 Complementary
Complementary
Corneal Transplantation Today. Giving Patients A Better Quality of Life
Cesar Gomezperalta*
Department of eye Surgeon, Senior Consultant Eye Surgeon Vision Percepcion, Mexico
Cesar Gomezperalta, Department of eye Surgeon, Senior Consultant Eye Surgeon Vision Percepcion, Mexico.
Received Date: March 26, 2019; Published Date: April 15, 2019
Complementary
Corneal transplant has been around for many years, the first one done more than a 100 years ago. Although the principle is the same, exchanging unhealthy, distorted, opaque or decompensated tissue for a healthy one, thanks to the evolution, knowledge in Medicine, higher technology and the need for more successful results, corneal transplant has reached a very specialized status.
With Penetrating Keratoplasty or Lamellar Keratoplasty the cornea can be exchanged in a partial or total way depending on the patient‘s pathology. In developed countries lamellar surgery is the gold standard for corneal transplant and in developing countries penetrating keratoplasty is still done in large numbers. The full thickness exchange of the cornea, the penetrating keratoplasty, is performed for pathologies in which most or all of the cornea is altered being opaque, scared or decompensated. It is a very good procedure, although endothelial rejection and open eye surgery complications can occur. Also, as endothelium is replaced, durability is an issue and a new transplantation may be necessary years after.
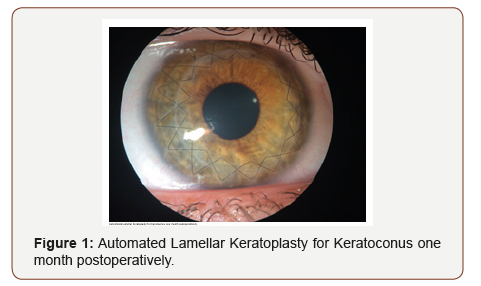
On the other hand, partial thickness exchange, lamellar keratoplasty, can be performed anteriorly or posteriorly. Anterior Lamellar Keratoplasty, removes scars, alterations in shape such as Keratoconus and transparency issues. You can remove up to 95% of the anterior tissue. It can be done manually, with microkeratomes or femtosecond lasers. It gives great visual results, has no endothelial rejection and the graft can last a lifetime. Posterior Lamellar Keratoplasty or Endothelial Keratoplasty was developed to remove only the abnormal or deficient endothelium. Different techniques have been presented and aimed for minimal invasive surgery, damage less and less the grafted tissue and fast visual recovery. It may also have endothelial rejection and other complications.
In many countries of the world corneal transplant still has social and religious considerations. There is still tabu about receiving someone else’s part of the eye and donation issues are still complicated. What it is a fact, is that patients that have been transplanted they recover functionality, quality of vision and what it is more important, quality of life. Patients with low vision due to corneal pathology stop working, stop doing daily life activities and has a very negative impact on their lives. In a study done at our clinic (Vision Percepcion - Mexico City, Mexico), one hundred transplanted patients for Keratoconus that depended 100% in glasses or contact lenses to function and partially do their life, work and activities, recovered not only good vision much less dependent on the use of a correction, but most of them without glasses could do their work, hobbies and normal life. Corneal transplant is not a surgery to remove glasses but when restoring corneal architecture other procedures may be performed to help patients see without them. This corrective procedure includes laser, phacoemulsification and intraocular lenses on their various modalities (Figure 1).
Conclusion
In conclusion, corneal transplant is a very accurate and repeatable surgery to restore vision in patients with anterior segment pathology.
Acknowledgment
None.
Conflicts of Interest
No Conflicts of interest.
-
Cesar Gomezperalta. Corneal Transplantation Today. Giving Patients A Better Quality of Life. W J Opthalmol & Vision Res. 1(4): 2019. WJOVR.MS.ID.000519.
-
Corneal transplant, Corneal pathology, Quality of vision, Endothelial Keratoplasty, lamellar, Keratoplasty, Analyzing information, Visual health, Commercial prejudices, Ophthalmology, Optometry, Visual science.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






