 Case Report
Case Report
Necrotizing Pancreatitis, an unusual presentation of longstanding Primary Hyperparathyroidism
F Sumrein and M Raghuwanshi*
Department of Endocrinology, Rutgers New Jersey Medical School, USA
M Raghuwanshi, Department of Endocrinology, Associate Professor of Medicine, Rutgers New Jersey Medical School, USA.
Received Date: March 21, 2019; Published Date: March 29, 2019
Introduction
Acute Necrotizing pancreatitis can be a rare, but first presentation of longstanding primary hyperparathyroidism. Acute pancreatitis was first described as a rare complication of Primary Hyperparathyroidism in the Annals of Surgery by Cope et al. in 1957, with an incidence rate of pancreatitis of 1.5 % - 7%. We present an interesting case of long-standing primary hyperparathyroidism presenting initially as necrotizing pancreatitis complicated by severe hypocalcaemia in a young woman secondary to hungry bone syndrome after a parathyroidectomy.
Clinical Case
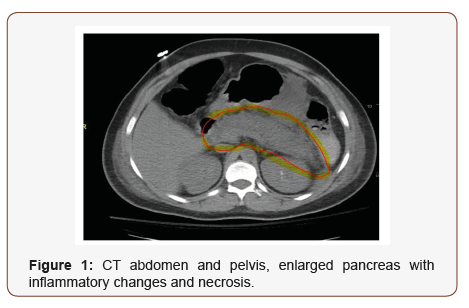
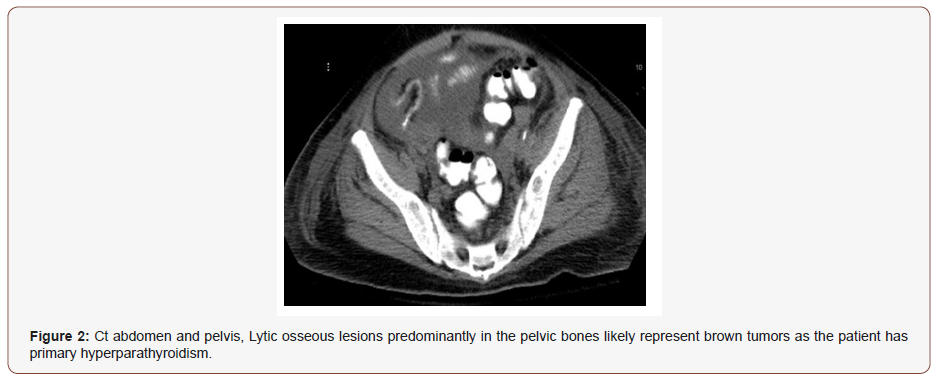
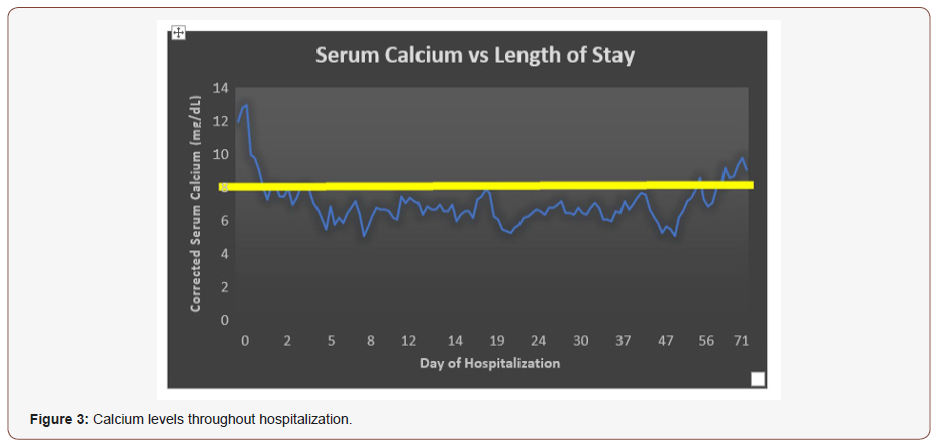
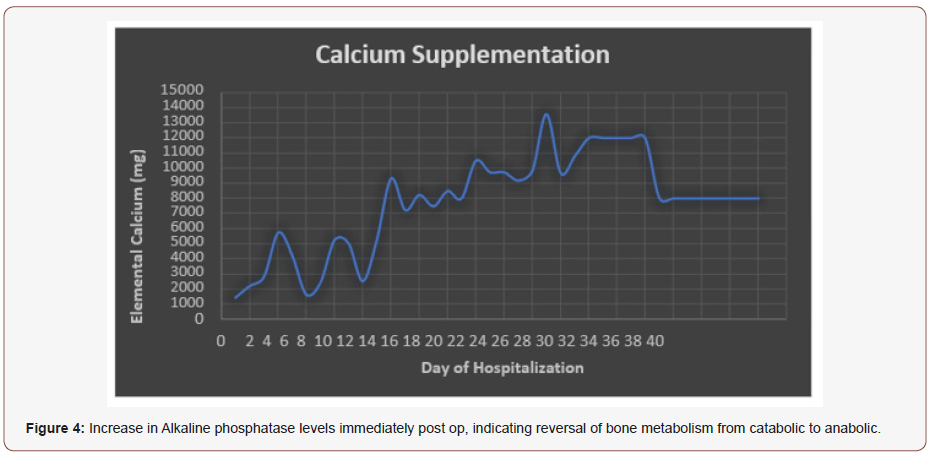
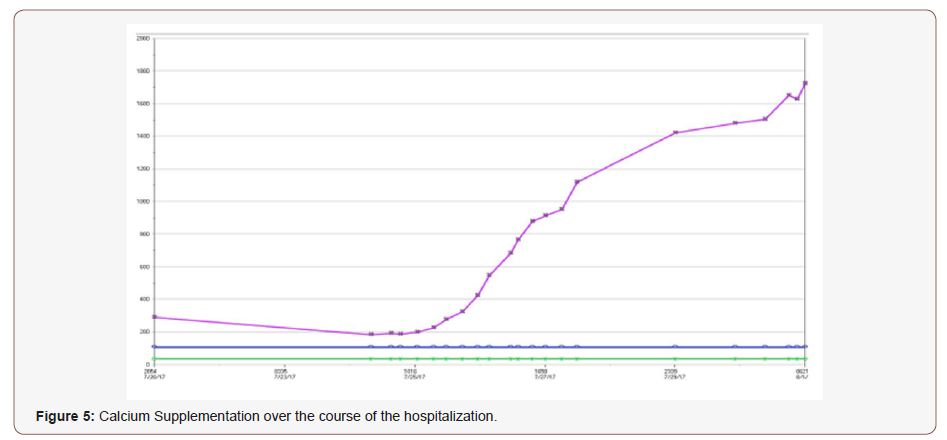
A 38-year-old woman with no past medical history presented with a syncopal episode. A few days prior to the syncopal event, she reported severe abdominal pain and intractable vomiting. These symptoms were a progression of abdominal pain she had experienced for the past 2 months, associated with myalgia and arthralgia. On clinical exam, she appeared in painful distress with epigastric tenderness and voluntary guarding, but no rebounding. On laboratory and imaging studies, she was noted to have severe hypercalcemia of 18mg/dL (n 8.4-10.2mg/dL), intact PTH-1200 pg/mL (n 15-65pg/mL), with initial imaging revealing necrotizing pancreatitis as demonstrated in (Figure 1). On review of previous hospital records, she had hypercalcemia of 13.1 mg/dl dating back to 2003 but was lost to follow up. Based on these clinical findings she was diagnosed with acute necrotizing pancreatitis and started on broad spectrum antibiotics, IV fluids, and taken to the OR emergently for pancreatic debridement. The operative report noted an infected pancreatic necrosis in lesser sac and omental saponification. Due to the patient’s significant abdominal pain post-operatively, she had a repeat CT scan of the abdomen and pelvis with contrast revealing pancreatic drain in the appropriate location and lytic osseous lesions predominantly in the pelvic bones likely representing brown tumors as shown in (Figure 2) [1- 3]. On physical exam patient was noted to have left sided neck mass, which on neck US showed left inferior parathyroid nodule. Due to hypercalcemia, exacerbating the necrotizing pancreatitis, she was taken to the OR for a left parathyroidectomy with a post-operative PTH level of 4 pg/mL. Intra-operatively, the patient was found to have a large left inferior parathyroid gland without any evidence for parathyroid tissue beyond the confines of the gland with pathology demonstrating a hyper cellular parathyroid gland weighing 9 grams and measuring 3.9 x 2.5 x 2 cm. Her calcium levels dropped post operatively within 12 hrs decreasing to as low as 5.9 mg/ dL and remained low throughout her hospitalization as indicated by (Figure 3), associated with symptoms such as Chvostek’s sign, perioral numbness, and muscle spasms. She was also noted to have a significant increase in alkaline phosphatase levels post-operatively, seen in (Figure 4). She was started on Calcium gluconate IV drip and pushes, due to her inability to take oral supplementation due to the pancreatitis. After one-week post op, she was able to tolerate oral medications started on Calcium Carbonate po in addition to the Calcium gluconate IV, as well as Calcitriol 0.5 mg twice daily a. On average, she required about 8 grams of elemental calcium daily, both IV and oral for about 6 weeks post operatively as indicated by (Figure 5). She was discharged on calcitriol and oral calcium supplementation to maintained Calcium levels of greater than 8 mg/dl, after about a 3-month hospitalization [4-6].
Discussion
Hypercalcemia secondary to primary hyperparathyroidism can cause many complications. In our case, we observed severe hypercalcemia leading to severe bone disease and acute necrotizing pancreatitis. Although a rare finding in asymptomatic hypercalcemia, with more serve elevations of calcium there are reported cases of pancreatitis associated with long-standing primary hyperparathyroidism. One of the suspected mechanisms is due to elevations of calcium in the pancreatic fluid leading to activation of trypsinogen within the pancreas causing autodigestion. Another mechanism causing pancreatitis would be the deposition of calcium in pancreatic ducts leading to obstruction. Pancreatitis can also present with low or normal serum calcium, as pancreatic saponification and calcium binding lowers serum calcium.
She also had very severe bone disease due to prolonged untreated hypercalcemia. Post operatively, she had prolonged symptomatic hypocalcemia, that required prolonged supplementation of Calcium, despite recovery of PTH levels to 83 pg./ml. In patients with prolonged primary hyperparathyroidism, they develop severe bone disease to maintain elevated serum calcium levels, known as brown tumors, which are areas of high bone turn over. Immediate reduction in parathyroid hormone causing a reversal of bone metabolism from catabolic to anabolic. This leads to a major influx of calcium into bone. Hypomagnesaemia and hypophosphatemia are also commonly seen. This is known as hungry Bone syndrome, characterized by severe prolonged hypocalcemia, seen in patients with primary hyperparathyroidism undergoing parathyroid excision surgery. Severe hypocalcemia can cause serious complications tetany, convulsions, laryngeal spasm, and myocardial dysfunction. Close monitoring of patient’s calcium levels is required post parathyroidectomies [7-9].
Conclusion
Necrotizing pancreatitis can be the first manifestation of primary hyperparathyroidism. Longstanding Primary Hyperparathyroidism can present with more severe hypercalcemia leading to complications such as pancreatitis and bone disease. Although hypocalcemia is usually noted in pancreatitis patients due to its link to morbidity, it is important to also be aware of hypercalcemia as it may be the cause of pancreatitis. The extent and longevity of the bone disease can lead to hungry bone syndrome causing severe hypocalcemia. Severe hypocalcemia can be life threatening, and patients need to be monitored very closely post operatively. With patients with severe bone disease from hyperparathyroidism, prevention should be the focus. Due to the acute presentation of our patients she could not be given calcitriol peri-operatively.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Berkoben M, Quarles D (2015) Hungry bone syndrome following parathyroidectomy.
- Khoo TK, Vege SS, Abu Lebdeh HS, Ryu E, Nadeem S et al. (2009) Acute Pancreatitis in Primary Hyperparathyroidism: A Population-Based Study. J Clin Endocrinol Metab 94(6): 2115-2118.
- Lenz JI, Jacobs JM, Op de Beeck B, Huyghe IA, Pelckmans PA et al. (2010) Acute necrotizing pancreatitis as first manifestation of primary hyperparathyroidism. World J Gastroentero 16(23): 2959-2962.
- Mayilvaganan S, Vijaya Sarathi HA, Shivaprasad C (2017) Preoperative zoledronic acid therapy prevent hungry bone syndrome in patients with primary hyperparathyroidism. Indian J Endocrinol Metab 21(1): 76-79
- Michels TC, Kelly KM (2013) Parathyroid Disorders. American Family Physician. Am Fam Physician 88(4): 249-257.
- Natalie E Cusano, Mishaela R Rubin, Donald J McMahon, Dinaz Irani, Laura Anderson (2014) PTH (1–84) Is Associated with Improved Quality of Life in Hypoparathyroidism Through 5 Years of Therapy. J Clin Endocrinol Metab 99(10): 3694–3699,
- Silverberg Shonni (2017) Primary Hyperparathyroidism: Clinical Manifestations.
- Shah M, Bancos I, Thompson GB, Richards ML, Kasperbauer JL et al. (2015) Teriparatide Therapy and Reduced Postoperative Hospitalization for Postsurgical Hypoparathyroidism. JAMA Otolaryngol Head Neck Sur 141(9):822–827.
- Witteveen JE, Thiel Svan, Romijn JA, Hamdy NA (2013) THERAPY OF ENDOCRINE DISEASE: Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol 168(3): R45-53.
-
F Sumrein and M Raghuwanshi. Necrotizing Pancreatitis, an unusual presentation of longstanding Primary Hyperparathyroidism. Arch Clin Case Stud. 1(3): 2019. ACCS.MS.ID.000512.
-
Primary hyperparathyroidism, Acute pancreatitis, Parathyroidectomy, Abdominal pain, Myalgia, Arthralgia, Epigastric tenderness.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






