 Case Report
Case Report
Kearns-Sayre Syndrome in A 27-Year-Old Male: A Case Report
Roquito Jose M Yutangco* and Roberto N Uy
Department of Ophthalmology, University of Santo Tomas Hospital, Philippines
Roquito Jose M Yutangco, Department of Ophthalmology, University of Santo Tomas Hospital, Philippines.
Received Date: July 19, 2021; Published Date: September 17, 2021
Abstract
Objective: To report a case of a 27-year-old patient who presented with progressive external ophthalmoplegia and ptosis along with pigmentary retinopathy, cardiac conduction abnormalities, and hearing loss.
Methods: Descriptive case report.
Results: We report a rare case of a patient who presented with progressive external ophthalmoplegia and ptosis. Upon further physical and diagnostic examination, he was also found to have pigmentary retinopathy, cardiac conduction abnormalities, and hearing loss, which are associated with his ophthalmologic signs and symptoms.
Conclusion: In conclusion, Kearns-Sayre Syndrome is an inherited mitochondrial myopathy characterized by chronic progressive external ophthalmoplegia, pigmentary retinopathy, and other non-ophthalmologic findings such as cardiac conduction abnormalities and hearing deficits. In a patient presenting with these ophthalmologic findings, it is important to also look out for associated cardiac and otologic abnormalities and manage these associated life-threatening conditions.
Keywords: Kearns-Sayre Syndrome; Chronic Progressive External Ophthalmoplegia
Introduction
Chronic Progressive External Ophthalmoplegia (CPEO) is an inherited mitochondrial myopathy characterized by slowly progressive, symmetric ophthalmoplegia with or without ptosis [1]. CPEO accompanied by pigmentary retinopathy, cardiac conduction abnormalities, and variably cerebellar ataxia, deafness, and elevated CSF protein levels, is known as Kearns-Sayre Syndrome (KSS). This syndrome was first described by Kearns and Sayre in 1958 when they reported 2 patients presenting with a triad of CPEO, retinitis pigmentosa, and complete heart block [2]. Up to date, only over 200 cases of Kearns-Sayre syndrome have been published, but the true incidence of the disease remains unknown [3]. Currently, the clinical diagnostic criteria of KSS includes the triad of progressive external ophthalmoplegia, pigmentary retinopathy, and onset before 20 years of age, plus at least one of the following: complete heart block, cerebellar ataxia, CSF protein levels above 1000 mg/L, short stature, hearing loss, and endocrine abnormalities [4,11]. We report a case of a 27-year-old male who only sought consult due to tearing of both eyes. Upon physical examination and diagnostic evaluation, he was found to have a cluster of signs and symptoms all pointing to Kearns-Sayre Syndrome.
Patient Information
The patient is a 27-year-old, male, Filipino, residing in Manila, Philippines, and working as a market vendor.
8 years, prior to consult, the patient started to note gradual progressive drooping of both eyelids. This was accompanied by gradual progressive difficulty in moving both eyes. No blurring of vision, double vision, history of trauma or ocular surgeries were reported. Interval history shows worsening / progression of symptoms, leading to complete inability to elevate the eyelids as well as complete inability to move eyes in all directions. The patient sought consult with the chief complaint of tearing and dryness of both eyes. Aside from his ophthalmologic complaints, he also complained of easy fatigability and difficulty hearing. No other family member was reported to have the same or similar complaints.
Physical Exam
Upon general physical examination, the patient was noted to have a short stature. Vital signs were under normal limits except for the heart rate which was significantly low at 41 beats per minute. Further cardiac examination revealed an irregular rhythm with the apex beat at the 6th intercostal space at the mid clavicular line. Upon ophthalmologic examination, visual acuity of the right eye was noted to be 20/40 uncorrected, not improved by pinhole, with a best correction of 20/30 (+0.50 sph = -0.75 cyl x 151), while visual acuity of the left eye was noted to be 20/100 uncorrected, improved to 20/40 on pinhole, with a best correction of 20/30 (+0.25 sph = -1.25 cyl x 100). No scotoma and metamorphopsia were noted on both eyes. Ptosis was noted on both eyelids (Figure 1) with the clinical measurements listed (Table 1).
On slip lamp examination, conjunctiva was slightly hyperemic on both eyes, with punctate epithelial erosions (PEE) noted inferiorly on cobalt blue filter (Figure 2). The rest of the external eye exam was unremarkable (Table 2).
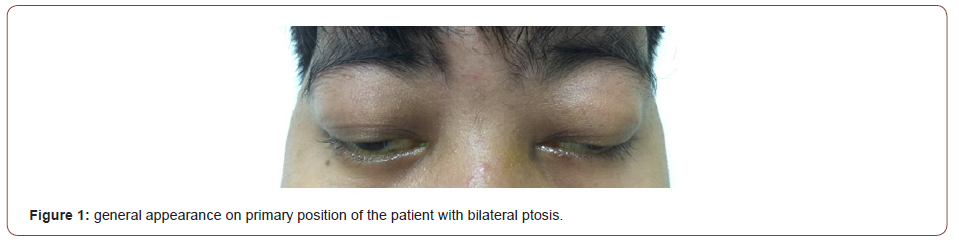
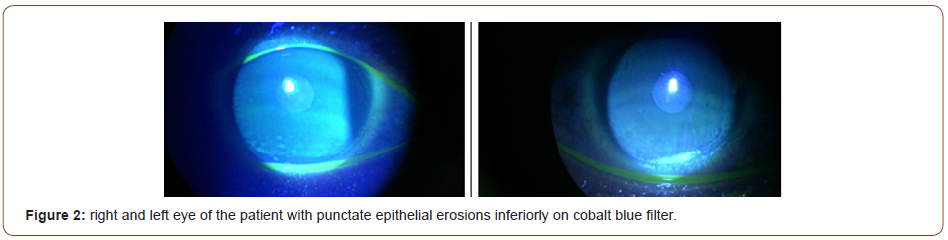
Table 1: Timeline.
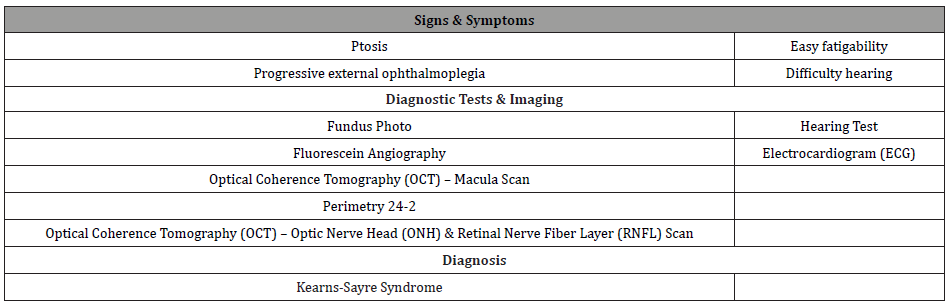
Table 2: Ptosis Data Collection Sheet.
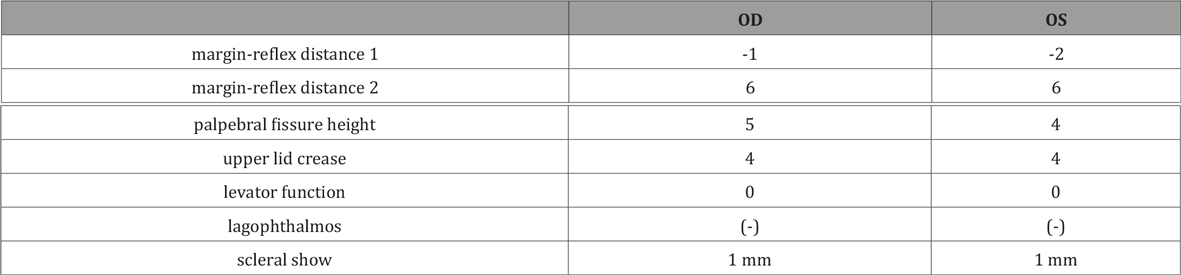
Table 3: External Eye Exam of the Patient.

Lacrimal irrigation was patent on both puncta with no discharge nor reflux noted, ruling out obstruction as the cause of tearing. Ocular motility examination showed severe limitation symmetrically on both eyes, with a clinical grade of -4 on all gazes (straight up, up and right, straight right, down and right, straight down, down and left, straight left, up and left) Figure 3. Forced duction test did not show any resistance / restriction, ruling out mechanical causes of ocular motility limitation (Figure 3). Intraocular pressure was within normal range at 18 on both eyes on applanation tonometry.

Diagnostic Assessment
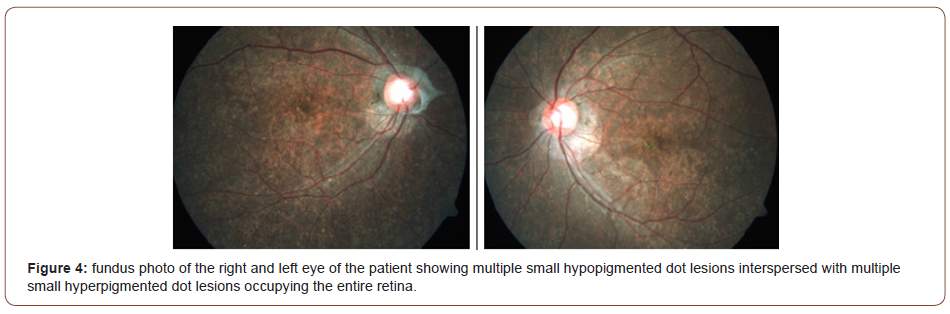
Fundus photo of the right eye was seen through a clear media, with distinct margins, cup-to-disk (CD) ratio of 0.8, peripapillary membrane and peripapillary atrophy inferior to the optic nerve head, arteriovenous (A: V) ratio of 2:3, dull foveal reflex with multiple hyperpigmented dot lesions over the fovea as well as multiple small hypopigmented dot lesions (white speckles) interspersed with multiple small hyperpigmented dot lesions occupying the entire retina. Fundus photo of the left eye was likewise seen through a clear media, with distinct margins, cup-to-disk (CD) ratio of 0.6, peripapillary atrophy, arteriovenous (A: V) ratio of 2:3, dull foveal reflex with multiple hyperpigmented dot lesions over the fovea as well as multiple small hypopigmented dot lesions (white speckles) interspersed with multiple small hyperpigmented dot lesions occupying the entire retina (Figure 4).
Fluorescein angiogram of the right eye with delayed dye transit noted at 24 seconds and laminar flow still evident at 25 seconds shows patchy choroidal filling. There are multiple pinpoint hyperfluorescences at the entire retina interspersed with hypofluorescent areas corresponding to the lesions seen at the colored fundus photo which did not increase in size and intensity in the late phases. Fluorescein angiogram of the left eye with first angiographic photo taken at 37 seconds with laminar flow still evident also shows patchy choroidal filling. There are likewise multiple pinpoint hyperfluorescences at the entire retina interspersed with hypo fluorescent areas corresponding to the lesions seen at the colored fundus photo which did not increase in size and intensity in the late phases (Figure 5).
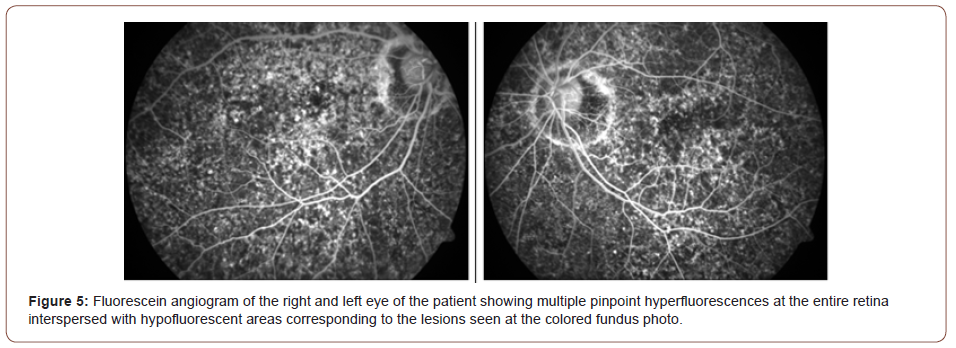

This fluorescein angiogram was signed out with the impression of RPE atrophic changes, both eyes, consider pigmentary retinopathy. In a study by Khambatta et al., they were able to identify 35 patients with KSS based on the clinical diagnostic criteria. Among those patients, they found that all patients had an ophthalmologic abnormality, i.e thirty-one (89%) had CPEO, thirty (86%) had ptosis, twenty-five (71%) developed pigmentary retinopathy [5] (Figure 6).
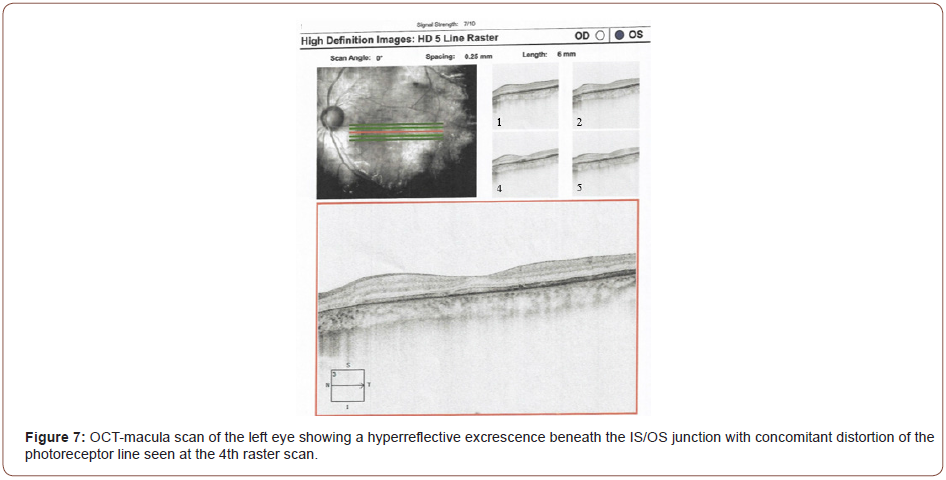
OCT scan of the macula of the left eye with a signal strength 7/10 likewise shows shallow (almost lost) foveal contour. There are no intraretinal cystic spaces seen. There is a hyperreflective excrescence beneath the IS/OS junction with concomitant distortion of the photoreceptor line seen at the 4th raster scan (Figure 7). ILM-RPE thickness map shows thinning of the entire macula with a central subfield thickness of 182 um (Figure 8).

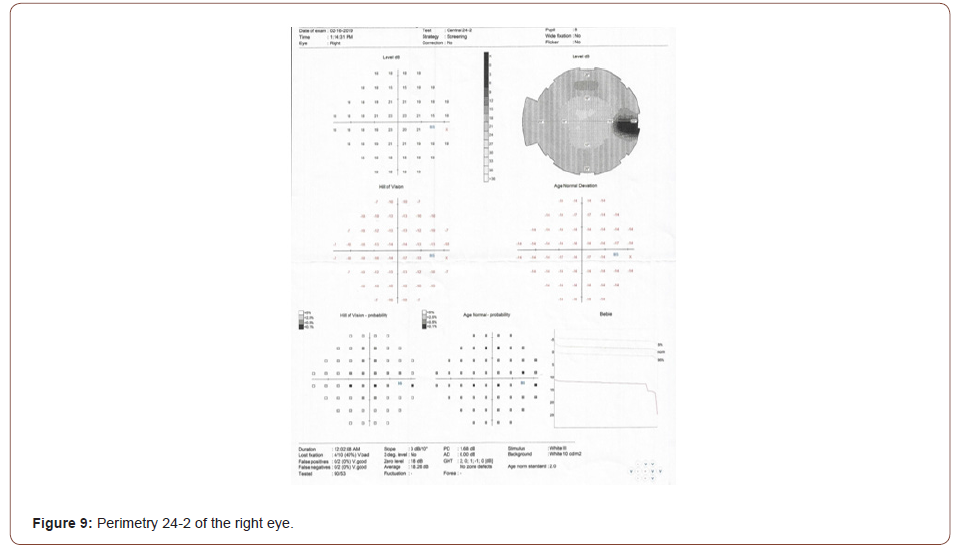
This OCT-macula scan was signed out with the impression of generalized macular thinning, both eyes. Perimetry 24-2 size III white stimulus on white background test of the right eye with a pupil size of 8 mm had elevated fixation losses and a severe generalized depression (Figure 9).
Perimetry 24-2 size III white stimulus on white background test of the left eye with no data on pupil size also had elevated fixation losses. There is a severe generalized depression with a cluster of mild paracentral defects (Figure 10).

The perimetry test was signed out as generalized depression of both eyes which may be due to media opacity or uncorrected refractive error, may be consistent with glaucomatous optic neuropathy, but other causes of visual field defects cannot be ruled out.
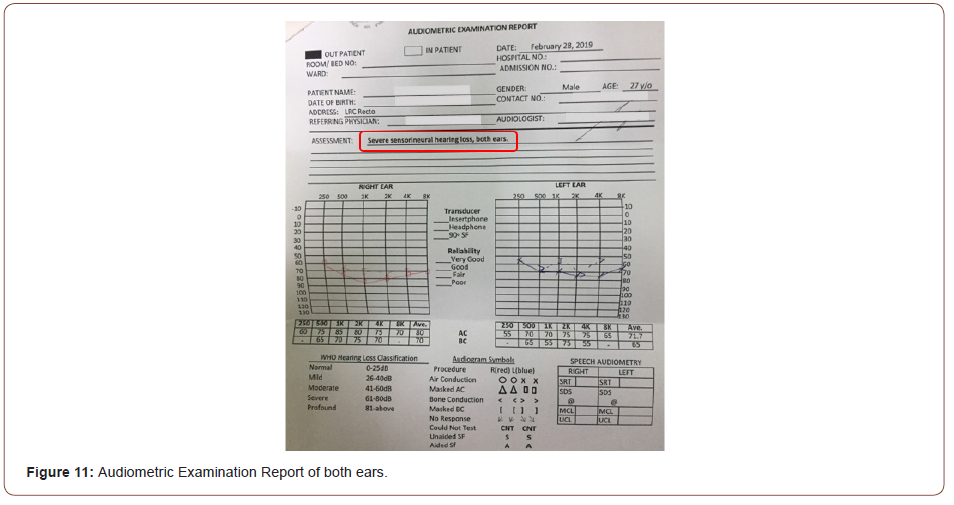
OCT scan of the optic nerve head (ONH) and retinal nerve fiber layer (RNFL) of the right eye shows a fair scan quality and average disk size. RNFL deviation map shows focal areas of thinning superior and inferior to the disk. Peripapillary RNFL thickness shows thinning on the superior and inferior quadrants. Rim area is thin. OCT scan of the optic nerve head (ONH) and retinal nerve fiber layer (RNFL) of the left eye also shows a fair scan quality and average disk size. RNFL deviation map shows focal areas of thinning inferior to the disk. Peripapillary RNFL thickness shows thinning on inferior quadrants. Rim area is likewise thin (Figure 11).

The results of the functional and structural test may be due to glaucomatous optic neuropathy, but other causes of visual field defects and retinal nerve fiber layer thinning cannot be ruled out. Interpretation of the OCT and perimetry studies were based on test printouts alone. If we correlate these tests with clinical data, the signs do not point to glaucomatous optic neuropathy e.g. RNFL thinning may be attributed to the generalized macular thinning. In a study by Zarnowski et al., they presented a case report on a patient diagnosed with KSS with normal tension glaucoma. However, they concluded that there is neither histological nor genetic evidence for the existence of an association between KSS and normal tension glaucoma, and it seems that mere coincidence of symptoms is more likely to explain this case [9].
The patient was also referred to the service of otorhinolaryngology where hearing test results done showed severe sensorineural hearing loss on both ears. In a study by Kornblum et al., they found that CPEO or KSS patients are at high risk of developing sensorineural hearing deficits, specifically due to mitochondrial DNA (mtDNA) deletion or A3243G point mutation (A3243G PM) [8]. That being said, hearing aids or cochlear implants may be considered as management for hearing loss in KSS. In another study by Oliveira et al., they recommended the use of a hearing aid and /or cochlear implant, together with speech therapy for auditory rehabilitation of KSS patients with hearing loss as they may bring beneficial results [7].
The patient was also referred to the service of internal medicine for further evaluation and management of his cardiovascular signs & symptoms, specifically his significantly low heart rate and easy fatigability. Electrocardiogram (ECG) testing showed the following results (Figure 12).

1. Complete heart block
2. Left ventricular hypertrophy
3. Right axis deviation
4. Intraventricular conduction delay, non-specific
5. Wandering atrial pacemaker with evidence of probable
sick sinus
6. Probable right ventricular hypertrophy
According to the American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines, a complete (3rd degree) heart block with or without symptoms falls under Class I indications for pacemaker implantation [6]. That being said, a pacemaker is considered necessary or beneficial for our patient, with his ECG findings of a complete heart block and easy fatigability. Even if with no indications based on guidelines, a prophylactic pacemaker may still be considered. Going back to the study of Khambatta et al. where they were able to identify 35 patients with KSS based on the clinical diagnostic criteria, four (11%) died among those patients, all of which due sudden cardiac events at a mean age of 46 years. In addition, Among those four patients, three (75%) had no ECG changes or symptoms indicating a need for a permanent pacemaker (PPM) / implantable cardioverterdefibrillator device (ICD). This study supports the possibility of considering a prophylactic PPM / ICD placement in patients diagnosed with KSS [5].
Interventions
No disease-modifying treatment is available for KSS at this time. Management is mainly supportive care for associated problems [10]. This includes hearing aids or cochlear implants for the sensorineural hearing loss and permanent pacemaker (PPM) / implantable cardioverter-defibrillator device (ICD) placement for the complete heart block in order to prevent adverse events.
Follow up and Outcomes
Although the patient can already be diagnosed with KSS based on the clinical diagnostic criteria, other diagnostic tests could be done in the future for documentation / educational purposes. These include skeletal muscle biopsy stained with Massons or Gomori trichrome which would exhibit “ragged red fibers” resulting from increased numbers of enlarged sub-sarcolemmal mitochondria, and Electron microscopy which would reveal increased numbers of abnormal mitochondria, appearing enlarged with disorganized cristae and paracrystalline inclusions [3]. These additional tests were not done previously due to financial constraints of the patient but would have further supported the diagnosis if present or positive.
Discussion
Kearns-Sayre Syndrome is an inherited mitochondrial myopathy characterized by chronic progressive external ophthalmoplegia, pigmentary retinopathy, and other non-ophthalmologic findings such as cardiac conduction abnormalities and hearing deficits. We hereby report a case of a 27-year-old male who presented with progressive external ophthalmoplegia and ptosis, the onset of which was noted about 8 years ago (19 years old), and pigmentary retinopathy. Along with these ophthalmologic signs and symptoms were cardiac conduction abnormalities and hearing loss, thus meeting the current clinical diagnostic criteria for Kearns-Sayre Syndrome. While there is no curative treatment at this time, management is focused on more life threatening and associated conditions such as cardiac conduction abnormalities.
Patient Anonymity, Consent and Confidentiality
Two printed informed consents were obtained from the patient for the writing and publication of this case report (See Appendix A & B and attached document). Both consents were written in English format, which according to the patient, can understand / comprehend. He was also informed that photos of the upper 1/3 of the face exposing the eyes and orbital area as well as diagnostic tests / images (fundus photos, fluorescein angiography, perimetry, optical coherence tomography, hearing test, and electrocardiography) will be included in this material. All personal information regarding the patient (name, geographic location, date of birth, contact number, etc.) will be kept confidential. Patient anonymity will be maintained when the study is for presentation or publication. A breach of confidentiality may occur if the information is used in any other way.
Ethics Approval
This case report has acquired granted approval from the Institutional Review Board of the University of Santo Tomas Hospital prior to presentation or publication of this material as required by our institution.
Acknowledgement
None.
Conflict of Interest
No conflict of interest relevant to this material was reported by the principal investigator which may interfere with the presentation and publication of this case report.
References
- Bhatti M Tariq (2018) Basic and Clinical Science Course Section 5, Neuro-Ophthalmology. San Francisco: American Academy of Ophthalmology.
- Kearns TP, Sayre GP (1958) Retinitis pigmentosa, external ophthalmoplegia, and complete heart block: unusual syndrome with histologic study in one of two cases. Arch Ophth 60(2): 280-289.
- Burkat KN (2019) Kearns-Sayre Ptosis.
- Yu M, Yu L, Wang ZX (2016) Diagnosis and Management of Kearns-Sayre Syndrome Rely on Comprehensive Clinical Evaluation. Chin Med J (Engl) 129(20): 2519-2520.
- Khambatta S, Nguyen D, Beckman T, Wittich C (2014) Kearns-Sayre syndrome: a case series of 35 adults and children. Int J Gen Med 7: 325-332.
- Dalia T (2019) Pacemaker Indications.
- Oliveira L, Brosco K, Oliveira E, Alvarenga K (2017) Cochlear implant in Kearns-Sayre syndrome: case study of twin sisters.
- Kornblum C, Broicher R, Walther E, Herberhold S, Klockgether T, et al. (2005) Sensorineural hearing loss in patients with chronic progressive external ophthalmoplegia or Kearns-Sayre syndrome. J Neurol 252(9): 1101-1107.
- Zarnowski T, Jaksch M, Rejdak R, Zagórski Z (2003) Kearns–Sayre syndrome, abnormal corneal endothelium and normal tension glaucoma. Acta Ophthalmol Scand 81(5): 543-545.
- Rohena L (2019) Kearns-Sayre Syndrome Treatment & Management.
- Clamp M, Burkat K, Lee N, Yen M (2020) Kearns-Sayre Ptosis.
-
Roquito Jose M Yutangco, Roberto N Uy. Kearns-Sayre Syndrome in A 27-Year-Old Male: A Case Report. W J Opthalmol & Vision Res. 3(5): 2021. WJOVR.MS.ID.000572. DOI: 10.33552/WJOVR.2021.03.000572.
-
Kearns-Sayre Syndrome, Chronic Progressive External Ophthalmoplegia, Cerebellar Ataxia, Endocrine Abnormalities
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






