 Case Report
Case Report
Allergic Reactions Associated with Ingestion of Protein Supplements
Andrew Rorie* and Jill A Poole
Department of Medicine/Division of Pulmonary, Critical Care, Sleep and Allergy, University of Nebraska Medical Center, Omaha, USA
Andrew Rorie, Department of Medicine/Division of Pulmonary, Critical Care, Sleep and Allergy, University of Nebraska Medical Center, Omaha, USA.
Received Date: September 22, 2020; Published Date:October 16, 2020
Introduction
IgE-mediated food allergy is a significant public health concern of which there is growing evidence the prevalence is increasing [1]. We present a case series of new-onset food allergy associated with ingestion of supplemental cow’s milk protein products.
Discussion
Patient #1 was 34-year-old male without history of food allergy. He drank an EAS whey protein shake and within 75 minutes he developed facial angioedema. The symptoms progressed to include generalized abdominal pain with cramps, explosive defecation, worsening periorbital and orolabial angioedema, chest tightness, shortness of breath, and pre-syncope. He was taken to the ER and received intramuscular epinephrine with immediate improvement in symptoms. After this reaction and prior to allergy consultation he tolerated traditional cow’s milk products (i.e. milk with cereal) on numerous occasions. He demonstrated sensitization to the EAS protein shake by skin prick testing (Figure 1A, Table 1).
Patient #2 was a 13-year-old male without history of food allergy. He drank a Vanilla Body Fortress whey protein shake and within 45 minutes he developed rhinorrhea, profuse sneezing, flushing with dermal pruritus, periorbital angioedema, diffuse urticaria and shortness of breath. The school nurse administered diphenhydramine with improvement in the symptoms. He subsequently tolerated cow’s milk on multiple occasions after this reaction occurred. He was skin tested to the Body Fortress protein shake which demonstrated sensitization (Figure 1B, Table 2).
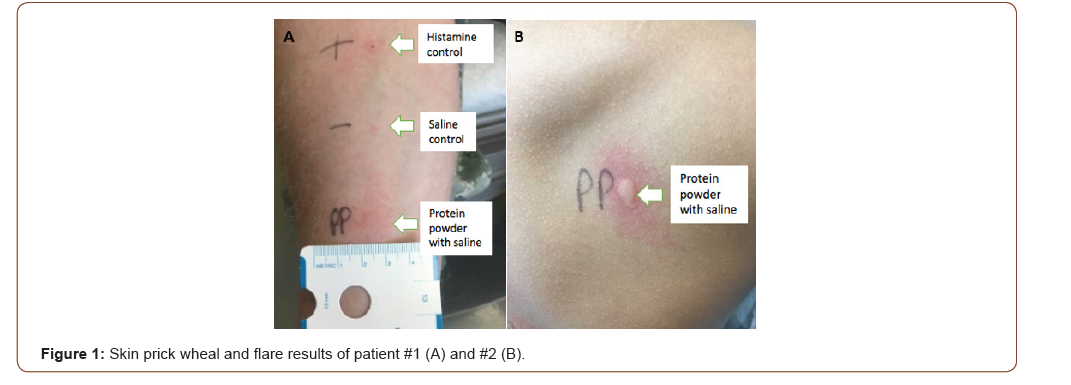
Table 1: Skin prick test and ImmunoCAP results of subjects with IgE-mediated allergy symptoms immediately after ingestion of whey protein products.
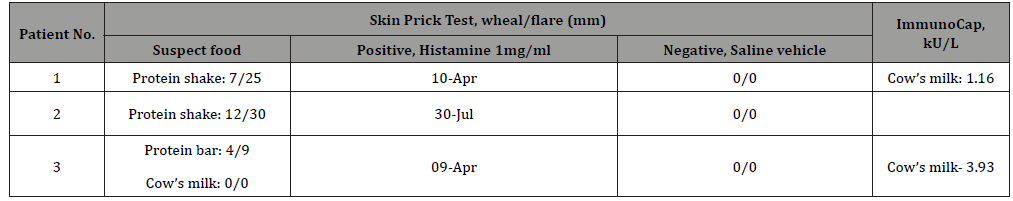
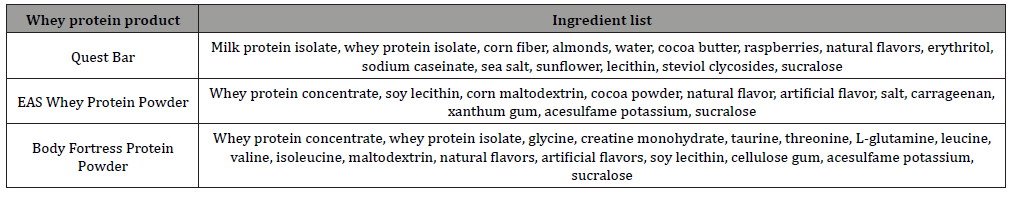
Table 2: Ingredient list of each whey protein product associated with allergic reaction.
Patient #3 was a 22-year-old female with a history of food allergy to chicken, egg and avocado. While eating a whey protein Quest Bar she immediately experienced the sensation of throat swelling and difficulty swallowing. She then became flushed with generalized dermal pruritus and lower lip numbness. She went to the ER and was treated with diphenhydramine and systemic corticosteroids with resolution of symptoms. She has strictly avoided cow’s milk products since this event. Skin test showed sensitization to the Quest Bar (Table 1). She has since ate and tolerated the other ingredients contained within the Quest Bar. She was also skin prick tested to almond which was negative.
To our knowledge this is the first case series of subjects experiencing immediate hypersensitivity reactions to supplemental protein products. There is a single report of a 24-year-old male developing cow’s milk allergy after frequent use of whey protein supplements. This case subject experienced typical IgE-mediated food allergy symptoms with both the whey protein supplement and traditional cow’s milk [2]. Two of our three subjects did not have any difficulty with traditional cow’s milk ingestion before or after the supplemental protein product reaction. One subject has completely avoided all cow’s milk products since the reaction. Although we did not challenge these patients to the specific product, the strong clinical history in conjunction with positive skin prick testing likely implicates these protein supplements. The testing was done by “prick-prick” method after the protein supplement was made into solution with saline. Each protein supplement was also skin prick tested in duplicate on control subjects. All control subject testing was negative.
The major cow’s milk allergens are casein and the whey proteins, lactalbumin and lactoglobulin. Whereas cow’s milk is a common food allergen in the pediatric population, it is considerably less common in adults [1]. None of the three subjects had a history of childhood cow’s milk allergy. In a review by Lieberman and colleagues, [3] which investigated causes of food allergy anaphylaxis in 133 predominately adult patients (mean age of 37 years), only one (0.75%) was confirmed cow’s milk allergy by oral graded challenge. The most common foods to cause anaphylaxis were shellfish (N=45, 33.8%) and peanuts (N=25, 18.7%) [3]. Although cow’s milk allergy is rare in adults, data suggest that allergic reactions to cow’s milk are typically quite severe. In a study by Lam and colleagues, [4] 20 of 30 subjects with cow’s milk allergy were classified as having severe reactions with 8 experiencing documented anaphylactic shock. By double-blind placebo-controlled food challenges, the dose of milk protein (0.3 to 300 mg) necessary to elicit subjective symptoms differed when compared to doses required to elicit objective evidence of reaction (300 to 9,000 mg or 10 to 300 mL of cow’s milk) [4]. In comparison, the concentration of whey protein in various protein supplements can be up to 30 to 60 grams as determined from information obtained from package product labeling. Thus, we suggest that it is possible that the high concentration of these proteins is likely responsible for eliciting new onset symptoms in previously, noncow’s milk allergic but likely sensitized individuals.
The immunologic mechanisms underlying these reactions remains unclear. It might be warranted to conduct a full composition analysis of these supplements as it is possible that they may be contaminated by another antigen other than cow’s milk protein. It is noted that many of these protein products also contain soy lecithin. Typically, soy lecithin does not contain sufficient soy residues to provoke a reaction, but it is not known whether these concentrated supplements are also high in soy residues. None of the three subjects had a prior history of soy allergy and all have regularly ingested soy since their respective reactions without any symptoms. The clinician should also be aware that protein supplements do not generally provide instructions for a recommended serving size, and therefore, the amount of protein powder consumed is at the discretion of the consumer. Lastly, during the production of these products there may also be chemical modifications, or protein aggregates created which could potentially change the immunogenicity of the proteins.
Allergic reactions to dietary protein supplementation products may be a new, developing cause of food allergy as demonstrated in this case series. Due to the widespread usage and growth of protein supplements, it is possible that this phenomenon could be under-recognized and/or under-reported. Further studies might be warranted. We suggest enhanced awareness about the use of protein supplements to guide care and testing when patients present with symptoms suggestive of an IgE mediated food allergy.
Acknowledgement
None.
Conflict of interest
Jill A Poole reports funding from the National Institute of Health (ES019325) and National Institute of Occupational and Safety Health (U54OH010162); all unrelated to the present topic. Andrew Rorie has no relevant disclosures.
References
- Boyce JA, Assaad A, Burks AW, Jones SM, Sampson HA, et al. (2010) Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel. J Allergy Clin Immunol 126(6 Suppl): S1-58.
- Sousa M, Reis Ferreira A, Moreira Da Silva J (2018) Bodybuilding protein supplements and cow’s milk allergy in adult. Eur Ann Allergy Clin Immunol 50(1): 42-44.
- Webb LM, Lieberman P (2006) Anaphylaxis: a review of 601 cases. Ann Allergy Asthma Immunol 97(1): 39-43.
- Lam HY, van Hoffen E, Michelsen A, Guikers K, CHW van der Tas, et al. (2008) Cow’s milk allergy in adults is rare but severe: both casein and whey proteins are involved. Clin Exp Allergy 38(6): 995-1002.
-
Andrew Rorie, Jill A Poole. Allergic Reactions Associated with Ingestion of Protein Supplements. 2(5): 2020. ACCS.MS.ID.000547.
-
Food allergy, Explosive defecation, Chest tightness, Shortness of breath, Throat swelling, Symptoms, Protein supplements.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






