soc Health Diabetes 04(02): 071–6.
- Kamalakannan S, Gudlavalleti ASV, Gudlavalleti VSM, Goenka S, Kuper H (2017) Incidence & prevalence of stroke in India: A systematic review. Indian J Med Res 146(2): 175.
- Pandian JD, Sudhan P (2013) Stroke Epidemiology and Stroke Care Services in India. J Stroke 15(3): 128–34
- Fahey M, Crayton E, Wolfe C, Douiri A (2018) Clinical prediction models for mortality and functional outcome following ischemic stroke: A systematic review and meta-analysis. PLOS ONE 13(1): e0185402.
- Tempest S, McIntyre A (2006) Using the ICF to clarify team roles and demonstrate clinical reasoning in stroke rehabilitation. Disabil Rehabil 28(10): 663-667.
- Zhang T, Liu L, Xie R, et al. (2018) Value of using the international classification of functioning, disability, and health for stroke rehabilitation assessment: A multicenter clinical study. Medicine (Baltimore) 97(42): e12802.
- Silva SM, Corrêa FI, Faria CD, Buchalla CM, Silva PF, et al. (2015). Evaluation of poststroke functionality based on the International Classification of Functioning, Disability, and Health: a proposal for use of assessment tools. J Phys Ther Sci 27(6): 1665-1670.
- Leonardi Matildea, Cerniauskaite Mildab, Quintas Ruib, Ajovalasit Danielab, Raggi, Albertob, Invernizzi Veronicab, Sattin Davideb; Parati Eugenioc, Boncoraglio Giorgioc (2009) Gomez, Jesusc ICF and Stroke: Describing Functioning and Disability, International Journal of Rehabilitation Research: August – 32: S16
- Kossi O, Amanzonwe ER, Thonnard JL, Batcho CS (2020) Applicability of International Classification of Functioning, Disability and Health-based participation measures in stroke survivors in Africa: a systematic review. Int J Rehabil Res 43(1): 3-11.
- Kinoshita Shoji, Abo Masahiro, Okamoto Takatsugu, Kakuda, Wataruc Miyamura, Koheib, Kimura Ikuobe (2017) Responsiveness of the functioning and disability parts of the International Classification of Functioning, Disability, and Health core sets in postacute stroke patients. International Journal of Rehabilitation Research 40(3): 246-253.
- Begum MR, Haque MO (2019) The Use of ICF in Physiotherapy Management for Patient with Ischemic Stroke: A Case Study. J Physiother Rehabil 3: 2.
- Brasure M, Lamberty GJ, Sayer NA, Nelson N, Macdonald R, et al. (2012) Multidisciplinary Post-acute Rehabilitation for Moderate to Severe Traumatic Brain Injury in Adults [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); (Comparative Effectiveness Reviews, No. 72.)
- Hislop H, Montgomery J (2007) Daniels and Worthingham’s Muscle Testing: Techniques of Manual Examination, 8th ed. W.B. Saunders St. Louis.
- Janssen WG, Bussmann HB, Stam HJ (2002) Determinants of the sit-to-stand movement: a review. Physical Therapy 82(9): 866-879.
- Janssen WG (2008) The sit-to-stand movement recovery after stroke and objective assessment, Ph.D. dissertation Erasmus Medical Center Erasmus University Rotterdam The Netherlands.
- Oh D (2013) Community Ambulation: Clinical Criteria for Therapists’ Reasoning and Decision-making in Stroke Rehabilitation. International Jrnl of Physical Med and Rehab 1(4): 2329-9096.
- MMSE guidelines. https://www.ncbi.nlm.nih.gov/projects/gap/cgibin/ GetPdf.cgi?id=phd001525.
- Lunar FRM, Gorgon EJR, Lazaro RT (2017) Clinimetrics of the Upright Motor Control Test in chronic stroke. Brain Behav 7: e00826.
- Mao YR, Wu XQ, Zhao JL, Le L, Xiu QW, et al. (2018) The Crucial Changes of Sit to Stand Phases in Subacute Stroke Survivors Identified by Movement Decomposition Analysis. Front Neurol 9: 185.
- Wagatsuma M, Kim T, Sitagata P, Lee E, Vrongistinos K, et al. (2019) The biomechanical investigation of the relationship between balance and muscular strength in people with chronic stroke: a pilot cross-sectional study. Top Stroke Rehabil 26(3): 173-179.
- Berger RA, Riley PO, Mann RW, Hodge WA (2019) Total body dynamics in ascending stairs and rising from a chair following total knee arthroplasty. Trans Orthop Res Soc 13: 542.
- de Haart M, Geurts AC, Dault MC, Nienhuis B, Duysens J (2005) Restoration of weight shifting capacity in patients with postacute stroke: a rehabilitation cohort study. Arch Phys Med Rehabil 86(4): 755-762.
- Dettmann MA, Linder MT, Sepic SB (1987) Relationships among walking performance, postural stability, and functional assessments of the hemiplegic patient. Am J Phys Med 66: 77-90.
- Lomaglio M, Eng J (2005) Muscle strength and weight-bearing symmetry relate to sit-to-stand performance in individuals with stroke. Gait and Posture 22(2): 126-131.
- Bohannon RW (2007). Muscle strength and muscle training after stroke. J Rehabil Med.; 39(1):14-20. doi:10.2340/16501977-0018
- Xu J, Ejaz N, Hertler B, Widmer M, Kitago T, et al. (2017) Separable systems for recovery of finger strength and control after stroke. J Neurophysiol 118(2): 1151- 1163.
- Geyh S, Cieza A, Schouten J, Dickson H, Frommelt P, et al. (2004) ICF Core Sets for stroke. J Rehabil Med 44: 135-141.
- Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A (2002) Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci 57(8): M539-M543.
- Pinheiro M, Polese JC, Machado G, Scianni AA, Hirochi TC, et al. (2010) Balance analysis during the sit-to-stand movement of chronic hemiparetic individuals based upon their functional levels. Man Ther Posturology Rehabil J 12: 260-264.
- Akulwar IS (2019) Can Quantitative Balance Measures Discriminate between Functional Ambulation Categories in Chronic Stroke Survivors? Physiother Rehabil 4: 178
- Ju S (2020) Correlation between lower limb muscle asymmetry during the sit-to-stand task and spatiotemporal gait asymmetry in subjects with stroke. J Exerc Rehabil 16(1): 64-68.
- Lee G, An S, Lee Y, Park DS (2016) Clinical measures as valid predictors and discriminators of the level of community ambulation of hemiparetic stroke survivors. J Phys Ther Sci 28(8): 2184-2189.
- Danielsson A, Meirelles C, Willen C, Sunnerhagen KS (2014) Physical activity in community-dwelling stroke survivors and a healthy population is not explained by motor function only. PM R 6(2): 139-145.
- Akbari A, Karimi H (2006) The Relationship Between Lower-extremity Muscle Strength and Functional Performance in Hemiparetic Patients. Journal of Medical Sciences 6: 327-331.
- Moriello C, Finch L, Mayo NE (2011) Relationship between muscle strength and functional walking capacity among people with stroke. J Rehabil Res Dev 48(3): 267-275.
- Nadeau S, Arsenault AB, Gravel D, Bourbonnais D (1999) Analysis of the clinical factors determining natural and maximal gait speeds in adults with a stroke. Am J Phys Med Rehabil 78(2): 123-130.
- Eng JJ, Tang PF (2007) Gait training strategies to optimize walking ability in people with stroke: a synthesis of the evidence. Expert Rev Neurother 7(10): 1417-1436.
-
Rucha Gadgil, Isha Akulwar Tajane. Correlation Between Functional Strength of Lower Limb, Sit to Stand and Functional Ambulation Capacity in Stroke Patients: an ICF Perspective. Arch Neurol & Neurosci. 12(4): 2022. ANN.MS.ID.000791. DOI: 10.33552/ANN.2022.12.000791.
-
Stroke, Neuro Physiotherapy, Neurosciences, ICF, Stroke, Upright motor control test, Sit -to-stand, Functional walking category, Impairments, Participation, Activity limitation.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






