 Case Report
Case Report
Early Postoperative Capsular Block Syndrome: Case Report
Claudia L Arellano-Martínez1*, René Dávila-Mendoza1, Juan M Paulin-Huerta1 and Andrew M Sorsby-Vargas2
1Ophthalmologist, Conde de Valenciana Eye Institute, Mexico City
2Intern doctor of the social service of the Faculty of Health Sciences of the Anahuac Mexico North University, Mexico
Claudia L Arellano-Martínez, Ophthalmologist, Conde de Valenciana Eye Institute, Mexico City, Mexico.
Received Date: June 22, 2022; Published Date: July 11, 2022
Abstract
Objective: To report a case of capsular block syndrome (CBS) 24 hours after phacoemulsification plus intraocular lens (IOL) implantation
without complications.
Observations: 78-year-old male with blurred vision after cataract surgery. Narrow anterior chamber is found with anterior displacement of the
iridolenticular complex, and retention of material in the capsular bag.
Results: Visual acuity of 0.2 logMAR, intraocular pressure 14mmHg, wide anterior chamber, centered IOL, in good position.
Conclusion: SBC is a rare complication of phacoemulsification. The diagnosis is fundamentally clinical and its treatment must be individualized.
Keywords: Capsular block syndrome; phacoemulsification; Intraocular lens; Viscoelastic; Residual myopia; Refractive errors
Introduction
Capsular block syndrome (BCS) is a rare complication of phacoemulsification. characterized by the accumulation of fluid within the capsular bag, between the lens intraocular lens (IOL) and the posterior capsule [1]. Its clinical manifestations are variable and include asymptomatic patients, with alterations in visual acuity, increased intraocular pressure and glaucoma [1]. Alterations in visual acuity are caused by two mechanisms: refractive changes (myopia) due to anterior displacement of the lens intraocular and/ or accumulation of retro lenticular white fluid, a phenomenon called lacteocrumenasia [1]. Capsular block is classified according to the time of its presentation. There are 3 different types: intraoperative, early postoperative, and late postoperative [2]. Postoperative capsular block syndrome (pBSC) represents a rare post-surgical complication [2]. According to different retrospective studies, the incidence of SBCp is approximately 0.73% [1]. Early SBCp is usually It presents from the first day to two weeks after surgery and its etiology is unknown with certainty. accuracy [3]. It has been reported that the presence of traces of viscoelastic material within the capsular bag generating a hyperosmotic gradient that attracts water, accumulates within the bursa, distends it and dislocates the IOL forward [3]. Early SBCp is usually accompanied by myopia, narrowing of the chamber angle, and increased pressure intraocular [3]. Cases are described in which this complication is associated with nystagmus or saccadic movements [3]. Within the first few days to weeks postoperatively, Patients generally suffer from low visual acuity due to induction of myopia [3]. A slit lamp inspection reveals a narrow anterior chamber, increased intraocular pressure, and the presence of clear fluid within the capsular bag [3]. We present the case of a patient with early pBSC.
Case Presentation
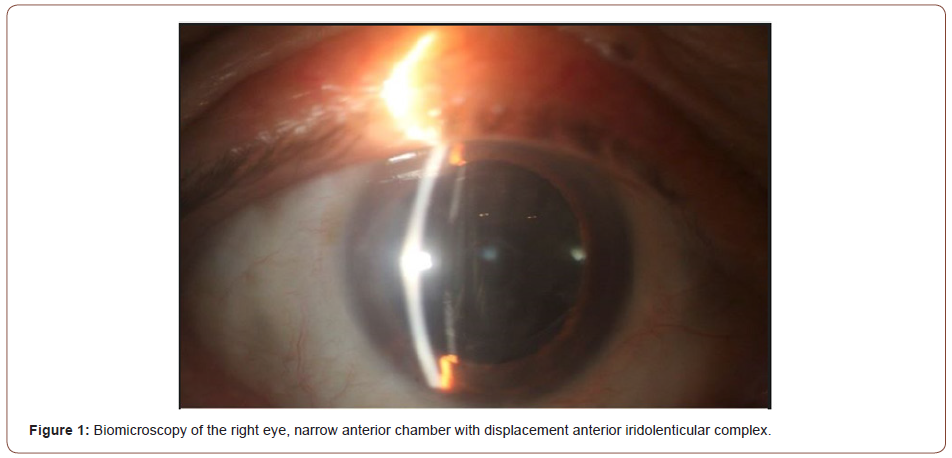
A 78-year-old male who comes to the clinic due to decreased visual acuity of predominance in the right eye of one month of evolution. Pathological personal history of oxygen-dependent chronic obstructive pulmonary disease and bladder cancer in remission. On ophthalmological examination we found visual acuity of the right eye (OD) 1.30 logMAR which improves to 0.2 logMAR with its correction and left eye (OS) 1 logMAR which improves to 0.1 logMAR with its correction. Subjective refraction OD +4.75= -0.50 x 60º and OS+4.00= -0.25 x 120º. Intraocular pressure 15 mmHg in both eyes. To RE biomicroscopy eyelids and annexes without alterations are found, transparent cornea with anterior chamber narrow, intact iris, round and reactive pupil, Gonioscopy with Shaffer II 270 angles degrees and 90 degrees Shaffer I. Crystalline with opacity, opalescence grade 3 and color grade 3 by LOCS III classification. Fundus of the eye presents applied retina, orange papilla with 45% excavation, dull macule, presence of drusen inside and outside 500 microns, periphery without predisposing lesions. The left eye has unaltered eyelids and annexes, a transparent cornea with a camera. narrow anterior, intact iris, round and reactive pupil, Gonioscopy with Shaffer II angles in all 4 quadrants. Crystalline with opacity, opalescence grade 2 and color grade 2 by LOCS III classification. Fundus of the eye presents applied retina, orange papilla with excavation 45%, dull macule, presence of drusen inside and outside 500 microns, periphery without predisposing lesions Optical coherence interferometry, IOL master, is performed, where an increase in the density of the lens in both eyes, predominantly in the right eye, axial length of the eye right 21.02 mm and LE 21.46 mm, anterior chamber depth of OD 2.32 mm and LE of 2.67 mm, increased lens AP axis RE 5.34 mm and LE 5.30 mm. Therefore, the diagnosis of senile cataract in both eyes, angle closure primary and dry age-related macular degeneration. Given the visual acuity and the angle closure, it was decided to start treatment in the right eye by phacoemulsification plus intraocular lens implant. The surgery was performed under sedation, pupil dilation with tropicamide - phenylephrine 50mg/ 8mg/ml. 2.2mm main port, trypan blue placement, dispersive viscoelastic, capsulorhexis 5.5 mm to the limbus, hydrodissection without complications, phacoemulsification, observes pupil with a tendency to miosis, intracameral adrenaline is placed with response partial to the medication, continued with aspiration of the cortex, placement of viscoelastic cohesive for placement of the lens in the capsular bag, IOL +29.00 is placed without complications, viscoelastic aspiration and suture placement are performed. At 24 postoperative hours, the patient reports blurred vision, visual acuity without correction of 0.5 logMAR, residual refraction of -1.75 diopters spherical and pressure intraocular pressure of 21 mmHg. Ophthalmologic examination reveals a formed anterior chamber, narrow, with anterior displacement of the iridolenticular complex, distension of the capsular bag with apparent retrolental fluid retention (Figure 1).
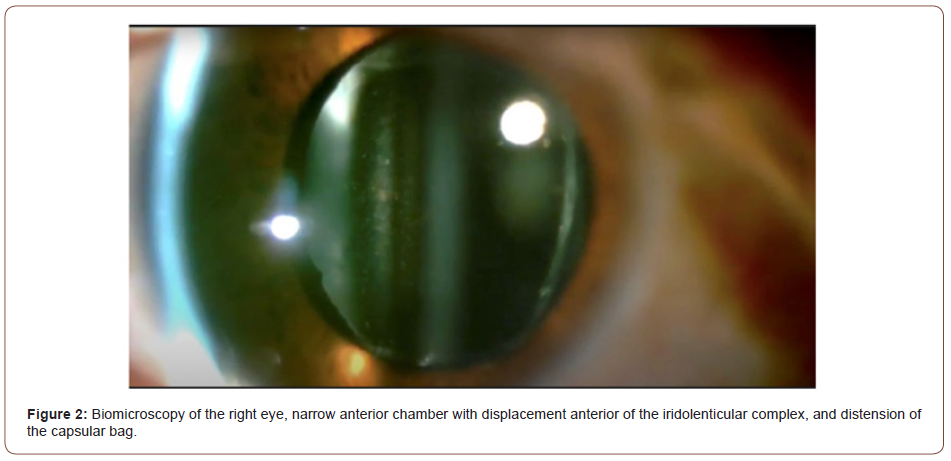
It is decided to keep under observation. A week after surgery, a decrease in visual acuity 1.0 logMAR, residual refraction of -2.50 diopters and intraocular pressure 22 mmHg, Biomicroscopy shows an increase in the distention of the capsular bag with apparent retrolental fluid retention (Figure 2).
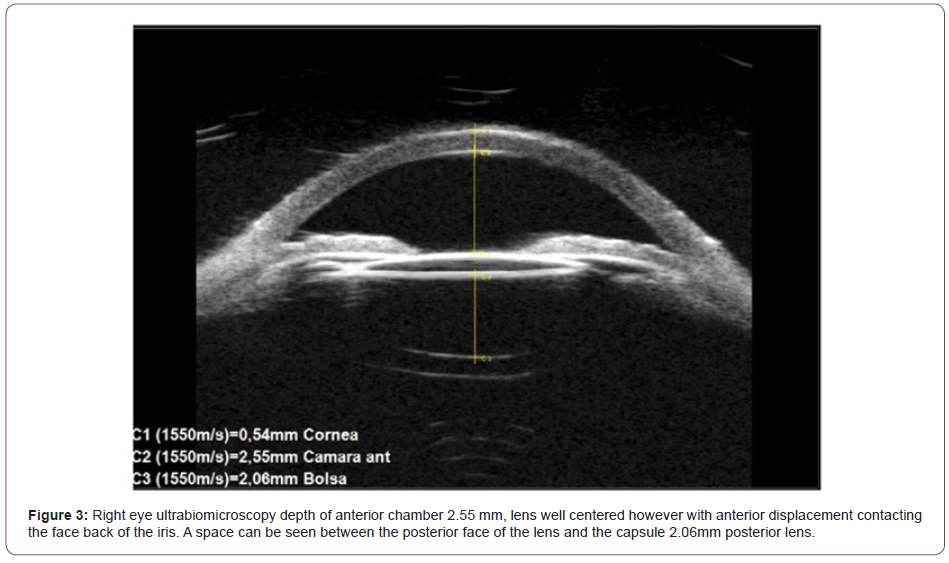
Optical coherence tomography (OCT) of the anterior segment and ultrabiomicroscopy were performed. where anterior chamber depth 2.55 mm is observed, lens well centered however with anterior displacement contacting the posterior aspect of the iris. There is a space between the posterior face of the lens and the posterior lens capsule of 2.06mm (Figure 3).
It is decided to perform a second surgical time to extract the material behind the IOL, proceeds to do it without complications, finding traces of viscoelastic material behind the intraocular lens. At the postoperative appointment, improvement in visual acuity of 0.2 is found logMAR, refraction of +0.25= -0.75 x 111º and intraocular pressure of 14 mmHg. To ophthalmological examination found anterior chamber formed and wide, intraocular lens centered and in good position, at 30 days he presents visual acuity of 0 logMar with pressure intraocular pressure of 12 mmHg.
Discussion
In 1990 and 1992, Davidson and Holtz were the first to publish descriptions of the syndrome [5,6], while Masket used the term capsular block syndrome due to first time [7]. In 1998, Miyake classified the SBC into 3 types depending on their play time. appearance and its pathophysiology [8]. BCS is classified as intraoperative, postoperative early and late postoperative [8]. Intraoperative capsular block syndrome (CiBS) It occurs at the time of hydrodissection and is associated with rupture of the posterior capsule. The proposed mechanism of SBCi dictates that during hydrodissection a nucleus with large dimensions is brought into contact with a small diameter capsulorhexis, forming a chamber behind the core where the solution used during the procedure collects [2] causing a posterior capsule rupture. The proposed mechanism of the SBCp dictates that the close relationship between the IOL and the capsulorhexis create a chamber between the IOL and the capsule posterior that can be distended by retaining fluid. (two). In the cases of Davidson and Holtz, reported the accumulation of clear fluid between the IOL and the posterior capsule just after IOL implantation [5]. Sugiura et al. hypothesize that the chamber formation between the IOL and the posterior capsule, distension of the posterior capsule and alterations myopic lesions in early SBCp are caused by entrapment of viscoelastic in the chamber formed by the IOL and the capsulorhexis (diameter of the capsulorhexis being less than that of the IOL), creating an osmotic gradient in which the aqueous humor produced distends the posterior capsule [9]. Kim and Shin reported that age and gender do not represent value significant in incidence, however, the main risk factor for developing SBCp Early is an anteroposterior eye length greater than 25mm. One was proposed different classification of SBCp, dividing into non-cellular, inflammatory and fibrous [6]. The Noncellular SBC is characterized by presenting within the first 24 hours of postoperative [6]. Biomicroscopy usually shows an IOL with anterior displacement with accumulation of clear fluid in the capsular bag [1]. The Noncellular SBC is secondary to retention of viscoelastic material [1]. The SBC inflammatory is described as an inflammatory reaction in the anterior chamber and exudate fibrinoid in the pupillary margin, usually occurs days after surgery [1]. The SBC fibrotic is characterized by fibrosis of the margin of the capsulorhexis and opacification of the posterior capsule [1]. Fibrotic BCS is caused by cell proliferation and metaplasia. epithelial cells of the lens and occurs in the late postoperative period [1]. The diagnosis is fundamentally clinical and is based on the findings in biomicroscopy. (Anterior displacement of the IOL and the irido-lenticular diaphragm) [2]. Similarly in In some cases, intraocular pressure may increase as a result of displacement. of the IOL [2]. Various treatments have been described from expectant management to reoperation [10]. Expectant management has been associated with acute angle glaucoma closed, chronic inflammation in the anterior chamber and opacification of the posterior capsule [10]. Anterior capsulotomy can be performed with YAG laser, however, there is a risk of release the viscoelastic into the anterior chamber and thus causing an increase in pressure intraocular, in the same way there is a risk of traumatizing the iris causing a posterior hemorrhage or synechiae [10]. Similarly, a capsulotomy can be performed. posteriorly, releasing the viscoelastic into the vitreous cavity where its effects seem minimal [10]. Posterior capsulotomy can be difficult as the capsulotomy lens is designed for depth focus of a normal IOL, not in the mid-vitreous [10]. Finally, you can intervene and aspirate the contents of the distended posterior capsule, which which increases the risk of introducing microorganisms to the eye [10]. The best treatment is prevention by completely aspirating all viscoelastic after IOL insertion. In the case of our patient, he presented an early SBCp secondary to entrapment of viscoelastic, which underwent a surgical intervention to aspirate the material, as well as improving your visual acuity and intraocular pressure.
Conclusion
BCS is a rare complication of phacoemulsification characterized by accumulation of fluid within the capsular bag, between the intraocular lens (IOL) and the posterior capsule. Patients may develop visual acuity disturbances, suffer increased intraocular pressure or even be asymptomatic. The main risk factor is Anteroposterior ocular length greater than 25 mm. Diagnosis is essentially clinic by slit lamp biomicroscopy, however today we have different tools such as ultrabiomicroscopy and OCT of the anterior segment that help confirm the diagnosis. Treatment varies from expectant to interventional surgery, so each case must be analyzed and individualized.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Vélez M, Velásquez LF, Rojas S, Montoya L, Zuluaga K, et al. (2014) Capsular block syndrome: a case report and literature review. Clin Ophthalmol 8: 1507-1513.
- Ibañez-Hernández MÁ, Navarro-Partida J, González-de la Rosa A (2011) Syndrome of Capsular block: a case report and review of the literature. Rev Mex Oftalmol 85(4): 196-200.
- Lorente R, Mendicute J (2008) Lens surgery. (1st), Spanish Society of Ophthalmology pp. 1682-1686.
- Pinarci EY, Bayar SA, Sizmaz S, Canan H, Yilmaz G (2012) Late capsular block syndrome presenting with posterior capsule opacification. J Cataract Refract Surg 38(4): 672-676.
- Davison JA (1990) Capsular bag distension after endophacoemulsification and posterior chamber intraocular lens implantation. J Cataract Refract Surg 16(1): 99-108.
- Holtz SJ (1992) Postoperative capsular bag distension. J Cataract Refract Surg 18(3): 310-317.
- Masket S (1993) Postoperative complications of capsulorhexis. J Cataract Refract Surg 19(6): 721-724.
- Miyake K, Ota I, Ichihashi S, Miyake S, Tanaka Y, etal. (1998) New classification of capsular block syndrome. J Cataract Refract Surg 24(9): 1230-1234.
- Sugiura T, Miyauchi S, Eguchi S, Obata H, Nanba H, et al. (2000) Analysis of liquid accumulated in the distended capsular bag in early postoperative capsular block syndrome. J Cataract Refract Surg 26(3): 420-425.
- Sorenson AL, Holladay JT, Kim T, Kendall CJ, Carlson AN (2000) Ultrasound measurement of induced myopia associated with capsular bag distention syndrome. Ophthalmology 107(5): 902-908.
-
Claudia L Arellano-Martínez, René Dávila-Mendoza, Juan M Paulin-Huerta, Andrew M Sorsby-Vargas. Early Postoperative Capsular Block Syndrome: Case Report. W J Opthalmol & Vision Res. 4(2): 2022. WJOVR.MS.ID.000583. DOI: 10.33552/WJOVR.2022.04.000583
-
Capsular bag, Refractive changes, Asymptomatic patients, Narrow anterior, Reactive pupil, Trypan blue placement, Dispersive viscoelastic
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






