 Review Article
Review Article
New Options for Non-Penetrating Glaucoma Surgery
Nuha Alfayumi, Department of Ophthalmology, Damascus, Syria.
Received Date: November 22, 2021; Published Date: December 07, 2021
Deep Sclerectomy
First choice and as initial procedure for primary congenital glaucoma.
• Glaucoma is a complex eye disease which is the second cause of blindness in the world. It consists of the progressive deterioration of the layer of retinal nerve fibers and of the optic nerve, which lead to the appearance of defects in the visual field and of atrophy of the optic nerve. In the majority of cases, this pathology is associated with increased intraocular pressure (IOP) due to the inhibition of correct drainage of the aqueous humor of the eye. The management of glaucoma requires chronic treatment with a spectrum of therapeutic options including drugs, laser treatment, incisional filtration surgery, drainage devices, and surgical implants. Deep sclerectomy (DS) is a nonpenetrating procedure for the treatment of openangle glaucoma (OAG).
• Glaucoma Surgery is rarely restorative or Curative. It Usually Substitutes One Problem for another.
The goal of Glaucoma Surgery is too Lower intra ocular pressure. Unfortunately, many surgeons who have operated on glaucoma have been sadly surprised on the day after performing the surgery at most of the time, like soft, painful eyeball, with collapsed anterior chamber, sometime choroidal detachment and tendency to develop cataract.
Deep Sclerectomy has gained importance in glaucoma surgical treatment in contrast to trabeculectomy, it enhances aqueous humor outflow acting on the major resistance site without entering the anterior chamber, thus reducing the incidence of the intra and the postoperative, over filtration, hypotony, and its potential sequelae. Moreover, the cataract hyphemia, endothelial damage and macular edema is lower with DS.
May be difficult to do it and more demanding, need more practice and true knowledge to anatomical features, but it is excellent option if gained skill to do this procedure.
Deep Sclerectomy is a bad name for a good surgery, Because Peeling off the external trabecular or the inner wall of Schlemm’s canal to obtain a good filtration is essential phase. Thus, the technique is more appropriately described as a:
Nonpenetrating external trabeculectomy
And not deep sclerectomy.
• Inclusion criteria: Primary or secondary open angle glaucoma no longer controlled by medical treatment. In my experience First choice and as initial procedure for primary congenital glaucoma.
Deep Sclerectomy in Congenital Glaucoma
Purpose: Retrospective statistic study, to evaluate the results of deep sclerectomy as a first-choice treatment in congenital glaucoma.
Participants: fifty-seven patients, ninety eyes have undergone deep sclerectomy.
Intervention: for all cases, surgery was done with mitomycin \c\ for three minutes that was put between the conjunctiva and the sclera before the flap incision.
Main outcomes measures: surgical success was defined as a complete success if the intraocular pressure (IOP) was 20mmHg or less without any anti glaucoma medication or the need for reoperation. Qualified success was if I.O.P. is 20 mmhg. Or less either after second surgery or a use of antiglaucoma medications after first surgery. Patients requiring additional surgery with IOP more than 20mmHg in spite of antiglaucoma medication use. Failed treatment was when IOP not controlled after first, second surgery with or without antiglaucoma medication.
Results: seventy-five patients, ninety eyes were operated. patient’s age between 3days and 12years, follow up examination one day, one week, one month and every six months till four years after surgery. Complete success rate were82,3% main IOP decreased from 33,7mmHg to 12,8mmHg. Qualified success rates were 15,5% and failed rates were 3,4%.
Conclusion: High success rates obtained in congenital glaucoma patient treated by deep sclerectomy as a first-choice treatment. Randomized controlled clinical trial in comparison with the other treatments need to be done in goal to have a real evaluation of clinical results of this new surgery in congenital glaucoma patients. Non-perforating trabecular surgery is increasingly becoming the standard surgical treatment for open-angle glaucoma. Just as effective as trabeculectomy with a lower complication rate and greatly improved patient comfort. Congenital glaucoma surgeries, including goniotomy, and trabeculectomy, have been the methods of choice of surgical therapy for congenital glaucoma for decades .Encouraged by relatively good success rates and safety profile of deep sclerectomy ,multiple reports are available on the use of this non-penetrating technique in congenital glaucoma cases. Nonpenetrating procedures may offer another approach to tackle the digenetic outflow system. They may be technically more demanding, especially in stretched globes, but are probably safer than trabeculectomy, if performed properly.
Patients and Methods
It is a retrospective statistic study for a supposed new method of treatment of an old disease as congenital glaucoma. Patients seen, diagnosed, and treated in the national eye center: IBN AL nafes’ hospital in Damascus.
All families of the patients were informed about the nature of the pathology and the treatment. Deep sclerectomy was done in all cases. Fornix based conjunctival flap was used . 4,5- 4,5mm wick-cell sponge soaked in a 0,5mg/ml solution of mitomycin-c was applied for 3 minutes, and the area was irrigated thoroughly with BSS.
Mitomycin’s was used in all patients. A one third thickness 4.5mm rectangular scleral flap carrying on 2mm through clear cornea was fashioned. Second triangular deep scleral flap was fashioned in the periciliary level that was identified by the dark color of the underlying choroids. Identification of the scleral spur by the pearly and shiny appearance of scleral fibres which became concentric to the limbus. To avoid the direct, enter in the anterior chamber we change the blade direction during completion of deep scleral flap dissection, discovering of trabecula-Descemet-membrane, resection of deep scleral flap with the internal wall of scheme’s canal and juxtacanalicular trabecular meshwork. Superficial scleral flap was sutured with 10-0 nylon sutures followed by heal on GV injection under the flap .Conjunctival incision was closed with 8-0 vicarly mattress sutures. The postoperative regimen included topical ofloxacin 0,03% for one week and prednisolone acetate 1% for 4 weeks. Preoperative data obtained for each patient included age, combined syndrome or any previous ocular surgery or antiglaucoma medication used, IOP, visual acuity if possible. Intraoperative data included type of surgery, type of antimetabolite used and complications. Postoperative data collected 1 day,1 week, 1 month,3 months, 6 months, and every 6months, till 4.5years for the first case. Postoperative data included IOP, VA, if possible, corneal appearance and shape, possible complications. Two levels of surgical success. The primary outcome measure was defined: 1) Complete success defined as IOP of 20mmhg or less without antiglaucoma medications. 2) Qualified success, defined as having an antiglaucoma medication or second antiglaucoma surgery. 3)Patient considered to have failed treatment when IOP still more than 20mmgh even if the patient had had more than one antiglaucoma surgery (deep sclerectomy or trabeculectomy) with addition of antiglaucoma medication. Hypotony was defined as an IOP less than 6mmgh.Results
Of the total of 90eyes of 57 patients enrolled in the study, 74 eyes or 82,3% had complete success ,14 eyes or 15,5% had qualified success, and 2cases or 2,2%were considered as failure! (Table 1,2).
Table 1: Illustrates the Tension Results and Percentage of Success.
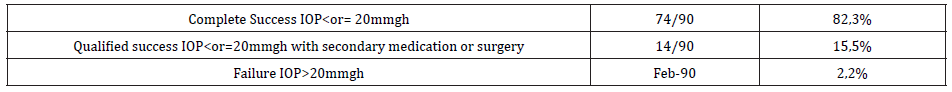
Table 2: Illustrates Considered Qualified Success Cases.
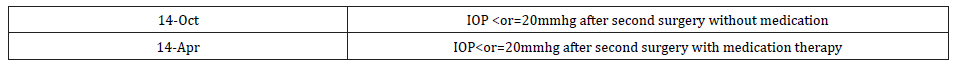
10 cases have received second surgery, trabeculectomy was done for 6 cases and second deep sclerectomy was done for4 cases with normal tensional result that IOP was < or=20mmgh without an additional medical therapy. Still 4cases of this qualified success that the IOP was < or=20mmgh after second trabeculectomy but with antiglaucoma medication therapy. 2 failed cases, treated later, one has had Ahmad’s valve surgery, second case has had photocyclodestruction.
Discussion
Congenital glaucoma is one of the most fearful blinding diseases in infancy. At the time, the ethology, physiopathology and treatment of this disease still have an obscure moment in our knowledge. Deep sclerectomy was an interesting idea for the treatment of this disease. Therefore, new anatomic theories suggest that Barkan’s membrane does not exist no more, and the rise of IOP in this eye is related to different anatomic malformation either for the anterior segment or for the anterior chamber angle. The very low rate of complication even in intraoperative or post operative times, (we did not see any choroidal detachment even the IOP. is less than 6mmhg in the first four weeks after surgery as a good sign for good clinical result) the well tolerated surgery for this particular patient and the high percentage of normalization of intraocular pressure were an advantages element when considering deep sclerectomy as a first-choice treatment in congenital glaucoma.
This study has a good sample size for this special medical problem as congenital glaucoma. A randomized clinical trial study with the other methods of treatment might be necessary to do if we want to optimize our clinical results.
Conclusion
In conclusion, deep sclerectomy can offer a good possibility of treatment for congenital glaucoma patients, and an easy follow and non-perforated eye. The important thing is more effective for the visual rehabilitation of these patients. You know adequate intra ocular pressure control is only half the job, the other major task is visual rehabilitation and the prevention of amblyopia. many ophthalmologists avoid pediatric glaucoma because it clearly takes a lot of time and difficult, but to me with this Technique, it’s always worth the effort. It may not affect a huge number of patients, but it will make a huge difference in whether this child goes on to be an adult who can see and function in society. More information still important to have about the ethology and physiopathology of the disease in goal to get better clinical results and quality of life for this patient Appendix.
Acknowledgement
None.
Conflict of Interest
None.
References
- Denis D, Pommier S, Coste R, Fogliarini C, Benso C, et al. (2008) Deep sclerectomy in congenital glaucoma: results of a study lasting more than 3 years. J Fr Ophthalmol 31(2): 173-179.
- Feusier M, Roy S, Mermoud A (2009) Deep sclerectomy combined with trabeculectomy in pediatric glaucoma. Ophthalmology 116(1): 30-38.
- Koukkoulli A, Musa F, Anand N (2015) Long-term outcomes of needle revision of failing deep sclerectomy blebs. Graefe's Archive for Clinical and Experimental Ophthalmology 253(1): 99-106.
- Anderson DR (1981) The development of the trabecular meshwork and its abnormality in primary infantile glaucoma. Trans Am Ophthalmol Soc 79: 458-485.
- Al-Obeidan SA, Osman Eel-D, Dewedar AS, Kestelyn P, Mousa A (2012) Efficacy and safety of deep sclerectomy in childhood glaucoma in Saudi Arabia. Acta Ophthalmol 92(1): 65-70.
- Qiao CY, Wang LH, Tang X, Wang T, Yang DY, et al. (2009) Epidemiology of hospitalized pediatric glaucoma patients in Beijing Tongren Hospital. Chin Med J 122(10): 1162-1166.
- Taylor RH, Ainsworth JR, Evans AR, Levin AV (1999) The epidemiology of pediatric glaucoma: the Toronto experience. J AAPOS 3(5): 308-315.
- Genĉík A (1989) Epidemiology and genetics of primary congenital glaucoma in Slovakia: description of a form of primary congenital glaucoma in gypsies with autosomal-recessive inheritance and complete penetrance. Dev Ophthalmol 16: 76-115.
- Kipp MA (2003) Childhood glaucoma. Pediatr Clin North Am 50(1): 89-104.
- Gould DB, John SW (2002) Anterior segment dysgenesis and the developmental glaucomas are complex traits. Hum Mol Genet 11(10): 1185-1193.
- Ramtohul P, Chardavoine M, Beylerian M, Aziz A, Matonti F, et al. (2018) Decompression retinopathy following nonpenetrating deep sclerectomy for primary congenital glaucoma. BMC Ophthalmol 18(1): 240.
- Chen TC, Chen PP, Francis BA, Junk AK, Smith SD (2014) Pediatric glaucoma surgery: a report by the American Academy Of Ophthalmology. Ophthalmology 121(11): 2107-2115.
- Bayoumi NH (2012) Deep sclerectomy in pediatric glaucoma filtering surgery. Eye 26(12): 1548.
- Dubey S, Agrawal A, Chauhan L, Mukherjee S, Douglas G (2015) Combined trabeculotomy-trabeculectomy with antimetabolite and releasable suture: outcome with primary congenital glaucoma in a north Indian population. Nepal J Ophthalmol 7(1): 16-25.
- Chang TC, Cavuoto KM (2013) Surgical management in primary congenital glaucoma: four debates. J Ophthalmol 2013: 612708.
- Tawara A, Inomata H (1981) Developmental immaturity of the trabecular meshwork in congenital glaucoma. Am J Ophthalmol 92(4): 508-525.
- Sampaolesi R, Caruso R (1982) Ocular Echometry in the Diagnosis of Congenital Glaucoma. Arch Ophthalmol 100(4): 574-577.
- Walton DS Congenital glaucoma. In: Traboulsi EI [ed.], Genetic Diseases of the Eye. New York, NY: Oxford University Press 1998: 177-182.
-
Nuha Alfayumi. New Options for Non-Penetrating Glaucoma Surgery. W J Opthalmol & Vision Res. 3(5): 2021. WJOVR.MS.ID.000575. DOI: 10.33552/WJOVR.2021.03.000575
-
Deep Sclerectomy, Randomized Controlled Clinical, Trabecular Surgery, Open-Angle Glaucoma, Congenital Glaucoma Surgeries, Including Goniotomy, Trabeculectomy, Trabecula-Descemet-Membrane
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






