 Case Report
Case Report
Ventricular Tachycardia Following Mannitol-Induced Hyperkalemia :A Case Report and Literature Review
Masad Ilyass1*, Abouelalaa Khalil1, Elwali Abderrahmane1, Doghmi Naoufal1, Bait abdelouahed1 and Bensghir Mustapha2
1Department of Anesthesiology and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Rabat, Morocco
2Department of Anesthesiology And Intensive Care, head of anesthesiology of The Mohamed V Military Training Hospital, Faculty of Medicine And Pharmacy of Rabat, Mohammed V University, Rabat, Morocco
MASAD Ilyass, Department of Anesthesiology and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Rabat, Morocco
Received Date: December 19, 2022; Published Date: February 20, 2023
Abstract
Diagnosis of Cardiac arrest in the operating room is relatively simple compared to other situations, as the majority of patients are closely monitored. Anesthetists and neurosurgeons should be aware that fatal arrhythmia can occur due to mannitol-induced hyperkalemia. We report a case of cardiac arrest type ventricular tachycardia on hyperkalemia induced by infusion of mannitol. Evidence is rare when dealing with cardiac arrest in neurosurgery, and more efforts are needed in understanding the etiologies, mechanisms and the specificities of its management.
Keywords: Ventricular tachycardia ; Hyperkalemia ; Cardiac arrest ; Neurosurgery
Introduction
Cardiac complications including Ventricular Tachycardia, Ventricular Fibrillation Pulseless Electrical Activity and Asystole during neurosurgery are rare but dreadful events. Diagnosis of Cardiac arrest in the operating room is relatively simple compared to other situations, as the majority of patients are closely monitored. Anesthetists and neurosurgeons should be aware that fatal arrhythmia can occur due to mannitol-induced hyperkalemia. We report a case of cardiac arrest type ventricular tachycardia on hyperkalemia induced by infusion of mannitol.
Case Report
A 58-year-old woman, 165 cm tall and weighing 78 kg, was suffering from headache and seizures for 4 months. Diagnosis confirmed a right temporal lobe glioma. She was then scheduled for craniotomy and tumor resection under general anesthesia. The patient had a medical history of hypertension treated by calcium channel blockers; she was also under sodium valproate for the seizures.
The preoperative checkup did not diagnose any problem, in particular the preoperative ECG and the other laboratory tests, blood ionogram, the renal function, the glycemia were all normal.
On admission to the operating room, the patient’s hemodynamic status wasstable. Anesthesia was induced with Propofol (100 mg) and fentanyl (200 μg/), and for intubation rocuronium was added (50 mg). The anesthesia was maintained with sevoflurane (1.2- 1.5%). Twenty five (25) minutes after the surgical incision, 200 ml of 20% mannitol (40 g) was administered intravenously over 60 min. Approximately 20 min after the end of mannitol administration, a Ventricular Tachycardia occurred (Figure 1).
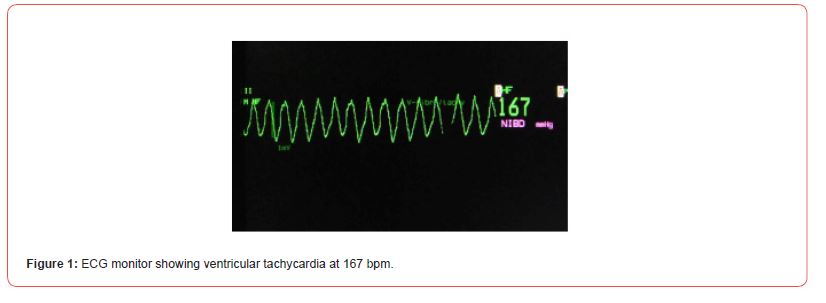
At this time, in the operative field, the arachnoid membrane of the Sylvian fissure was separated. Blood pressure decreased to <40 mmHg. We immediately started the chest compression, and the VT recovered to sinus rhythm at a rate of 75 bpm approximately 20 s after the start of the chest compressions. After recovery of sinus rhythm, ECG did not show noticeable abnormalities. Analysisof arterial blood gases showed pH 7.38, PaCO2 of 40 mmHg, PaO2 of 350 mmHg, ionogram revealed hyperkalemia of 5.5 mmol/L.
The glucose serum was administered with 10 units of insulin. The control value of kalemia was 3.6 mmol/L. Tumor resection was performed without any further incident nor hemodynamic instability. At the end of the operation, no abnormalities were described in the ECG and laboratory tests. The duration of the surgical intervention was 4 h 20 min the estimated blood loss during the operation was 300 ml.
The urine output was 2000 ml. The patient had no other postoperative event and was admitted to intensive care for postoperative care. The patient was extubated after full recovery.
Discussion
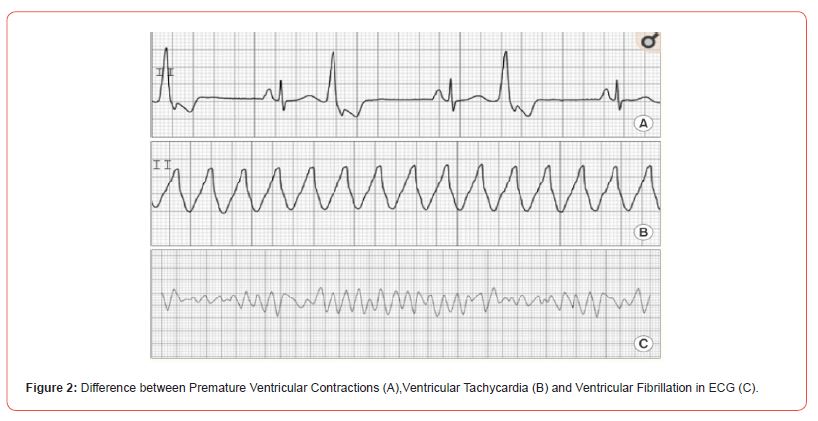
There are a few reports of fatal arrhythmia, Ventricular Tachycardia and / or ventricular fibrillation (Figure 2) due to mannitol,which are mainly due to hyperkalemia [1,2]. The ECG is then the main tool to predict the event on the appearance of arrhythmias.
Mannitol is widely used to reduce intracranial pressure due to increased osmolality of plasma. However, it has several side effects including osmotic nephrosis and electrolyte disorders [3]. Rapid infusion of mannitol may cause hyponatremia or hyperkalaemia. Hyponatremia is mainly due to transient dilution. During mannitolinduced hyperkalemia, intracellular potassium (K) is released into the extracellular space due to an acute increase in plasma osmolality, rhabdomyolysis, hemolysis, and acidosis. In this case, preoperative renal function was normal and there was no evidence of acidosis, rhabdomyolysis or hemolysis. The frequency of mannitol-induced hyperkalemia is 7.7%, and the total dose of mannitol as well as its rate of infusion and decreased renal function may have a role in the development of mannitol induced hyperkalemia [4]. We used a total dose of 40 g of mannitol, which was the recommended dose (0.25-1 g/kg) [5], And the infusion rate was 60 minutes, which was not rapid. In most of the published cases, the change in the ECG - elevation of T waves - was the main finding.
All cases of lethal arrhythmia reported so far have been preceded by a change in the ECG, including elevated T waves and a wide QRS complex. However, no prior ECG changes were observed in our patient, and even after returning to sinus rhythm after VT. Regarding ECG changes in hyperkalemia, such as elevation of T wave (temporary T wave), decrease of P wave, prolongation of PQ interval due to an increase in the kaleemia the extension of the width of the QRS, the disappearance of the P wave and its subsequent increase which leads to an unclear distinction between the QRS and T waves, leading to the cessation of activity cardiac mechanics [6].
However, an ECG without any abnormalities consistent with hyperkalemia is noted in more than 50% of patients with a K> 6.5 mmol/L, and cases of arrhythmia and cardiac arrest have been reported in patients with of hyperkalaemia without ample T wave [7,8].
Ventricular tachycardia should be quickly detected by the anesthetist on the ECG Cardioscope and propose the adequate protocole. The immediate task is to correct any reversible etiology that can include (Hypotension, Hypoxemia, Acidosis and other electrolyte imbalances, Surgical stimulation, light anesthesia) then to propose rapid defibrillation. Concerning pharmacological interventions, AHA recommends the use of Amiodarone or Lidocaine in Ventricular tachycardia and Ventricular Fibrillation resistant to defibrillation [9].
Conclusion
In our case It is not clear why the VT occurred, but in addition to the transient elevation of potassium and mannitol, the craniotomy itself may have influenced it. Evidence is rare when dealing with cardiac arrest in neurosurgery, and more efforts are needed in understanding the etiologies, mechanisms and the specificities of its management.
References
- Akira Gohara, Sumi Okamatsu-Kifuji, Shinjiro Shono, Midoriko Higashi, Ken Yamaura, et al. (2021) Ventricular tachycardia without preceding electrocardiogram change after hypertonic mannitol administration: a case report.
- Flynn BC (2007) Hyperkalemic cardiac arrest with hypertonic mannitol infusion: the strong ion difference revisited. Anesth Analg. 104(1): 225-226.
- Nomani AZ, Nabi Z, Rashid H, Janjua J, Nomani H, Majeed A, et al., (2014) Osmotic nephrosis with mannitol: review article. Ren Fail 36(7):1169-1176.
- Fanous AA, Tick RC, Gu EY, Fenstermaker RA (2016) Life-Threatening Mannitol-Induced Hyperkalemia in Neurosurgical Patients. World Neurosurg. 2016 Jul;91:672.e5-e9.
- Sorani MD, Manley GT (2008) Dose-response relationship of mannitol and intracranial pressure: a metaanalysis. J Neurosurg 108(1): 80-87.
- Mattu A, Brady WJ, Robinson DA (2000) Electrocardiographic manifestations of hyperkalemia. Am J Emerg Med 18(6): 721-729.
- Montague BT, Ouellette JR, Buller GK (2008) Retrospective review of the frequency of ECG changes in hyperkalemia. Clin J Am Soc Nephrol CJASN 3(2): 324-330.
- Durfey N, Lehnhof B, Bergeson A, Durfey SNM, Leytin V, McAteer K, et al., (2017) Severe Hyperkalemia: Can the Electrocardiogram Risk Stratify for Short-term Adverse Events? West J Emerg Med 18(5):963-671.
- (2018) American Heart Association Focused Update on Advanced Cardiovascular Life Support Use of Antiarrhythmic Drugs During andImmediately After Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary esuscitation and Emergency Cardiovascular Care.
-
Masad Ilyass*, Abouelalaa Khalil, Elwali Abderrahmane, Doghmi Naoufal, Bait abdelouahed and Bensghir Mustapha. Ventricular Tachycardia Following Mannitol-Induced Hyperkalemia :A Case Report and Literature Review. Arch Clin Case Stud. 3(3): 2023. ACCS.MS.ID.000563.
-
Infusion of mannitol, Sodium valproate, Blood ionogram, Arrhythmia
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






