 Mini Review
Mini Review
Management of Intraocular Foreign Bodies of Posterior Segment
Hsouna Zgolli1, Khalifa Alsawidi2*, Sonya Mabrouk1, Gareeb Bagdadi2, Chiraz Abdelhedi1, Imen Zghal1 and Leila Nacef1
1Assistant Professor, Department A, Institute Hedi Raies of Ophthalmology, Tunis, Tunisia
2Assistant Professor, Tripoli Eye Hospital, Tripoli, Libya
Khalifa Alsawidi, Assistant Professor, Tripoli Eye Hospital, Tripoli, Libya
Received Date: March 26, 2022; Published Date: April 20, 2022
Abstract
Purpose: to study the epidemiological and clinical characteristics of penetrating wounds with intraocular foreign bodies (IOFB) and to discuss
different timing and surgical techniques related to the extraction of the foreign body.
Methods: We collected information from the files of 60 patients hospitalized for penetrating wound with metallic IOFB over a period of 10 years
from 2010 to 2020. All patients underwent vitrectomy and extraction of the IOFB immediately after the first consultation.
Results: The age ranged from 3 to 90 years with a predominance of males. The circumstances were dominated by work accidents (58.33%).
The IOFB was metallic in 75%. The size of the IOFB varied from 1 to 30 mm with a median of 5.39 mm. The preoperative visual acuity varied between
8/10 and light perception. The postoperative visual acuity depended of the primary visual acuity and the evolution.
Conclusion: At the end of this study, our results testify to the severity and seriousness of these ocular injuries and show that prevention remains
a fundamental element in the management of penetrating wounds with IOFB, not only in the workplace but also in the home.
Keywords: Intraocular; Foreign body; Management
Introduction
Ocular trauma with open globe injury is a severe cause of visual impairment and monocular loss of vision that can lead to substantial visual morbidity, blindness, and lifelong sequelae in young working people, especially males [1,2]. The incidence of intraocular foreign body (IOFB), in this kind of trauma is between 14 to 35% [1,3]. Intraocular foreign bodies may be removed with an intraocular magnet or forceps through either a sclerotomy or corneal incision. It depends on their location, their size, their magnetic properties but also on the status of the lens [1]. Various surgical techniques for removing IOFBs have been described. However, Pars plana vitrectomy (PPV) is the first surgical technique, recommended to remove a posterior foreign body [4,5]. Recent advances in vitreoretinal surgery, has suggested to improve the outcomes of PPV in the management of posterior segment IOFBs. The aim of our work was to study the epidemiological and clinical characteristics of penetrating wounds with intraocular foreign bodies and to discuss different timing and surgical techniques related to the extraction of IOFB.
Methods
A retrospective, descriptive analytic study was enrolled. We collected information from the files of 60 patients hospitalized for penetrating wound with IOFB over a period of 10 years from 2010 to 2020. The files was selected according to the definition established by the Birmingham Eye Trauma Terminology classification. Patients with penetrating wounds without IOFBs, with perforating wounds, with extraocular orbital foreign bodies, with non-extracted IOFBs and patients with anterior ocular pathology responsible for a known decrease in visual acuity were excluded from the study. All patients underwent a complete general ophthalmologic examination prior to the surgical procedure. Preoperative visual acuity, site of entry of foreign body, capsular and zonular integrity was assessed. Ultrasound B-Scan and/or Orbital CT scan were performed in all patients to locate and evaluate the IOFB (Figure 1). Postoperatively all patients received topical antibiotics and steroid for four weeks. In each case recording of best corrected visual acuity (BCVA), intraocular pressure measurement, slit lamp biomicroscopy and indirect ophthalmoscopy was done postoperatively. Written informed consent for participation was obtained from all patients and the study is adherent with the Declaration of Helsinki.
Surgical Technique
The surgery was performed under local general anesthesia for most of patients. The corneal wound was sutured previously. We performed, firstly, a phacoemulsification of an eventual traumatic cataract and a foldable hydrophobic acrylic intraocular lens was implanted into the capsular bag. Three 23-gauge sclerotomies were created for the infusion line, endo illumination and vitreous cutter. We started performing a complete central and peripheral vitrectomy. A complete 360° indentation was done to remove the whole vitreous debris. The metallic foreign body was identified. We released the foreign body from vitreous proliferations. A 20-gauge sclerotomy was made in the temporal superior quadrant on 3,5mm to the limb. A 20-gauge foreign body forceps was carefully introduced on the ocular cavity and the foreign body was gently extracted through the pars plana sclerotomy (Figure 2). We finished the surgery by verifying the absence of a tear or any peripheral retinal break (video supplemental material).
Results
Table 1: Circumstances of the Accident.
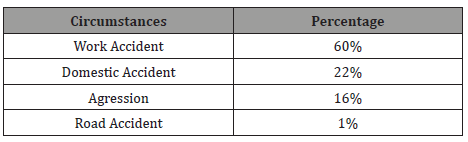
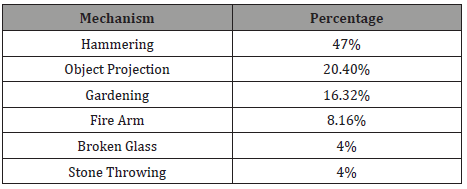
The age of our patients ranged from 3 to 90 years with an average of 32.7 years with a predominance of males, the sex ratio was 9 (54 men/6 women). The circumstances of the accident were dominated by work accidents (58.33% of cases) (Table 1). Hammering was the main cause of these injuries (23 patients (47%)). No patient reported the use of eye protection at the time of the traumatic accident. In our study, only one case of road traffic accident was noted (Table 2). The IOFB was metallic in 75%, organic in 16.66% and mineral in 6.66% of cases. The size of the IOFBs varied from 1 to 30 mm with a median of 5.39 mm. Anatomical success was achieved in 52 patients, 6 months after surgery with reattached retina and preserved eyeball. 2 patients developed endophthalmitis and the evolution was towards the phthisis of the eyeball. 6 patients were re operated for post-traumatic retinal detachment with good evolution. Functionally, the preoperative visual acuity was between 8/10 and well directed light perception. The postoperative visual acuity was fully dependent on the preoperative visual acuity as well as the evolution. an average of 6/10 was recorded (Table 1,2).
Table 2: The Mechanisms of Occurrence of the Accident.
Discussion
In this paper, we presented our attitude to manage an intraocular foreign body complicating an open globe injury. We proceeded to a simple technique with a classic core vitrectomy and extraction of the IOFB with a 20-gauge forceps. Eye injuries and IOFB, have been found to be common in the young, aged population and our finding attests this. We found that majority of patients with IOFB were young with mean age of 27.7 years and median of 28 years. This finding is similar to the findings of several authors [6]. the impact on visual acuity and visual function is severe. The Ocular Trauma Score (OTS) is a useful tool prior to surgical approach for predicting the visual prognosis; described by Kuhn and al. [7] in 2002. Surgically, many techniques are described in the literature [3,8-11]. The outcomes and prognosis factors have been studied also. The main risk factor of poor final visual acuity was a large size of the IOFB and the preoperative retinal detachment [12,13,14]. The timing and indications for Vitrectomy are also debated. We opted for immediate vitrectomy and extraction of the IOFB. Potential advantages of immediate IOFB removal include a possible decrease in risk of endophthalmitis [15], a decrease in the rate of proliferative vitreoretinopathy (PVR), and a single procedure for the patient [15]. Many surgical techniques for the extraction of IOFBs have been discussed in the literature. Yuksel and al. reported 36 patients with trauma related to IOFB using the “T” or “L” sclerotomy where the interval between accident and surgery was 14 days [16]. The extraction of IOFB without PPV can be possible as shown by Rusnak and al. where they reported 9 patients with IOFB removed through a transscleral incision using a magnet achieving a good visual acuity and there was no report of complications [17].
Conclusion
In conclusion, an intraocular foreign body poses a threat to the retina. Its extraction is mandatory; whatever the nature of the foreign body. The threat is greater in the case of a plant foreign body because of the risk of endophthalmitis. Extraction techniques are numerous and highly dependent on the skills of the retinal surgeon.
Disclosure Statement
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no finance.
Acknowledgement
None.
Conflict of Interest
No Conflict of Interest.
References
- Ozkaya A, Cakir I, Tarakcioglu HN (2019) The outcomes of bimanual posterior segment intraocular foreign body removal with vitrectomy and description of two different handshake techniques: A single surgeon case series. J Fr Ophtalmol 42(2): 109-117.
- Valmaggia C, Baty F, Lang C, Helbig H (2014) Ocular injuries with a metallic foreign body in the posterior segment as a result of hammering: the visual outcome and prognostic factors. Retina 34(6): 1116-1122.
- Dhoble P, Khodifad A (2018) Combined Cataract Extraction with Pars Plana Vitrectomy and Metallic Intraocular Foreign bodyremoval Through Sclerocorneal Tunnel Using a Novel "Magnet Handshake" Technique. Asia Pac J Ophthalmol (Phila) 7(2): 114-118.
- Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, et al. (2016) Intraocular foreign bodies:a review. Surv Ophthalmol 61: 582-596.
- Demircan N, Soylu M, Yagmur M, Akkaya H, Atakan Ozcan A, et al. (2005) Pars plana vitrectomy in ocular injury with intraocular foreign body. J Trauma 59(5): 1216-1218.
- Sharma S, Thapa R, Bajimaya S, Pradhan E, Poudyal G (2018) Clinical characteristics and visual outcome, prognostic factor, visual acuity and globe survival in posterior segment intraocular foreign body at Tilganga Institute of Ophthalmology. Nepal J Ophthalmol 10(19): 66-72.
- Kuhn F, Maisiak R, Mann L, Mester V, Morris R, et al. (2002) The ocular trauma score (OTS). Ophthalmology Clinics of North America 15(2): 163-165.
- Gonzalez-Cortes JH, Bages-Rousselon Y, Gonzalez-Cantu JE, Mohamed-Hamsho J (2017) Minimally Invasive surgery for the removal of posterior intraocula foreign bodies. J Ophthalmic Vis Res 12(2): 236-240.
- Guevara-Villarreal DA, Rodríguez-Valdés PJ (2016) Posterior segment intraocular foreign body: extraction surgical techniques, timing, and indications for vitrectomy. J Ophthalmol, pp.
- Singh R, Bhalekar S, Dogra MR, Gupta A (2014) 23-gauge vitrectomy with intraocular foreign body removal via the limbus: an alternative approach for select cases. Indian J Ophthalmol 62(6): 707-710.
- Öztas ¸ Z, Nalc¸acı S, Afrashi F, Erakgün T, Mentes J, Degirmenci C, et al. (2015) Posterior segment intraocular foreign bodies: the effect of weight and size, early versus late vitrectomy and outcomes. Ulus Travma Acil Cerrahi Derg 21(6): 496-502.
- Wani VB, Al-Ajmi M, Thalib L, Azad RV, Abul M, et al. (2003) Vitrectomy for posterior segment intraocular foreign bodies: visual results and prognostic factors. Retina 23(5): 654-660.
- Lam DS, Tham CC, Kwok AK, et al. (1998) Combined phacoemulsification, pars plana vitrectomy, removal of intraocular foreign body (IOFB), and primary intraocular lens implantation for patients with IOFB and traumatic cataract. Eye (Lond) 12(3): 395-398.
- Pavlovic S (1999) Primary intraocular lens implantation during pars plana vitrectomy and intraretinal foreign body removal. Retina 19(5): 430-436.
- Yeh S (2008) Current trends in the management of intraocular foreign bodies. Current Opinion in Ophthalmology 19(3): 225-233.
- Yuksel K, Celik U, Alagoz C, Dundar H, Celik B, et al. (2015) 23 Gauge pars plana vitrectomy for the removal of retained intraocular foreign bodies. BMC Ophthalmology 15: 75.
- Rusnak S, Kozova M, Belfinova S, Ricarova R (2009) Transscleral Extraction of an Intraocular Foreign Body without PPV, EVRS Meeting.
-
Hsouna Zgolli, Khalifa Alsawidi, Sonya Mabrouk, Gareeb Bagdadi, Chiraz Abdelhedi, et all. Management of Intraocular Foreign Bodies of Posterior Segment. W J Opthalmol & Vision Res. 4(1): 2022. WJOVR.MS.ID.000579. DOI: 10.33552/ WJOVR.2022.04.000579.
-
Pars plana vitrectomy, Visual morbidity, Blindness, Lifelong sequelae, Best corrected visual acuity, Peripheral vitrectomy, Traumatic accident, Ocular trauma score, Proliferative vitreoretinopathy
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






