 Review Article
Review Article
Post-Operative Atrial Fibrillation: Historical Aspects, Risk Factors and Complications Derived from its Origin
Jhon Alejandro Rico Gallego1*, Yeny Leandra Uribe Sánchez1, Iván Darío Morales-Tobar1 and Liseth Lorena Quintero Herrera2
1Emergency Department hospital San Vicente de Paúl - Santa Rosa de Cabal, Risaralda, Colombia
2Emergency Department Versailles, Colombia
Corresponding AuthorJhon Alejandro Rico Gallego, General physician, Emergency Department hospital San Vicente de Paúl - Santa Rosa de Cabal, Risaralda, Colombia.
Received Date: November 28, 2019; Published Date: December 10, 2019
Introduction
Cardiovascular Surgery is a speciality developed over the last six decades, undergoing profound changes in response to the needs of each historical stage. Its development occurred in close relationship with Thoracic Surgery for obvious anatomical reasons and both were born from general surgical activity, not specialized according to the concepts currently used [1]. Thoracic Surgery preceded Cardiovascular Surgery, which was defined as an independent entity as soon as the technological advances allowed physicians the entry into the cardiac cavities for the correction of congenital heart disease [1]. and thanks to these advances its surgical spectrum is much broader today.
The most important technological advance for the development of cardiovascular surgery was the Extracorporeal circulation (ECC), because thanks to the innovative technology applied in this procedure, physicians were allowed to perform successfully, interventions for correction of intra and extra cardiac defects unthinkable for the time due to the complexity and difficulty of access to the heart [2]. However, despite the success achieved with the ECC, this how all medical procedures are lack Total safety and since its development, surgical and post-operative complications have been reported, attributed to the effect generated by its use during surgical procedures. Within the spectrum of post-surgical complications, have been reported neurological, Respiratory, cardiovascular, endocrine, renal and haematic alterations [3].
Post-Operative Atrial Fibrillation (POAF)
Within the spectrum of cardiovascular complications caused by the use of cardiopulmonary bypass during the surgical act, there are cardiac arrhythmias, whose etiology is very varied and can occur in the context of a sympathetic discharge due to surgery, direct surgical aggression on the pathways of conduction, use of arrhythmogenic drugs (such as B agonists) and hydro electrolytic alterations[3]. Due to their high incidence, the impact on the hospitalization time of patients and the cost overruns caused to the health system due to the multiple complications derived from this pathology, atrial fibrillation (AF) is especially important.
AF is considered as that supraventricular arrhythmia characterized by disorganized atrial activation that leads to a deterioration of the mechanical function of the atrium. On the electrocardiogram, AF is manifested by the replacement of P waves with rapid oscillations or fibrillatory waves that vary in both shape and size and frequency, associated with an irregular ventricular response [4].
Atrial fibrillation is considered the most common arrhythmia after cardiac surgery and a higher incidence of this phenomenon has been reported between the second and third day of the postoperative period, however, it can happen at any time. Some studies show that postoperative AF (POAF) particularly in elderly patients with left ventricular dysfunction represents a risk factor for congestive heart failure, hemodynamic instability and ischemic stroke, which significantly increases the morbidity and mortality of these patients; In addition to prolonging their hospital stay [5].
Risk Factors for POAF
In general, POAF affects between 17% and 29% of patients undergoing coronary artery bypass surgery, 20% to 49% of patients undergoing valvular surgery and 31% to 60% of patients undergoing combined cardiac surgery [6], However, it has been shown that such arrhythmia is the result not only of the surgical act and the physiological changes induced by the ECC but also of the coalition and synergism of other clinical risk factors such as advanced age (over 65 years), sex male, history of AF, left ventricular dysfunction, chronic obstructive pulmonary disease (COPD), B-adrenergic blocker suspension, P wave duration greater than 116 ms, large left atrium, chronic renal failure, diabetes mellitus, among others such as heart disease rheumatic and ischemic [7,8].
Among the risk factors associated with the development of POAF it is the age the one that most affects, some studies report a frequency close to 1% in individuals under the age of 50 years and above 10% in those over 75 years [9] and taking into account the increasing proportion of the elderly population, an increase in this complication is estimated in the coming years, so in the US it is projected to increase from 5.2 million cases in 2010 to 12 , 1 million cases by 2030 [10].
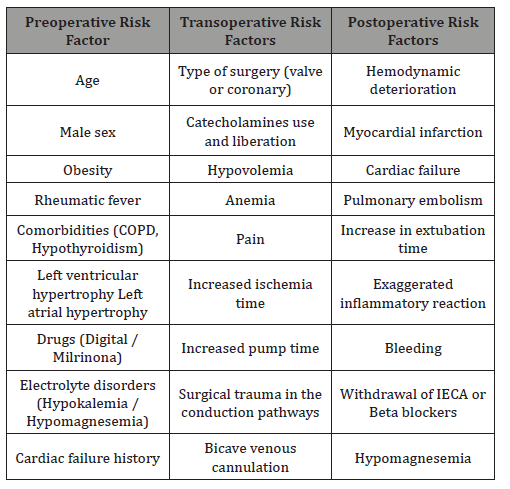
Some authors classify the risk factors for POAF as preoperative [11-13] (underlying atrial pathology), trans operative [14] (surgical trauma) and postoperative [15], the most important according to the literature are condensed in the following (Table 1).
Table 1: Risk factor for postoperative atrial fibrilation.
Classification of Atrial Fibrillation
The classification of atrial fibrillation is not easy, since the etiology, the atrial substrate of each patient, the basic pathology and the different treatments can vary very widely and none of the classifications can be perfect to guide the appropriate treatment in a determined patient [16], however there are worldwide accepted classifications, which allow a more approximate initial approach to the diagnostic and therapeutic process of AF.
• Recent diagnosis AF: Includes the FA detected for the first time, that of recent onset and of unknown onset.
• Paroxysmal AF: It lasts 7 days or less and remits without treatment (usually at 48 hours). Follow a recurring pattern with two or more episodes.
• Persistent AF: The episodes last longer than 7 days, a limit from which it has been observed that spontaneous remission is unlikely to occur.
• Permanent AF: Stable rhythm in AF, cardioversion is not effective, or if it is effective initially, recurrence at 24 hours. It is also known as chronic AF [17].
Because POAF is not included in these 4 forms of atrial fibrillation described above, the researchers Rodríguez Rosales et al, in their article Post-operative atrial fibrillation: Statement of a concept, published in 2014 by the medical journal of the Industrial University of Santander – Colombia decide to define it according to these 4 parameters:
1. POAF is that AF that occurs after an intrathoracic operation: if the patient underwent surgery that does not include opening of the thoracic cavity, it should not be included as postoperative atrial fibrillation. It can be classified as diagnosed AF for the first time, paroxysmal AF or the corresponding AF, but not post-operative. More than 95% of POAF is associated with cardiac surgery, leaving less than 5% for lung, esophagus, mediastinum, thymus surgeries, etc.
2. That it appears between the first and 21 days of the postoperative period: If it appears after 22 days it will not be considered post operative, since POAF has as triggers the mediators that are released as a result of the extracorporeal circulation, and the edema produced by the manipulation of the surgeon and the rupture and cannulation of atria. Those mediators begin to release during the surgical act, reach a peak at three days and are present in the body until 21 days.
3. But generally, it appears about 72 hours: because it is the time when mediators reach the highest values and begin the “plateau”.
4. That in its etiopathogenesis, the patient’s own elements, surgery and extracorporeal circulation are related: due to the differences that we point out in terms of epidemiology with respect to AF and the direct relationship it has with surgical time, the route of access, pump time, ECC time, etc., more than with sex, age, and other variables described for “conventional” AF [18].
POAF Triggers
Some authors have proposed that the reactive species derived from oxygen and oxidative stress that occur as a result of the inflammatory process after surgery are decisive in the process of atrial electrical remodeling, this, together with a genetic predisposition of the individual, are necessary factors for the development of AF [19]. In addition to oxidative stress, it has also been considered as a potential trigger of POAF the atrial distention caused by the mobilization of fluids from the interstitial and intracellular spaces, accumulated there during surgery, whether due to secondary edema the surgical activity as such or due to the overload of liquids commonly used in these procedures [20].
POAF Complications
Atrial fibrillation can be a “benign” arrhythmia in the general population, but when it occurs after cardiac surgery it is associated with various complications, some of which can seriously compromise life. Some authors have described an association between POAF and increased early and late mortality by up to 9.7% (ranging from 3 to 33.3%) after cardiac surgery [21,22]. Within the spectrum of complications derived from FAPO we have the neurological [23], cardiovascular [24,25], respiratory [26] and renal [27].
Neurological Alterations
POAF is an arrhythmia that represents an important economic burden for health systems [28], since it doubles mortality, triples hospital statistics and five times the risk of ischemic stroke. After cardiac surgery with ECC, an incidence of neuropsychological dysfunction has been detected in 14-48% of patients, registering serious neurological lesions with ischemic stroke in 2-5% of cases [29]. In addition, some studies have experienced that this risk is proportional to age, as it occurs in 1% of patients between 51 and 60 years but increases to 7% in those over 75 years [30].
It has been generally attributed that stroke and systemic arterial occlusion in patients with AF are secondary to thrombus embolism from the left atrium [31]. However, about 25% of stroke in patients with AF may be due to disease intrinsic of the cerebral vessels, and comorbidities of the patient because in some series it has been observed that half of the elderly patients who develop AF are basic hypertensive and approximately 12% of them have stenosis of the carotid artery. Cerebral infarction is usually evident as soon as the patient wakes up after surgery. Prolonged deterioration of the state of consciousness suggests the existence of multiple cerebral infarctions. Computed tomography (CT) of the brain shows small multiple infarcts, usually in the parietal and occipital regions or in the cerebellum, but also in the parasagittal regions of both cerebral hemispheres [32].
In the central part of a brain infarction the ischemia is deep and irreversible, constituting structural damage within a few minutes. On the other hand, in the periphery of the ischemia the structural integrity is preserved for a longer time, so the damage in this area is reversible; It is the so-called twilight zone, where according to the evolution time and the amount of cerebral parenchyma with irreversible structural lesion, the sequelae and the prognosis of the affected patient will be constituted [32].
Cardiovascular Alterations
At the Cardiovascular level, multiple post-surgical complications derived from ECC have been reported and whose incidence is directly influenced by the development or not of POAF, among them acute myocardial infarction (AMI), which occurred in 3.36% of the patients studied by Almassi GH, et al, who did not present POAF and in 7.41% of those who did; this same study showed an incidence of persistent congestive heart failure of 1.4% in those without postoperative arrhythmia and 4.57% in those who developed it [33]. One of the most feared cardiac complications described in the literature is hemodynamic instability given by marked systemic arterial hypotension that can lead to shock, cardiac arrest and death [25].
Respiratory Alterations
Respiratory failure after cardiac surgery is the result of many pre, intra and postoperative factors (including AF) that can directly or indirectly influence lung damage, 26 although only a small minority demonstrate an intermediate degree of lung deterioration. and an even smaller minority develops Acute Respiratory Distress Syndrome (ARDS) are complications that must always be taken into account because they lead to mortality rate between 36% and 60% [34] and significantly increase the length of hospital stay in the ICU (Intensive Care Unit), the need for invasive mechanical ventilation and the development of secondary infectious processes [35].
Renal Alterations
Postoperative renal failure (PRF) is a complication of high prevalence and importance in cardiac surgery. It is estimated that more than 30% of patients undergoing cardiac surgery develop clinically important PRF, requiring dialysis treatment in approximately 1 to 4% of cases [27,36]. ECC has been implicated for many years in the genesis of renal damage associated with cardiac surgery [37], however, it has also been shown that the development of POAF significantly increases its incidence [38]. This complication frequently occurs in the context of a multiple organ failure, which once established obscures the patient’s evolution, prolongs the hospital stay and is associated with a high mortality that can reach 80% [39,40].
Acknowledgement
None.
Conflicts of Interest
No conflicts of interest.
References
- Mestres C, Domenech A (2015) Cardiovascular Surgery, past, present and future, review article, Rev Fed Arg Cardiol 44 Special edition.
- Hessel EA (2014) A Brief History of Cardiopulmonary Bypass. Semin Cardiothorac Vasc Anesth. 18(2): 87-100.
- Rincon J, Novoa E, (2013) Management of postoperative complications of cardiac surgery in intensive care. journal of the Mexican Association of Critical Medicine and Intensive Care 27(3): 172-178.
- Craig T January, L Samuel Wann, Joseph S Alpert (2014) AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology 64(21): e1–e76.
- Luna P, Martinez M (2012) Atrial fibrillation after cardiac surgery, review article. Mexican Journal of Anesthesiology 35(1): 53-66.
- Jahangir K, Niina K, Eetu L (2016) Increasing Occurrence of Postoperative Atrial Fibrillation in Contemporary Cardiac Surgery. Journal of Cardiothoracic and Vascular Anesthesia 30(5):1302–1307.
- Hari B Keshava, Daniel J Boffa (2015) Cardiovascular Complications Following Thoracic Surgery. Thoracic Surgery Clinics 25(4): 371–392.
- Jesse M Raiten, Kamrouz Ghadimi, John GT, Augoustides, Ramakrishna H et al. (2015) Atrial Fibrillation after Cardiac Surgery: Clinical Update on Mechanisms and Prophylactic Strategies. Journal of Cardiothoracic and Vascular Anesthesia 29(3): 806–816.
- Wann LS, Curtis AB, January CT, et al, (2011) ACCF/AHA/HRS Focused Update on the Management of Patients with Atrial Fibrillation (Updating the 2006 Guideline). A Report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines 57: 223-242.
- Sheikh A, Patel NJ, Nalluri N, Agnihotri K, Spagnola J, et al. (2015) Trends in Hospitalization for Atrial Fibrillation: Epidemiology, Cost, and Implications for the Future. Progress in Cardiovascular Diseases 58(2): 105–111.
- Diem TT, Tran, Jeffery J Perry (2015) Predicting New-Onset Postoperative Atrial Fibrillation in Cardiac Surgery Patients. Journal of Cardiothoracic and Vascular Anesthesia 29(5): 1117–1126.
- Fleming GA, Marray KT, Yu C, Burbe JG, Petracek MR, et al. (2008) Milrinone use is associated with postoperative atrial fibrillation after cardiac surgery. Circulation 118(16): 1619-1625.
- Giovanni Peretto, Alessandro Durante, Limite LR, Cianflone D (2014) Postoperative Arrhythmias after Cardiac Surgery: Incidence, Risk Factors, and Therapeutic Management. Cardiol Res Pract 2014: 615-987.
- Hall RI, Smith MS, Rocker G (2007) The systemic inflammatory response to cardiopulmonary bypass: pathophysiological, therapeutic, and pharmacological considerations. Anest Analg 85(4): 766-782.
- Jesse Raiten, Prakash A Patel, Jacob Gutsche (2015) Management of Postoperative Atrial Fibrillation in Cardiac Surgery Patients. Seminars in Cardiothoracic and Vascular Anesthesia 19(2): 122–129.
- Gutierrez C, Blanchard DG (2011) Atrial fibrillation: diagnosis and treatment. Am Fam Physician 83(1): 61-68.
- Steven A Lubitz, Emelia J Benjamin, Ruskin JN, Fuster V, Ellinor PT (2010) Challenges in the classification of atrial fibrillation. Nature Reviews Cardiology 7(8): 451-460.
- Rodriguez E, Arazoza A, Vásquez F (2014) Postoperative Atrial Fibrillation: Statement of a concept, Rev of medical students of the Industrial University of Santande 27(2): 109-112.
- Maesen B, Nijs J, Maessen J, Allessie M, Schotten U (2012) Post-operative atrial fibrillation: a maze of mechanisms. Europace 14(2): 159-174.
- M Yadava, AB Hughey (2016) Postoperative Atrial Fibrillation: Incidence, Mechanisms, and Clinical Correlates. Heart Failure Clinics 12(2): 299-308.
- Alqahtani AAR (2010) Atrial Fibrillation Post Cardiac Surgery Trends Toward Management. The Official Journal of the Gulf Heart Association. 11(2): 57-63.
- Hashemzadeh K, Dehdilani M (2013) Postoperative Atrial Fibrillation following Open Cardiac Surgery: Predisposing Factors and Complications. Journal of Cardiovascular and Thoracic Research. 5(3): 101-107.
- Attaran S, Shaw M, Bond L, Pullan MD, Fabri BM et al. (2011) Atrial Fibrillation post cardiac surgery: a common but a morbid complication. Interact Cardiovasc Thorac Surg12(5): 772-777.
- Melduni RM, Suri RM, Seward JB, Bailey KR, Ammash NM, et al. (2011) Diastolic dysfunction in patients undergoing cardiac surgery:a pathophysiological mechanism underlying the initiation of new-onset post-operative atrial fibrillation. J Am Coll Cardiol 58(9): 953-961.
- Her AY, Kim JY, Kim YH, Choi EY, Min PK, et al. (2013) Left atrial strain assessed by speckle tracking imaging is related to new-onset atrial fibrillation after coronary artery bypass grafting. Can J Cardiol 29(3): 377-383.
- Ropolo Federico A, et al. (2016) Respiratory insufficiency in post-surgical cardiac surgery. Intramed journal 5(1): 27.
- Albert F Guerrero B, Jaime Camacho M, Nestor F Sandoval, Juan P, Umana M, et al. (2015) Factors associated with postoperative renal failure in myocardial revascularization surgery. Colombian Journal of Cardiology 23(3): 230-236.
- Boccuzzi SJ, Martin J, Stephenso J, Kreilick C, Fernandes J, et al. (2009) Retrospective study of total healthcare costs associated with chronic non valvular atrial fibrillation and the occurrence of a first transient ischemic attack, stroke or major bleed. Curr Med Res Opin 25(12): 2853-2864.
- Sun X, Lindsay J, Monsein LH, Hill PC, Corso PJ (2012) Silent Brain Injury after Cardiac Surgery: A Review: Cognitive Dysfunction and Magnetic Resonance Imaging Diffusion-Weighted Imaging Findings. J Am Coll Cardiol 60(9): 791-797.
- Salomon NW, Page US, Bigelow JC, Krause AH, Okies JE et al. (1991) Coronary artery bypass grafting in elderly patients: comparative results in a consecutive series of 469 patients older than 75 years. J Thorac Cardiovasc Surg 101(2): 209-218.
- Perez-Ortega I, Moniche-Alvarez F, Jimenez-Hernandez MD, Gonzalez Marcos JR (2012) Cardioembolic stroke from atrial fibrillation and new anticoagulation criteria: a therapeutic challenge. Rev Neurol 55(7): 74-80.
- Moré Duartea, Fuentes Herrera, Ceballos Álvarez, Cols (2015) Postoperative neurological complications in patients undergoing cardiac surgery with extracorporeal circulation. Cor Salud 7(1): 28-34.
- Almassi GH, Schowalter T, Nicolosi AC, Aggarwal A, Morizt TE, et al. (1997) Atrial fibrillation after cardiac surgery: A major morbid event? Ann Surg 226(4): 501-511.
- Stephens RS, Shah AS, Whitman GJ (2013) Lung injury and acute respiratory distress syndrome after cardiac surgery. Ann Thorac Surg 95(3): 1122-1129.
- Rodrigues CDA, Oliveira RARA, Soares SMTP, Figueiredo LC, Araújo S, et al. (2010) Lung injury and mechanical ventilation in cardiac surgery: a review. Rev Bras Ter Intensiva 22(4): 375- 383.
- Rincón Salas, Novoa Lago, Hortal Iglesias, Cols (2013) Management of postoperative complications of cardiac surgery in intensive care. Magazine Mexican Association of Critical Medicine and intensive therapy 28(3): 172-178.
- García Nidetz S, Perez Navarro A, Sossa Gil A (2009) Acute renal failure in the postoperative period of cardiovascular surgery. Review article. Electronic magazine of medical portals, intensive care and critical care.
- Lema G, Canessa R, Urzúa J, Jalil R (2008) Renal function in cardiac surgery with cardiopulmonary bypass: valvular and coronary patients. Rev Méd Chile 136: 459-466.
- Kim DH, Kim CA, Placide S, Lipsitz LA, Marcantonio ER (2016) Preoperative Frailty Assessment and Outcomes at 6 Months or Later in Older Adults Undergoing Cardiac Surgical Procedures: A Systematic Review. Ann Intern Med 165(9): 650-660.
- Lopez-Delgado JC, Esteve F, Javierre C, Ventura JL (2014) Severity of post-cardiac surgery acute kidney injury and long-term mortality: is chronic kidney disease the missing link? Crit Care 18(2): 424.
-
Jhon Alejandro Rico Gallego, Yeny Leandra Uribe Sánchez, Iván Darío Morales-Tobar, Liseth Lorena Quintero Herrera. Post-Operative Atrial Fibrillation: Historical Aspects, Risk Factors and Complications Derived from its Origin. Arch Biomed Eng & Biotechnol. 3(3): 2019. ABEB.MS.ID.000565.
-
Thoracic Surgery, Cardiovascular Surgery, Spectrum, Fibrillation, Morbidity, Mortality, Coalition Synergism, Trigger, Respiratory, Renal
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






