 Review Article
Review Article
Relationship between Pain Profiles and Comorbidity in Elderly Population
Rizaldy Taslim Pinzon, Vincent Ongko Wijaya* and Ranbebasa Bijak Buana
Department of Medicine, Duta Wacana Christian University, Indonesia
Vincent Ongko Wijaya, Faculty of Medicine Duta Wacana Christian University, Dr. Wahidin Sudirohusodo No.5-25, Yogyakarta, Indonesia.
Received Date: March 05, 2019; Published Date: March 26, 2019
Abstract
Introduction: Pain is an unpleasant sensory and emotional experience associated with actual and potential tissue damage. Elderly are more likely to have chronic disorders associated with pain, leading to disability and impaired quality of life.
Aim: The aim of this study was to explore the clinical profile of pain and its relationship with comorbidity in elderly population. Methods: This was an observational analytic study with cross sectional design. 111 geriatric patients with pain complaints were recruited from Neurology Department in Bethesda Hospital, Yogyakarta. Data obtained by interviewing patients that completed questionnaires to determine the pain profiles (intensity, type, properties, and location) and medical records for the comorbidity. Data were analyzed with univariate test and Chi-square test.
Result: There were 111 subjects consist of 40 (36%) males and 71 (64%) females. There were 79 patients with comorbidity (71.2%). The most common comorbidity in subjects was hypertension (63.3%), whereas the rarest was chronic kidney disease (2.5%). Mixed pain (85.6%) was the most common type of pain, multiple side pain (60.4%) was the most common location of pain, moderate pain (46.8%) was the most common pain intensity, and chronic pain (60.4%) was the most common properties of pain. Location of pain (p:0.642), type of pain (p:0.925), pain intensity (p:0.450), and pain duration (p:0.573) were not significant with patient comorbidity.
Conclusion: The comorbidity prevalence in elderly patients is 71.2%, there are no significant profile of pain that influence the comorbidity in geriatric patients.
Keywords: Pain; Comorbidity; Elderly population
Introduction
Pain is a common complaint that are often untreated or undertreated of the elderly. Therefore, undertreatment for pain can have an impairment on the health and quality of life of the elderly, resulting in depression, anxiety, social isolation, cognitive impairment, immobility, and sleep disturbances. Geriatric patients are more likely to have arthritis, bone and joint disorders, cancer and other chronic disorders associated with pain. As the number of elderlies continues to rise, frailty and chronic disease associated with pain are expected to increase [1]. The age limit for elderly in Indonesia is 60 years or more. In 2017, the elderly population in Indonesia reaches 23,66 million people or 9,03% from the country total population. The number of people worldwide 65 years and older was estimated at 506 million as of 2008 and by 2040 will increase to 1.3 billion. The morbidity of elderly population in Indonesia is 28,62% in 2015 and will increases every year. According to the International Association for the Study of Pain, as many as 48.5% of geriatric patients come to the hospital with pain complaints [2].
Persistent pain is highly prevalent and frequently causing disability in later life. It is most often attributable to musculoskeletal causes, usually involves multiple locations, and often occurs with other comorbidities. Most people with chronic disease usually have more than one health problem, which is referred to as multimorbidity. The term comorbidity is also used but this is now taken to mean that there is a defined index condition with other linked conditions, for example diabetes and cardiovascular disease.Early recognition of its impact can help improving outcomes for individuals affected [3,4]. In the past study, multimorbidity increases in the elderly where 30.4% of adults aged 45 to 64 years reported at least two chronic conditions, increasing to 64.9% of adults aged 65 to 84 years and more than 80% for those above 85 years old. Research about pain in multiple health condition in elderly is still very limited. Therefore, better understanding the relationship between the pattern of pain and comorbidities in geriatrics are expected to help physicians to choose appropriate treatment and improved patient clinical outcomes [5].
Aim
The aim of this study was to explore the clinical profile of pain and its relationship with comorbidity in elderly population.
Methods
Study design
This was an observational analytic study with cross sectional design in geriatric patients. All data were collected from 2017 to 2018 with interviews and medical records at the neurology department in Bethesda Hospital Yogyakarta. 111 subjects were recruited using consecutive sampling where sampling is based on all test subjects who met the inclusion and exclusion criteria in the study until a certain period of time. The inclusion criteria in this study were patients with age ≥ 60 years, who referred to a pain clinic due to complaint of neuromuscular pain and willing to be the subject research by signing informed consent and being willing to be interviewed.
Measurement
The instrument used in this study is a self-made pain essay sheet that corresponds to Pain Management Guideline for Bethesda Hospital Yogyakarta. Data retrieval conducted by interviewing patients enrolled in neurology department and from the patient’s medical record to ensure the patient’s answers. From the results of interviews and the patients medical records are used to see the relationship between variables.
Statistical Analysis
Data analysis will compare between the pain pattern (intensity, type, duartion, and location) and subjects comorbidity (hypertension, diabetes, etc) from the data acquired from the subjects. Descriptive statistics were used to describe subjects demographic, pain patterns and the comorbidities. The Chi-Square test was used to see relationships between the pattern of pain and comorbidity in this study. This study was approved by the Medical Research Ethics Committee and Health Faculty of Medicine Duta Wacana Christian University Yogyakarta and has received permission from Bethesda Hospital Yogyakarta.
Result
A total of 111 geriatric patients who met the inclusion criteria were participated in this study and included in the analyses. There were no missing data reported. This study aims to explore the clinical pattern of pain and its relationship with comorbidity in geriatric patients.
Subjects characteristics
Patients demographic is showed in Table 1. Female (61.6%) group has the largest percentage compared to male (38.4%) from the total subjects. The age characteristic was divided into 2 groups, which were 60-74 years and 75-90 years. Subjects with group age 60-74 years (81.1%) were more common than age 75-90 years (18.9%). Table 2 presented the clinical characteristics of the subjects, including the pain patterns and comorbidities. The pain profiles were divided into several criteria including pain intensity, type of pain, pain duration, and location of pain. Pain intensity was measured with visual analog score (VAS) and divided into 3 categories which are mild (VAS 1-3), moderate (4-6), and severe (VAS 8-10). Patients who complained moderate pain (46.8%) are more common than mild (35.1%) or severe pain (18.0%) intensity. Pain duration were categorized between acute (≤6 months) and chronic pain (≤6 months). Furthermore, 60.4% of patient reported a pain duration of more than 6 months and the remaining 39.6% of less than 6 months. The most common type of pain was mixed pain (85.6%) which is a combination of nociceptive and neuropathic pain, followed by inflammatory (10.8%) and neuropathic pain (3.6%).
Table 1: Demographic of Geriatric Patients.
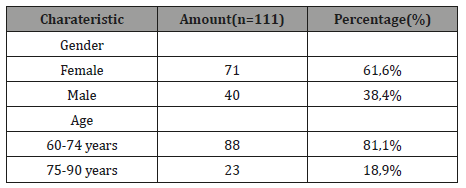
Table 2: Clinical Characteristics of Pain and Comorbidities in Geriatric Patients.
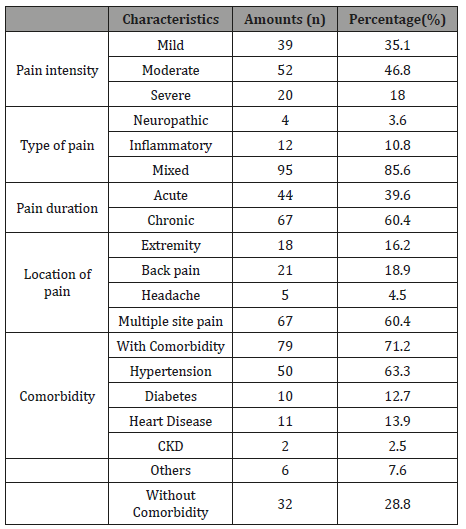
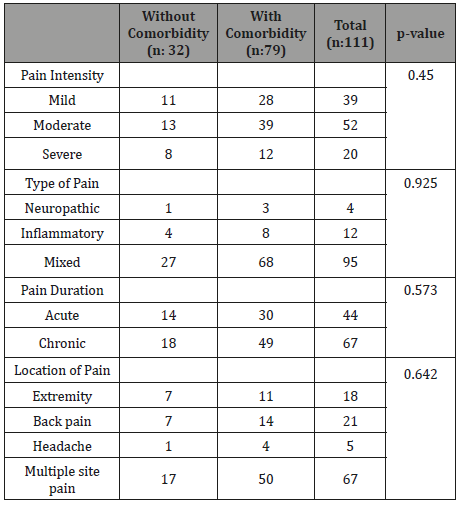
This study also assessed pain based on the location, 60.4% subjects complained multiple site pain, described as pain in two or more body sites with back pain being the most common type of pain (18.9%), followed by pain in extremity (16.2%), and headache (4.5%). Seventy-nine (71.2%) subjects presented with comorbidity, 50 (63.3%) had hypertension, 10 (12.7%) had diabetes, 11 (13.9%) had history of heart disease, 2 (2.5%%) had chronic kidney disease, and 6 (7.6%) had other diseases (osteoarthritis, stroke, etc.) Table 3. displays the relationship between various pain profiles and comorbidity in subjects. A total of 111 subjects were divided into two groups: 79 subjects with comorbidity and 32 subjects without comorbidity. In short, the analysis on pain profiles including pain intensity (p=0.45), type of pain(p=0.925), pain duration (p=0.573), and location of pain (p=0.642) revealed there were no statistically significant difference between any pain profiles and subjects with or without comorbidity (p>0.05).
Table 3: Comparison on pain profiles between patients with or without comorbidity.
Discussion
The study shows the pain profiles in geriatric patients and its relationship between patients with or without comorbidity. From the patients characteristics, female gender group were more common than male, and most patients were in age 60-74 years. Previous study demonstrated that women are more likely than men to experience a variety of pain especially recurrent pain and tend to have more severe levels of pain, more frequent pain and pain of longer duration than male [6-8].The different of pain perception between male and female may happen because the influence of sex hormones, testosterone in male have more anti-nociceptive effect compare to estradiol and progesterone in female [9]. The prevalence of pain in geriatric is increasing linear with age, it happened because the older patient has huge risk to injury and disease, thus increase the risk of pain, however the presence of dementia and communication difficulties can disturb the assessment result, causing the unreported pain experience. The finding was in line with past studies that found pain prevalence peak during late middle age (55-6) [10].
Past study showed severe pain as the most common pain intensity, this result is different with the finding of this study, it may happen because the difference in pain tolerance and perception of pain between each patient [11]. Previous studies found chronic pain as the most common duration of pain found in geriatric, the result is similar with this study that found chronic pain as the most common duration of pain in geriatric. The prevalence of chronic pain is increased with age; thus, the chronic pain is commonly found in geriatric patients [12]. Mixed type of pain was the most prevalence type of pain among geriatric patients in this study. Mixed pain is the result from the mix between neuropathy and nociceptive pain [13]. Previous studies result showed nociceptive pain followed by mixed type of pain as the most type of pain in geriatric patients [14]. According to pain location, previous studies found multiple site pain location as the most common pain location, this result consistent with the result of this study [7]. The Comorbidity pattern showed hypertension as the most comorbidity experience by patients in this study, this finding is in line with previous study that found hypertension followed by diabetes as the most commonly found comorbidity in geriatric patients [15]. The higher blood pressure level in patient with chronic pain have been associated with the increase or higher sensitivity to pain, this association is reversed in healthy person. The phenomenon may happen because substance that modulates both blood pressure and pain are same, thus chronic pain may exhaust the substance, and reduce the regulatory effect of the substance on blood pressure [16].
In our study, statistical analytic showed no difference in relation of pain pattern and comorbidity pattern between two group of subjects, it means the comorbidity does not affect or have a small impact to pattern of pain that experience by patients. Previous study investigate the chronic pain in temporomandibular pain disorder patients present the positive relation between pain duration and pain intensity with the present of comorbidity [17]. Other study also showed the increase of pain intensity associated with the greater level of comorbidity, this study also stated patients with four or more medical comorbidities exhibited higher pain intensity, whereas patient with zero to three medical comorbidities did not have significant different from each other, this statement could also explain the finding in our study [18].
Limitation in resource and time when this study conducted affecting the selection of study design. We suggest using cohort prospective design for better result in future research.
Conclusion
There are no significant different in pain profiles between patient with or without comorbidity. Our study showed that more than half geriatric with pain also have comorbidities, this study provides an overview about the condition that commonly found in geriatric with pain and consideration for management of pain in geriatric patient.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Cavalieri TA (2007) Managing Pain in Geriatric Patients. The Journal of the American Osteopathic Association 107(4): ES10-ES16.
- Indonesian Ministry of Health (2017) Elderly Analysis in Indonesia.
- Makris, UE Abrams, RC Gurland, B Reid MC (2014) Management of Persistent Pain in the Older Patient. JAMA 312(8): 825-836.
- Smith SM, Wallace E, O Dowd T, Fortin M (2016) Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 14: 3.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, et al. (2012) Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380(9836): 37-43.
- Unruh AM (1996) Gender variations in clinical pain experience. Pain 65(2-3): 123-167.
- Larsson C, Hansson EE, Sundquist K, Jakobsson U (2016) Chronic pain in older adults: prevalence, incidence, and risk factors. Scand J Rheumatol 46(4): 317-325.
- Patel KV, Guralnik JM, Dansie EJ, Turk DC (2013) Prevalence and Impact of Pain among Older Adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain 154(12): 2649-2657.
- Bartley EJ, Fillingim RB (2013) Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 111(1): 52-58.
- GibsonS J, Lussier D (2012) Prevalence and Relevance of Pain in Older Persons. Pain Medicine 13(2): 23-26.
- Pereira LS, Sherrington C, Ferreira ML, Tiedemann A, Ferreira PH, et al. (2014) Self-reported chronic pain is associated with physical performance in older people leaving aged care rehabilitation. Clinl Interv Aging 5(9): 259-65.
- Santos FC, de Moraes NS, Pastore A, Cendrologo MS (2015) Chronic pain in long-lived elderly: prevalence, characteristics, measurements and correlation with serum vitamin D level. Revista Dor 16(3).
- Cecil RL, Goldman L MD, Schafer AI (2016) Goldman’s Cecil medicine (25th ed.).
- Pylkko RS, Haanpaa M, Liira H (2016) Chronic pain among communitydwelling elderly: a population-based clinical study. Scand J prim Health care 34(2): 158-163.
- Al Modeer MA, Hassanien NS, Jabloun CM (2013) Profile of morbidity among elderly at home health care service in Southern Saudi Arabia. J Family Community Med 20: 53-57.
- Bruehl S, Chung OY, Jirjis JN, Biridepalli S (2005) Prevalence of clinical hypertension in Patients with Chronic Pain Compared to NonPain General Medical Patients. Clinical J Pain 21(2):147-153.
- Dahan H, Shir Y, Velly A, Allison P (2015) Specific and Number of Comorbidities are Associated with Increased Levels of Temporomandibular Pain Intensity and Duration. J Headache Pain 16: 528.
- Leong IY, Farrell MJ, Helme RD, Gibson SJ (2007) The Relationship Between Medical Comorbidity and Self-Rated Pain, Mood Disturbance, and Function in Older People With Chronic Pain. J Gerontol A Biol Med Sci 62(5): 550-555.
-
Rizaldy Taslim Pinzon, Vincent Ongko Wijaya, Ranbebasa Bijak Buana. Relationship between Pain Profiles and Comorbidity in Elderly Population. Annal Biostat & Biomed Appli. 1(5): 2019. ABBA.MS.ID.000525.
Pain, Comorbidity, Elderly Population, Emotional experience, Unpleasant sensory, hypertension, chronic kidney disease, Mixed pain, multiple side pain, moderate pain, Arthritis, Bone and Joint disorders, Cancer, Chronic disorders, Depression, Anxiety, Social isolation, Cognitive impairment, Immobility, Sleep disturbances.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






