 Case Report
Case Report
Rapid Resolution of Carotid Thrombus within Two Hours
Fatima Zahra Bensabeur*, Andrew Joseph Reichard and Esteban Cheng-Ching
Department of Neurology, Boonshoft School of Medicine, Wright State University, USA
Fatima Zahra Bensabeur, Department of Neurology, Boonshoft School of Medicine, Wright state University, USA.
Received Date: August 17, 2022; Published Date: August 30, 2022
Case Report
An 83-year-old male patient with PMHx of hypertension, myelodysplastic syndrome, and hypothyroidism presented to the emergency department with left-sided facial droop, left arm weakness, dysarthria, and right gaze preference. Baseline Modified Rankin Scale (mRS) was 0-1. He had no history of Afib or prior strokes. There was no history of tobacco, illicit drug, or alcohol use. Time of last known well (LKW) was 10:40. On initial presentation at 11:34 the NIHSS was 9. CT head revealed no acute bleed or recent infarct and he was considered a candidate for intravenous thrombolysis. Given his NIHSS and suspicion for large vessel occlusion, the decision was made to administer a thrombolytic drug at 12:02. CTA head-neck demonstrated no intracranial large vessel occlusion (LVO), however, a large partially occlusive thrombus was identified in the right carotid bifurcation. Following intravenous thrombolysis, the patient initially improved to an NIHSS of 5, but at 13:20 worsened clinically with NIHSS increasing to 16. The clinical change was concerning for hemorrhage or migration of thrombus fragments to an intracranial artery. Therefore, CT and CTA were obtained at 13:40 demonstrating no evidence of intracranial large vessel occlusion and complete resolution of the previously visualized carotid thrombus. Given the lack of LVO, the patient was not a candidate for mechanical thrombectomy. The patient improved clinically, with NIHSS of 8 at 15:40, NIHSS of 6 at 22:00, and NIHSS of 5 at 09:00 the next morning.
Brain MRI obtained later demonstrated small acute infarcts involving the right basal ganglia, adjacent deep white matter, and the cortex of the frontal, temporal and parietal lobes. CT head at 24 hours was negative for hemorrhage. On discharge his NIHSS was 4 (1 for dysarthria, 2 for facial palsy, and 1 for partial hemianopsia). At his 1 month follow up he had mild dysarthria but no other focal deficits.
Questions for consideration:
1. What caused the rapid resolution of the carotid thrombus?
2. What dose is currently used in the administration of this
drug?
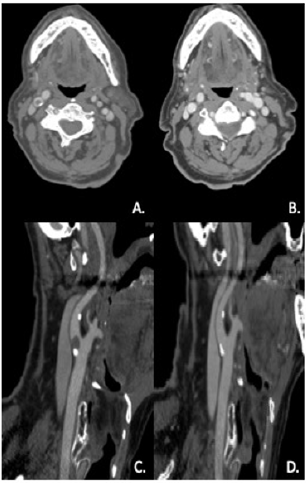
Our patient received tenecteplase (TNK) as an IV bolus of 21mg at 0.25mg/kg x 82.5kg which caused rapid resolution of the carotid thrombus (Figure1). Intravenous TNK leads to rapid thrombolysis in acute ischemic stroke and can be associated with resolution of large carotid intra-arterial thrombus. Intravenous alteplase (tPA) is currently the thrombolytic agent of choice in acute ischemic stroke. However, based on current guidelines it is also reasonable to administer TNK as a single bolus (0.25 mg/kg) instead of alteplase in patients without contraindications for intravenous thrombolysis who are considered eligible for mechanical thrombectomy [1].
An emerging strong body of evidence is revealing the advantages and possible superiority of TNK in reperfusion of large intracranial vessels, however no cases have been reported on the role of TNK in cervical vessel reperfusion [2-5]. Furthermore, the time elapsed from administration of the thrombolytic until thrombus resolution is achieved is not known. This case is the first to show documented resolution of carotid artery thrombus with TNK, with rapid effect achieved within 2 hours of TNK administration (Figure 1).
Figure 1:CTA head-neck prior to tenecteplase administration (A Axial scan and C Sagittal scan at 11:41), and following tenecteplase administration (B Axial scan and D Sagittal scan at 13:40) demonstrating rapid and complete resolution of a large partially occlusive thrombus.
Discussion
We present a case with rapid resolution of a large and partially occlusive carotid thrombus treated with intravenous TNK in an acute ischemic stroke patient. Based on the NINDS tPA trial published in 1995, intravenous alteplase has been the treatment of choice for patients presenting with an acute ischemic stroke [6]. Recently, multiple randomized controlled trials have demonstrated that patients with LVO acute ischemic stroke benefit from mechanical thrombectomy, showing significant improvement in disability and functional outcomes [7-8]. As the principle of arterial recanalization has been correlated with improved outcomes, achieving early recanalization of an occluded vessel in acute ischemic stroke has been the marker of a beneficial therapy [9]. Administering a thrombolytic agent early and in a simpler setting without the need for a lengthy infusion may prove beneficial, and TNK has been studied extensively for this purpose given its characteristics.
Tenecteplase is a genetically modified variant of alteplase with fourteen-fold greater fibrin specificity, ten-fold greater conversion of fibrinogen, eighty-fold greater resistance to the activity of plasminogen activator inhibitor-1 (also known as endothelial plasminogen activator inhibitor or serpin E1), increased speed of thrombolysis, and reduced plasma clearance leading to a longer plasma half-life [10-13]. The fibrin specificity of TNK not only translates into greater potency for thrombolysis, but also helps to preserve the integrity of the systemic coagulation cascade, potentially decreasing the risk of hemorrhage following administration of the medication [11]. This preservation may involve maintaining levels of factor V, fibrinogen, and plasminogen [12]. In addition to the longer duration of action and improved fibrin specificity, TNK is administered as a single intravenous bolus injection and does not require the hour long infusion used in administration of tPA therapy [13].
In the EXTEND-IA TNK trial, TNK was compared with tPA in patients with LVO acute ischemic stroke demonstrating improved reperfusion and functional outcomes [5]. Based on this study, most recent stroke guidelines support the use of this thrombolytic agent in patients who would be candidates for mechanical thrombectomy. At our institution, we have adopted the use of TNK for patients who are suspected to have LVO acute ischemic stroke. Our patient had an initial presentation with symptoms suggestive of LVO acute ischemic stroke and was a candidate for intravenous thrombolysis. Following our protocol for treatment of acute ischemic stroke, TNK was administered and CTA was obtained to determine if mechanical thrombectomy was indicated. While the initial CTA demonstrated no intracranial LVO but a large carotid thrombus, a follow up CTA was obtained within 2 hours given clinical decline, showing no intracranial arterial occlusion and complete resolution of the carotid thrombus in a very rapid fashion (Figure 1). This impressive speed of recanalization has not been previously reported in carotid arterial thrombus. However, reports of intracranial arterial recanalization have been documented after TNK administration. One recent case report discusses administration of tenecteplase 105 minutes after symptom onset in a 90-year-old woman with a right middle cerebral artery (MCA) occlusion confirmed by CTA and CT perfusion and an NIHSS score of 9. The patient was transferred to the angiosuite for thrombectomy 25 minutes after administration of the tenecteplase bolus, but the NIHSS had already decreased to 2 within this interval and angiography with mechanical thrombectomy was cancelled. Transcranial doppler showed right MCA recanalization consistent with the observed clinical improvement and MRI/MRA showed complete recanalization with minimal hyperintensity on DWI and no hypoperfusion [14].
An earlier case report described a 23-year-old woman with an abrupt occlusion of the M1 segment of the right MCA confirmed by MRA and an NIHSS of 12 at the time of tenecteplase bolus administration, 60 minutes after last known well. The patient’s NIHSS decreased to 0 at 2 hours after tenecteplase administration. MRA at 24 hours showed complete recanalization of the previously affected MCA M1 segment, with no signs of ischemia [15]. Our patient had clinical decline following TNK administration, and it is possible that the carotid thrombus diminished in size or fragmented into smaller emboli from the TNK effect, causing transient distal embolization and explaining his neurologic symptoms. However, his continued improvement and absence of arterial occlusions on follow-up CTA suggest that TNK’s effect on these emboli continued until complete lysis had occurred, leading to neurologic improvement, and preventing the need for mechanical thrombectomy.
Conclusion
To the best of our knowledge this is the first case report of carotid recanalization with TNK, with documented rapid resolution of the carotid thrombus and associated neurologic improvement, preventing the need for other acute therapeutic interventions.
Acknowledgement
None.
Conflict of Interest
No Conflict of interest.
References
- Powers WJ, Rabinstein AA, Ackerson T, Opeolu M Adeoye, Nicholas C Bambakidis, et al. (2019) Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke. Stroke 50(12): e344-e418.
- Xu N, Chen Z, Zhao C, Tao Xue, Xin Wu, et al. (2018) Different doses of tenecteplase vs alteplase in thrombolysis therapy of acute ischemic stroke: evidence from randomized controlled trials. Drug Des Devel Ther 12: 2071-2084.
- Kheiri B, Osman M, Abdalla A, Tarek Haykal, Sahar Ahmed, et al. (2018) Tenecteplase versus alteplase for management of acute ischemic stroke: a pairwise and network meta-analysis of randomized clinical trials. J Thromb Thrombolysis 46(4): 440-450.
- Huang X, Cheripelli BK, Lloyd SM, Dheeraj Kalladka, Fiona Catherine Moreton, et al. (2015) Alteplase versus tenecteplase for thrombolysis after ischaemic stroke (ATTEST): a phase 2, randomised, open-label, blinded endpoint study. Lancet Neurol 14(4): 368-376.
- Campbell BC V, Mitchell PJ, Churilov L, , Nawaf Yassi, Timothy J Kleinig, et al. (2018) Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke. N Engl J Med 378(17): 1573-1582.
- National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333(24):1581-1587.
- Siegler JE, Jovin TG (2020) Thrombolysis Before Thrombectomy in Acute Large Vessel Occlusion: a Risk/Benefit Assessment and Review of the Evidence. Curr Treat Options Neurol 22(8): 22.
- Campbell BC V, Mitchell PJ, Churilov L, Nawaf Yassi, Timothy J Kleinig, et al. (2020) Effect of Intravenous Tenecteplase Dose on Cerebral Reperfusion Before Thrombectomy in Patients with Large Vessel Occlusion Ischemic Stroke: The EXTEND-IA TNK Part 2 Randomized Clinical Trial. JAMA 323(13): 1257-1265.
- Rha JH, Saver JL (2007) The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38(3): 967-973.
- Van de Werf FJ (1999) The ideal fibrinolytic: can drug design improve clinical results? Eur Heart J 20(20): 1452-1458.
- Sakharov D V, Barrertt-Bergshoeff M, Hekkenberg RT, Rijken DC (1999) Fibrin-specificity of a plasminogen activator affects the efficiency of fibrinolysis and responsiveness to ultrasound: comparison of nine plasminogen activators in vitro. Thromb Haemost 81(4): 605-612.
- Huang X, Moreton FC, Kalladka D, Bharath Kumar Cheripelli, Rachael MacIsaac, et al. (2015) Coagulation and Fibrinolytic Activity of Tenecteplase and Alteplase in Acute Ischemic Stroke. Stroke 46(12): 3543-3546.
- Tanswell P, Modi N, Combs D, Danays T (2002) Pharmacokinetics and pharmacodynamics of tenecteplase in fibrinolytic therapy of acute myocardial infarction. Clin Pharmacokinet 41(15): 1229-1245.
- Psychogios K, Kargiotis O, Safouris A, Georgios Magoufis, Georgios Liakakis, et al. (2019) Tenecteplase Averting Mechanical Thrombectomy in Emergent Large Vessel Occlusion. Neurologist 24(6): 180-182.
- Meenakshi-Sundaram S, Periakaruppan A, Karuppiah SNKP, Karthik SN, Roopakumar L, Thembavani I (2013) Complete recovery following intra-arterial tenecteplase administration in a woman with acute ischemic stroke. J Clin Neurosci 20(12): 1786-1788.
-
Fatima Zahra Bensabeur*, Andrew Joseph Reichard and Esteban Cheng-Ching. Rapid Resolution of Carotid Thrombus within Two Hours. Arch Neurol & Neurosci. 13(1): 2022. ANN.MS.ID.000803.
-
Carotid Thrombus, Hypertension, Myelodysplastic Syndrome, Hypothyroidism, Weakness, Dysarthria, Hemianopsia, Ischemic Stroke.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






