 Research Article
Research Article
Effectiveness of Vibration on Myofascial
Trigger Points
Dawn T Gulick*, Sandra Campbell and Kerstin Palombaro
Institute for Physical Therapy Education, Widener University, USA
Dawn T Gulick*, Sandra Campbell and Kerstin Palombaro
Institute for Physical Therapy Education, Widener University, USA
Dawn T Gulick, Institute for Physical Therapy Education, Widener University, USA.
Received Date: September 27, 2023; Published Date:October 25, 2023
Abstract
Myofascial trigger points (MTrP) are a common source of musculoskeletal pain. The purpose of this manuscript is to compare the efficacy of vibration and manual compression (MC) on the pain pressure threshold (PPT) of MTrPs.
Methods: Thirty participants with two MTrP in the upper back (one on each side) were recruited. All MTrPs were tested with a dolorimeter for PPT pre- and post-treatments. On one MTrP, four vibration treatments were rendered via a VibraCool device at 200 Hz for 15-minutes per treatment over two weeks. On the other MTrP, the four sessions included three bouts of 90-seconds of MC at a seven on a visual analogue scale of 0-10 using an Index Knobber II.
Results: The mean pre-test PPT was 7.1 (1.6) pounds for the vibration side and 6.8 (1.7) pounds for the MC side. The mean post-test PPT was 8.5 (2.1) pounds for the vibration side and 8.5 (1.9) pounds for the MC side. The change scores found no significant differences (p = 0.186) between the treatments. Thus, vibration and MC were similar in the management of MTrP discomfort.
Conclusions: The current results are consistent with prior research. The mechanism for improvements in MTrPs treated with vibration has been theorized to be increased blood flow, normalizing the length of the sarcomeres, as well as activation of the Aβ fibers to abate pain via the gate control theory. The action of mechanotransduction, the conversion of a mechanical force to a molecular and cellular response to promote tissue repair and remodeling, has also been discussed. Furthermore, high-frequency vibration (200 to 400 Hz) has also been shown to activate the Pacinian corpuscles for pain management. Thus, vibration is a promising modality for the management of MTrP discomfort. Future studies should focus on the best combination of parameters, i.e. duration of treatment, rate of treatment application, and number of treatments.
Keywords: Vibration; Pain management; Myofascial Trigger Points
Introduction
Myofascial trigger points (MTrP) are a common source of musculoskeletal pain affecting a variety of ages and occupations. Travell and Simons defined a MTrP as “a hyperirritable spot in skeletal muscle associated with a hypersensitive palpable nodule in a taut band” [1, p5]. The etiology of MTrPs has been correlated with circumstances that include genetics, aging, performing a strenuous activity within a sedentary lifestyle, cumulative microtrauma, and abnormal posture [1,2].
The presence of a MTrP has been associated with muscle pain, weakness, and dysfunction [1,3-8]. Differences in histochemical characteristics, including acidity and pain catecholamines, have given rise to numerous hypotheses for the pathogenesis of MTrPs. One possibility is that the viscosity of hyaluronic acid is decreased in fascia, trapping pain afferents in a mesh. If so, therapies that manually or physiologically break up HA may allow for dispersal and reduction of afferent stimulation [9]. There are a variety of interventions purported to relieve or diminish the symptoms associated with MTrPs. These include injections/topical agents, taping, manual therapies, and modalities.
Studies using injections and topical agents have demonstrated mixed results. A study by Affaitati et al. [10] compared a lidocaine patch to placebo and bupivacaine hydrochloride (Marcaine) injection (N=60). Both the patch and the injection were successful at relieving pain. A study by Rauck, Busch, and Marriott [11] reported the effectiveness of heated lidocaine/tetracaine patches applied for 4-hours, twice daily for two weeks (N=17). There was a clinically significant reduction in pain for 40% of the participants and 25% had a substantial decrease. Over 75% were satisfied with the topical patch. Hsieh et al. [12] examined the efficacy of diclofenac patches on MTrPs on the upper trapezius muscle versus a placebo (N=153). The patches were applied for seven days. Visual analog scale (VAS) values, active cervical range of motion (ROM), and Neck Disability Index (NDI) scores all improved when reassessed on the fourth and eighth day. Cho et al. [13] studied capsaicin hydrogel patches on myofascial neck pain. They applied the patch 12-hours daily for four weeks. VAS, NDI, and Beck’s Depression Inventory Index all improved more than the control, but it was not statistically significant. Avrahami et al. [14] compared a single application of five topical (over-the-counter) products to control (N=120). Painpressure threshold (PPT) was the dependent variable. Bengay®, Muscle Care®, and Motion Medicine TM demonstrated statistically significant improvement in PPT; Biofreeze, Icy Hot®, and the placebo did not result in improvement.
There is an assortment of medical/athletic tapes available. One of these tapes used to treat MTrPs is Kinesio TexTM (KT) tape. The research results are variable. Bae [15] taped the sternocleidomastoid (SCM) muscle with latent trigger points three times per week for two weeks (N=42). The results were a reduction in SCM pain and VAS score with an increase in PPT and ROM. Gulick et al. [16] examined upper back MTrP PPT and compared KT taping to control (N=31). The KT taping technique used was the “star” inhibitory pattern. The tape was applied for three days and testing was performed prior to taping, immediately after taping, and four days after the tape was removed. Although the KT tape group improved, the difference from the control group was not statistically significant. Ozturk et al. [17] also used the inhibitory technique identified by KT tape (N=40). They taped for three days, took one day off, and then re-taped for three more days. Outcome measures were VAS, PPT, and manual muscle testing. All measures were better for the KT group but the authors were unable to articulate a mechanism for the improvement.
Manual compression (MC) has been studied by a large number of researchers using PPT as the outcome measure. Fryer and Hodgson [18] found 60-seconds of manual pressure at a level of 7/10 on the VAS resulted in significant improvement (N=37). Hanten et al. [19] compared 5-days of MC with twice daily stretching to a control (N=40). The participants were instructed to maintain the pressure until “release,” defined as a “letting go or melting” of the MTrP. The time for this to occur ranged from 60-90 seconds for each participant. The results were a significant difference in PPT and VAS between the two groups. Gulick, Palombaro, and Lattanzi [2] utilized a Backnobber II to apply MC to MTrPs of the upper back (N=28). A statistically significant increase in PPT tolerance with six repetitions of MC applied for 30-seconds for four days was found. Wilke, Vogt, and Banzer [20] used a foam roller to apply either static or dynamic compression to MTrPs (N=84). They defined static compression as 90-seconds at a 6-7/10 VAS score and dynamic compression as 90-seconds at five strokes/minute over the muscle at a 6-7/10 VAS score. They reported significant improvement in PPT in the static group over the dynamic and control groups. Manual techniques have also been employed using instruments. Gulick [4] utilized three techniques (1-minute sweeping, 1-minute swiveling, 2-minutes fanning, 1-minute sweeping) with stainless steel instruments. The swiveling technique has some similarities to MC. Treatment was rendered twice per week for three weeks and there was a significant improvement in PPT. A systemic review by Guzman-Pavon et al. [21] examined a variety of manual interventions across 15,158 studies and concluded manual therapy to be an effective therapeutic strategy.
Ultrasound (US) has also been studied using a variety of parameters (thermal and mechanical) to manage MTrP. Aguilera et al. [22] compared 2-minutes of 1-MHz pulsed ultrasound (1 W/cm2) to 90-seconds of MC. PPT improved in both groups. Thus, given the parameters used, the effectiveness of the US was most likely due to mechanical properties and/or the pressure of the transducer on the MTrP. Draper et al. [23] compared US to sham treatment (N=26). The US group was treated with a 3-MHz frequency at 1.4 W/cm2 for 5-minutes. These parameters could produce a vigorous thermal effect and is consistent with the authors’ rationale of reduced MTrP stiffness that reduced pain and improved PPT. Again, the slight improvement of the sham treatment may be due to the pressure on the transducer to maintain contact with the skin. This data is consistent with the results of Gulick et al. [24] where non-thermal US with Aquasonic gel (Parker Laboratories, Fairfield, NJ) compared to T-prep gel found slight improvements in PPT but they were not statistically significant (N=30). Likewise, thermal US with and without diclofenac resulted in a reduction in pain and an increase in PPT compared to sham (N=60). Ay et al. [25] reported the thermal effect may have increased blood flow, tissue metabolism, and tissue elasticity. The mechanical effects could have included degranulation of mast cells and increased acoustical streaming.
A variety of frequencies have been used with electrical stimulation (ES) to treat MTrPs. Takla and Rezk-Allah [26] compared US, US with diclofenac gel (phonophoresis), and ES (120-200 Hz) combined with phonophoresis (N=100). All three treatments demonstrated improvements in PPT and ROM. However, in another study, treatment at 10 Hz was shown to improve range of motion and VAS and a frequency of 60 Hz improved VAS and PPT [27]. Ebadi et al. [28] compared daily treatment for five days using acupuncture-like ES (5 Hz), conventional ES (120 Hz), and sham ES. VAS, DASH, and ROM all improved more for the 5 Hz and 120 Hz groups than the sham group. Long [29] has suggested low frequency stimulation increases blood perfusion, while success of higher frequencies may be related to the gate control theory.
Vibration has some similarities to that of ES in that vibration can be delivered at varying frequencies. The purpose of this study was to compare the efficacy of vibration at a frequency of 200 Hz delivered via the VibraCool® device to that of the known standard of care, manual compression, of the PPT of MTrPs.
Methodology
Instruments
A dolorimeter was used to measure pain-pressure threshold. This device has an ICC of 0.75 – 0.95 [30]. The VibraCool® device (PainCareLabs, Atlanta, GA) is a class 1, FDA-cleared, wearable device used to manage pain via a preset vibratory frequency of 200 Hz. The Index Knobber II (Pressure Positive, Gilbertsville, PA) was used to administer the manual compression treatments.
Procedures
A convenience sample was recruited from a variety of facilities. Each participant read and signed a consent form approved by the Institutional Review Board for the Protection of Subjects (#55-23). All participants were at least 18 years of age and presented with two myofascial trigger points in their upper back (one on each side). Participants could not have had any neck or shoulder surgery, no sensory deficits, and no broken skin in the upper back region. In the seated position, the researchers (experienced clinicians), palpated the upper back region for the presence of two MTrPs. The criteria used was that of Travelle and Simon [7]: the presence of a palpable band, presence of a hypersensitive tender spot in the taut band, and a palpable/visual local twitch response (snapping) with palpation. Once found, each was marked with a Sharpie® (Figure 1).

A dolorimeter was used to assess the PPT of each trigger point (Figure 2). Three measures were taken for each MTrP with 30 seconds between tests. The participant was instructed to indicate “when the pressure reached the level of discomfort of 7 on a 0 to 10 scale.” The measured values were not shared with the participants to avoid participant bias. For each participant, one MTrP was treated with vibration and one was treated with manual compression. Treatment sides were randomly assigned.

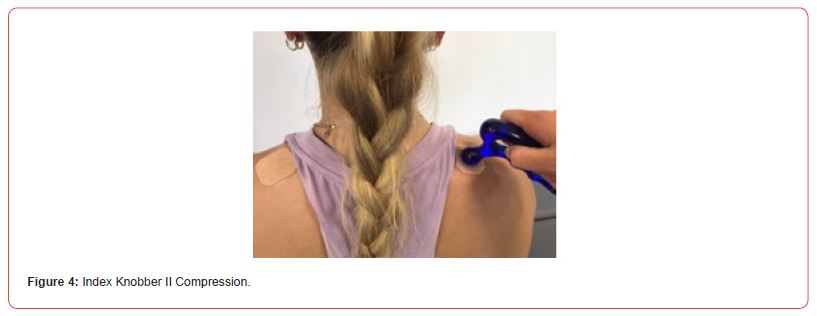
The VibraCool® device was secured on the MTrP with a shoulder strap to maintain constant pressure (Figure 3). Vibration treatment time was 15 minutes. The cold pack component of the VibraCool® device was not utilized in this study. Manual compression was administered to the other MTrP for 90-seconds, repeated three times with 30-seconds between applications. Manual compression was applied with an Index Knobber II (Figure 4) to a participantreported level 7 (0-10 scale). At the conclusion of the treatments, both trigger points were marked with a Sharpie®, sprayed with TUF-SKIN tape adherent (Cramer Products, Gardner, Kansas), and then covered with a 4 cm diameter piece of water-resistant therapy tape (Dynamic Tape, Bristol, United Kingdom) to be able to ensure the same site is treated/tested each time. Four treatments were rendered to each MTrP over a period of two weeks with at least two days but not more than four days between treatments. PPT was re-assessed on the fifth session (two to four days after the fourth treatment).

Data analysis
Statistics were run using SPSS version 27. Descriptive statistics were run on the highest PPT that the participants rated as a 7 on the numeric pain rating scale for the pretest and post-test vibration and manual compression conditions. Change scores were calculated between the pre-test and post-test highest PPT recorded value for both the vibration and manual compression conditions. A Wilcoxon signed ranks test was performed between the change scores. The non-parametric Wilcoxon signed ranks test was used because the sample was one of convenience and because participants served as their own controls. Post-hoc power analysis was run to determine the power of the present study as well as the sample size needed to detect a statistical difference.
Results
Thirty participants completed the study. The PPT results are displayed in Table 1. Wilcoxon signed ranks test on the change scores found no significant differences (p = 0.186) between the use of the vibration device and the standard of care for trigger point release. Post hoc power analysis revealed a low power of 0.271; to have sufficient power of 0.8, 124 participants would be needed to detect a statistically significant difference between the treatments.
Table 1:Pain Pressure Threshold Values for Pre-Test and Post-Test Between Treatments (measures are in pounds).

Discussion
The purpose of this study was to compare the outcome of vibration using the VibraCool® to the “known standard of care” treatment (manual compression) on MTrPs. The decision to compare these interventions with individuals serving as their own controls was a deliberate one. If vibration was compared to a control and found to be better, one would not know how vibration would fair to other previously studied interventions. So, the authors elected to compare vibration to manual compression since numerous studies have found compression at 90-seconds to a VAS of seven (0-10 scale) to be effective. When comparing the pre-tests and post-tests for the vibration treated MTrPs, there was a 19.7% improvement. Whereas, the pre-tests and post-test comparisons for manual compression treatment were 25%. These were determined to not be statistically different. Thus, the improvements with vibration were similar to that of manual compression.
The results of the current study are consistent with that of Duenas et al. [31]. When 28 patients treated their MTrPs in the upper trapezius and levator scapulae with vibration, improvements were reported in the Neck Disability Index and PPT compared to control. The authors theorized vibration may reduce MTrP pain by increasing blood flow [32] or normalizing the length of the sarcomeres [33]. In addition, vibration is also believed to activate the Aβ fibers to abate pain via the gate control theory [34]. Thompson et al. [35] has discussed the action of mechanotransduction which is the conversion of a mechanical force to a molecular and cellular response to promote tissue repair and remodeling.
Research by Cheathum et al. [30] explored the impact of a vibration roller, non-vibration roller, and a control on PPT and knee range of motion (N=45). The treatments were rendered to the quadriceps in prone for 2-minutes each. The vibration frequency of the roller was 33 Hz. The outcome was a statistically significant improvement in both measures with the vibration roller being superior. The mechanism for this effect was believed to be both mechanical and neurophysiological. The direct pressure of the roller is a mechanical effect that can impact the viscoelastic properties of the tissue, while the vibration may produce a neurophysiologic effect to result in pain reduction and tissue relaxation.
Research conducted by Hollins et al. [34] examined the impact of 12, 50, and 80 Hz vibration. They reported the high-amplitude of 80 Hz vibration resulted in the highest Pacinian activity. The greater the Pacinian activity the greater the pain reduction. Furthermore, Pacinian corpuscle’s sensitivity frequency has been reported to extend from 200 to 400 Hz. The vibration device used in the current study, the VibraCool®, functions at a frequency of 200 Hz. Thus, the mechanism of action for the reduction of pain measured by the increase in PPT could be the result of increased activity of the Pacinian corpuscles.
In the current study, four treatments were rendered with PPT assessments at the beginning and end of the treatments. However, Duenas et al. [31] studied the application of vibration over 10 sessions (daily x 15 minutes each) with assessments at sessions 0, 1, 5, and 10. They reported vibration and control groups as being similar at the start but demonstrating significant differences at sessions 1, 5, and 10 for the NDI and PPT. A graph of the outcome measures revealed a linear improvement in both measures over time. So, perhaps, the current study might have demonstrated greater improvements in the vibration group if the treatment had been delivered more often. In addition, it should be noted the VibraCool® is designed to be used with a mini-cold pack. In the interest of delineating results from vibration from that of cryotherapy, only vibration was used. Unlike the administration of manual compression which, depending on the location of the MTrP, may have to be administered by another person, the VibraCool® device can be secured in place with an elastic strap for the user to be mobile.
In summary, the first step in examining the efficacy is to determine positive outcomes. The current study did that with the comparison to manual compression. The next step is to determine the best combination of parameters, i.e. duration of treatment, rate of treatment application, and number of treatments. This is the challenge for ongoing studies on the use of vibration for pain management.
Limitations
The limitations of the current study should be revealed. There was one unexpected factor that may have influenced the data. On five participants, they exceeded the maximum reading of the dolorimeter. The device measured up to 11 pounds of force applied. Despite using the smallest diameter probe to intensify the force per unit area, maximums were surpassed on the post-test of five participants. These measures were all on the vibration-treated MTrPs with three of the same five being on the manual compression MTrP. For the purposes of data analysis, PPT values were recorded as 11.1 to indicate that their pressure threshold exceeded the measurement ceiling of the dolorimeter. For future studies, a dolorimeter with a greater range will be used.
Acknowledgements
The authors wish to acknowledge the in-kind contributions of VibraCool® devices and honorariums for the participants from Pain Care Labs. However, it should be noted Pain Care Labs had limited input into the methodology and no input into data collection, analysis, or construction of this manuscript. The authors would also like to thank Ms. Molly Lanza for her administrative assistance. Her attention to detail was appreciated.
Conflict of Interest
None.
References
- Simons DG & Dommerholt J (2005) Myofascial pain syndromes – Trigger Points. Journal of Musculoskeletal Pain 13(4): 73-81.
- Gulick DT, Palombaro K, Lattanzi JB (2011) Effect of ischemic pressure using a Backnobber II device on discomfort associated with myofascial trigger points. Journal of Body Work & Movement Therapies. 15(3): 319-325.
- Daniels JM, Ishmael T, Wesley RM (2003) Managing myofascial pain syndrome: sorting through the diagnosis and honing treatment. Physician and Sports medicine 31(10): 39-45.
- Gulick DT (2014) Influence of instrument-assisted soft tissue treatment techniques on myofascial trigger points. Journal of Body Work & Movement Therapies 4: 602-607.
- Desai MJ, Bean MC, Heckman TW, Jayaseelan D, Moats N, et al. (2013) Treatment of myofascial pain. Pain Management 3(1): 67-79.
- Diakow PRP (1992) Differentiation of active & latent trigger points by thermography. Journal of Manipulative Physiology & Therapy 15: 439-441.
- Travelle JG, Simon DG (1983) Myofascial pain & dysfunction: the trigger point manual. Baltimore (MD): Williams & Wilkins.
- Vazquez-Delgado E, Cascos-Romero J, Gay-Escoda C (2010) Myofascial pain associated to trigger points: a literature review. Part 2: differential diagnosis and treatment. Med Oral Patol Oral Cir Bucal 15(4): 639-643.
- Stecco A, Gesi M, Stecco C, Stern R (2013) Fascial Components of the Myofascial Pain Syndrome. Pain Headache Rep 17: 352-359.
- Affaitati G, Fabrizio A, Savini A, Lerza R, Tafuri E, et al. (2009) A randomized, controlled study comparing a lidocaine patch, a placebo patch, & anesthetic injection for treatment of TrP in patients with myofascial pain syndrome: evaluation of pain & somatic thresholds. Clinical Therapeutics 31(4): 705-720.
- Rauck R, Busch M, Marriott T (2013) Effectiveness of a heated Lidocaine/Tetracaine topical patch for pain associated with myofascial trigger points: Results of an open-label pilot study. Pain Practice 13(7): 533-538.
- Hsieh LF, Hong CZ, Chern SH, Chen CC (2010) Efficacy & side effects of diclofenac patch in treatment of patients with myofascial pain syndrome of the upper trapezius. Journal of Pain & Symptom Management 39(1): 116-125.
- Cho JH, Brodsky M, Kim EJ, Cho YJ, Kim KW, et al. (2012) Efficacy of a 0.1% capsaicin hydrogel patch for myofascial neck pain: a double-blinded randomized trial. Pain Medicine 13(7): 965-970.
- Avrahami D, Hammond A, Higgins C, Vernon H (2012) A randomized, placebo-controlled double-blinded comparative clinical study of 5 OTC topical analgesics for myofascial pain. Chiropractic & Manual Therapies 20: 7.
- Bae Y (2014) Change the myofascial pain and range of motion of the temporomandibular joint following kinesio taping of latent myofascial trigger points in the sternocleidomastoid muscle. Journal of Physical Therapy Science 26(9): 1321-1324.
- Gulick DT, Cain J, Cheney S, DeMarino D, Ettaro M, et al. (2015) Effects of Kinesio Tex taping on discomfort associated with myofascial trigger points. Orthopaedic Physical Therapy Practice 27(1): 32-36.
- Ozturk G, Kulcu DG, Mesci N, Silte AD, Aydog E (2016) Efficacy of kinesio tape application on pain and muscle strength in patients with myofascial pain syndrome: A placebo-controlled trial. Journal of Physical Therapy Science 28(4): 1074-1079.
- Fryer G, Hodgson L (2004) Effect of manual pressure release of myofascial trigger points in the upper trapezius muscle. Unpublished research from Victoria University, Melbourne Australia.
- Hanten WP, Olson SL, Butts NL, Nowicki AL (2000) Effectiveness of a home program of ischemic pressure followed by sustained stretch for treatment of myofascial trigger points. Physical Therapy 80(10): 997-1003.
- Wilke J, Vogt L, Banzer W (2018) Immediate effects of self-myofascial release on latent trigger point sensitivity. Biology of Sport 35(4): 349-354.
- Guzman-Pavon MJ, Cavero-Redondo I, Martinez-Vizcaino V, Torres-Costoso AI, Reina-Gutierrez S, et al. (2022) Effect of manual therapy interventions on range of motion among individuals with myofascial trigger points. Pain Medicine 23(1): 137-143.
- Aguilera FJ, Martin DP, Masanet RA, Botilla AC, Soler LB, et al. (2009) Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: a randomized controlled study. Journal of Manipulative and Physiological Therapeutics 32(7): 515-520.
- Draper DO, Mahaffey C, Kaiser D, Eggett D, Jarmin J (2010) Thermal ultrasound decreases tissue stiffness of trigger points in upper trapezius muscles. Physiother Theory Pract 26: 167-172.
- Gulick DT, Barsky J, Bersheim M, Katz K, Lescallette M (2001) Effect of ultrasound on pain associated with myofascial trigger points, Platform presentation APTA CSM, February.
- Ay S, Dogan SK, Evcik D, Baser OC (2011) Comparison of the efficacy of phonophoresis and ultrasound therapy in myofascial pain syndrome. Rheumatology International 31(9): 1203-1208.
- Takla MKN, Rezk-Allah SS (2018) Immediate effects of simultaneous application of transcutaneous electrical nerve stimulation & ultrasound phonophoresis on active myofascial trigger points. American Journal of Physical Medicine & Rehabilitation 97(5): 332-338.
- Hsueh T-C, Cheng P-T, Kuan T-S, Hong C-Z (1997) The immediate effective of electrical nerve stimulation and electrical muscle stimulation on myofascial trigger points. American Journal of Physical Medicine & Rehabilitation 76(6): 471-476.
- Ebadi S, Alishahi V, Ahadi T, Raissi GR, Khodabandeh M, et al. (2021) Acupuncture-like versus conventional transcutaneous electrical nerve stimulation in the management of active myofascial trigger points. Journal of Bodywork & Movement Therapies 28: 483-488.
- Long BC (2021) Repeated electrical point stimulation treatments for myofascial trigger points in the upper trapezius muscle. International Journal of Athletic Therapy & Training 26: 36-41.
- Cheathum SW, Stull KR, Kolber MJ (2019) Comparison of a vibration roller and a nonvibration roller intervention on knee range of motion and pressure pain threshold: A randomized controlled trial. Journal of Sport Rehabilitation 28: 39-45.
- Duenas L, Zamora T, Lluch E, Artacho-Ramirez MA, Mayoral O, et al. (2020) The effect of vibration therapy on neck myofascial trigger points: A randomized controlled pilot study. Clinical Biomechanics 78: 105071.
- Armstrong WJ, Grinnell DC, Warren GS (2010) The acute effect of whole-body vibration on the vertical jump height. J Strength Cond Res 24 (10): 2835-2839.
- Barbara Cagnie, Vincent Dewitte, Tom Barbe, Frank Timmermans, Nicolas Delrue, et al. (2013) Physiologic effects of dry needling. Current Pain Headache Rep 17 (8): 348.
- Hollins M, Corsi C, Sloan P (2017) Pacinian signals determine the direction and magnitude of the effect of vibration on pain. Perception 46(8): 987-999.
- Thompson WR, Scott A, Loghmani MT, Ward SR, Warden SJ (2016) Understanding mechanobiology: physical therapists as a force in mechanotherapy and musculoskeletal regenerative rehabilitation. Phys Ther 96 (4): 560-569.
-
Dawn T Gulick*, Sandra Campbell and Kerstin Palombaro. Effectiveness of Vibration on Myofascial Trigger Points. W J Yoga Phys Ther & Rehabil 4(2): 2023. WJYPR.MS.ID.000583.
-
Myofascial trigger points (MTrP), Pain-pressure threshold (PPT), shoulder surgery, Neck Disability, Aβ fibers, VibraCool®
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






