 Research Article
Research Article
A Comprehensive Study on the Causes of Low Vision and Effective Management Strategies at BSMMU Low Vision Clinic
Aysha Siddika Mukta1*, Syed Mohammad Didarul Alam2, Syed Abdul Wadud3 and Shams Mohammad Noman4
1Aysha Siddika Mukta, optometry officer, Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
2Syed Mohammad Didarul Alam, optometrist, Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Syed Abdul Wadud, Professor & Chairman, Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
4Shams Mohammad Noman, Associate Professor, Department of Ophthalmology Bangabandhu Sheikh Mujib Medical University (BSMMU) Hospital, Bangladesh
Aysha Siddika Mukta, Optometry officer, Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Received Date:April 04, 2025; Published Date:May 20, 2025
Abstract
Background: The BSMMU Low Vision Clinic (Bangabandhu Sheikh Mujib Medical University) has been providing essential low vision care and
management. Identifying the major causes of low vision and the most prescribed low-vision devices will help to develop and implement the lowvision
rehabilitation service.
Methodology: A retrospective cross-sectional overview of total 200 patients were observed at BSMMU low vision clinic between January’ 2021
to December’ 2022.
Results: This study at the BSMMU Low Vision Clinic revealed prevalent causes of low vision, including uncorrected refractive error, diabetic
retinopathy, cataract and glaucoma. A total of 200 patients were observed. The mean age was 32.53 ± 22.90 years. There was statistically no significant difference between the mean age in either sex; p-value=1.00. Female were sufferings more with low vision then male. Refractive error & amblyopia 40 (20%) was the leading cause of low vision, followed by Diabetic Retinopathy 31(15.5%), Cataract 28(14%), Glaucoma 21(10.5%), Retinitis
Pigmentosa 17(8.5%), Optic atrophy 14(7%), ARMD 12 (6%), Pathological Myopia 9(4.5%), Maculopathy 7(3.5%), Retinal detachment 6(3 %),
Nystagmus 5(2.5%), keratoconus 5(2.5%), CRVO 3(1.5%), Corneal Dystrophy 2(1%) respectively. Low vision caused by glaucoma was significantly
corelated with increasing age. We prescribed Optical aids 157(78.50%) and non-optical aids 39(19.50%). Interventions were mainly Spectacles,
Magnifiers, telescopes, closed circuit television (CCTV), orientation and mobility counselling and referral to the social welfare department for Visual Impairment Certificate.
Conclusion: Refractive error, Diabetic retinopathy and cataract were the predominant causes of low vision, and magnifiers and telescopes were
the most prescribed low vision devices.
Keywords: Low vision; Refractive error; Cataract; Telescope; Magnifier
Highlights: Refractive Error with Amblyopia, Diabetic Retinopathy, Cataract are the leading causes of Low vision
The risk of Low vision in children is greater than in adults & most of the patients were working age group
Low vision due to glaucoma upgraded markedly with increasing age.
The most prescribed optical low-vision device was telescope & magnifier and most of the patients prefer to use magnifier rather than telescopes.
Introduction
Low vision is a major public health issue that affects people from all over the world. Globally, Millions of people are struggling with low vision, which has an enormous impact on their independence and quality of life. According to the World Health Organization, “A person with low vision is one who has best corrected visual acuity in his/her better eye is less than 6/18 to light perception, or a visual field of less than 10 degrees from the point of fixation.” Low vision is a condition that cannot be improved with surgery, medication, glasses, or contact lenses. To address these challenges and improve the lives of those affected, the management of low vision requires a multidisciplinary approach, including accurate diagnosis, personalized rehabilitation, and the use of assistive technologies.
According to WHO (2020) Globally, 2.2 billion people suffer from a near- or distance vision impairment. It is estimated that globally, 36% of individuals with refractive have distance vision problems and 17% of adults suffer vision impairment due to cataract have had access to an appropriate intervention [1]. Age-related macular degeneration (AMD), glaucoma, and diabetic retinopathy are the main causes of blindness in developed countries. In the rest of the world, Cataracts (47%) are the main factor of visual impairment [2]. Nearly 90% of the world’s visually impaired people live in low-income countries. One-third of the global blind resided in South Asia, 2015. The prevalence of blindness in South Asia was 0.7%. Similarly, 61.2 million people in South Asia have moderate and severe visual impairment, which accounts for 28.2% of the global magnitude [3]. Globally, the top four causes of visual impairment are uncorrected refractive errors, cataract, age-related macular degeneration (AMD) and glaucoma. Therefore, 80% of all visual impairments are avoidable. The Southeast Asia Region, including Bangladesh, is estimated that 90.5 million people are visually impaired and 12 million are blind adults [4]. The most recent study in Bangladesh conducted by IAPB,2022 showed that prevalence of blindness is 1% aged over 40 and blindness is 1% overall population. The rate of blindness is higher in female than male [5]. In the context of Bangladesh, where visual impairment is a growing public health concern, the Bangabandhu Sheikh Mujib Medical University (BSMMU) Low Vision Clinic plays a vital role in providing essential services to individuals with low vision. This research endeavor aimed to conduct a comprehensive study focused on the underlying causes of low vision among the patient served by the BSMMU Low Vision Clinic.
Methods
Study Design and Participants:
In this retrospective cross sectional study, we reviewed the medical records of low vision patients who had been referred by Ophthalmologists for low vision services. At the Low Vision Clinic, patients were re-examined to confirm that they had low vision and were suitable for low vision devices. Subjects were taken as a low vision patient according to WHO, whose visual acuity was less than 6/18 with correction. The visual acuities of all patients was determined using a LogMAR chart (with letters and tumbling E chart), color vision with ishihara and contrast sensitivity with Pelli-robson chart. All patients were refracted for near and distance and best corrected visual acuities were recorded. Patients with best corrected visual acuities of less than 6/18 but better than light 3/60 in the better were considered for low vision devices. Clinical records of low vision patients managed at the BSMMU Hospital between January’ 2021 to December’ 2022. The sample size was 200. Inclusion criteria were a diagnosis of vision impairment and availability of complete records. We extracted the following data from each record: age, sex, education level, employment status, chief complaints concerning vision, associated ocular diseases, uncorrected distance and near visual acuities, best-corrected distance and near visual acuities, statuses of previous and current prescribed optical devices, and cooperation status of patients during the optometric examination.
Data Collection Tools and Technique:
Different kinds of data collection techniques used for the study, such as demographic information, relevant history, clinical examination data were collected from recorded sheet. The clinical data were collected with the help of a well-designed data collection format. Visual Acuity was recorded with LogMAR Acuity Chart, Refractive Status were determined by Retinoscopy, Anterior Segment examined by slit lamp, and Posterior Segment examined by 90 D, indirect ophthalmoscope.
Data Analysis plan:
All quantitative data was processed using SPSS version 23, statistical package with the help of Microsoft office (excel and excess). Both univariate and bivariate analysis was done to describe and show relationships. Interpretation of qualitative data was done under guidance of a senior researcher. Graphs, Charts and Tables were used for easy understanding of the findings.
Results
Gender distribution with Low vision
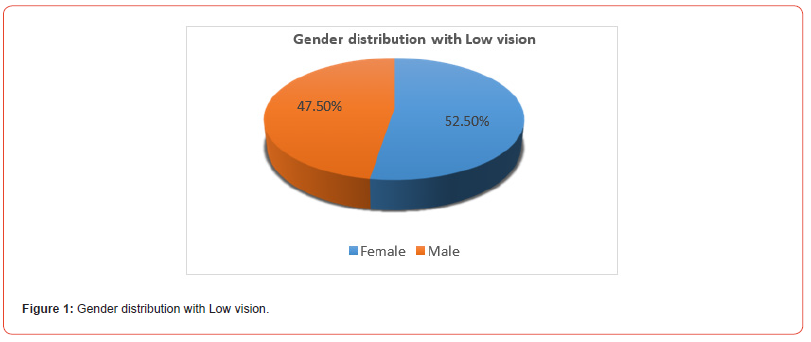
Our study included total 200 subjects to see the causes of low vision in these patients and difficulties. In which 105 (52.5%) were females and 95 (47.5%) were males (Figure 1). Female were more sufferings with low vision than male. Figure 1
Age/sex distribution of patients with low vision
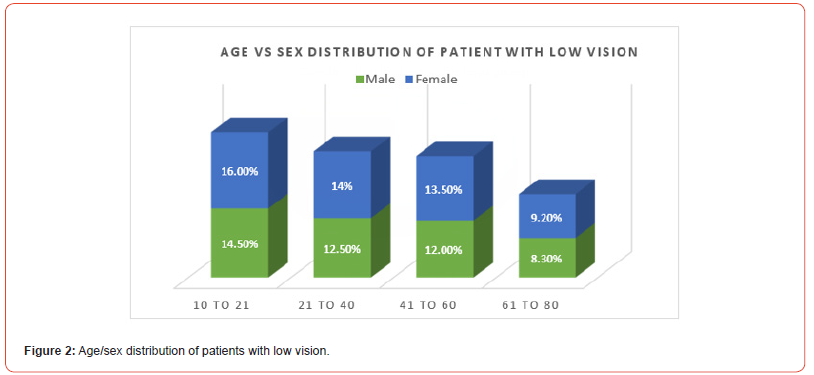
In this study, according to age ranging from 10-21 (30.5%), 21- 40 (26.5%), 41-60 (25.5%) and 61-80 (17.50%). It is concerning that the age group 10 to 21 low vision patient was more and it gradually decreased with increasing age. The mean age of the patients was 32.53 ± 22.90 years, with a range of 10-80 years. The mean age of the female was 34.05 ± 22.85 years while that of male was 28.69 ± 22.89 years. (Pearsons’ Chi-Square test, p < .05)
Causes of Low Vision
Our study we found that, the most common causes of low vision is Refractive Error and Amblyopia 40 (20%), Diabetic Retinopathy 31(15.5%), Cataract 28 (14%), Glaucoma 21 (10.5%), Retinitis pigmentosa 17(8.5%), Optic atrophy 14(7%), ARMD 12 (6%), Pathological Myopia 9(4.5%), Maculopathy 7(3.5%), Retinal detachment 6(3 %), Nystagmus 5(2.5%), keratoconus 5 (2.5%), CRVO 3 (1.5%), Corneal Dystrophy 2 (1%) (Table 1). The mean age was 41.56 ± 28.79 years (ranging from 10 to 80) in the cataract group, and the mean age of the RP group was 38.9 ± 18.89 years (ranging from 11 to 70). Age was significantly correlated with an increase in low vision from glaucoma. The mean age of the amblyopic patients was 19.81 ± 7.19 years ranging from 10 to 35, and the mean age was 65.83 ± 12.23 years ranging from 40 to 80 in the patient group having ARMD. The mean age of the Diabetic Retinopathy patient was 57.43 ± 10.56 Age ranging from 40 to 80.
Table 1:Causes of Low Vision.
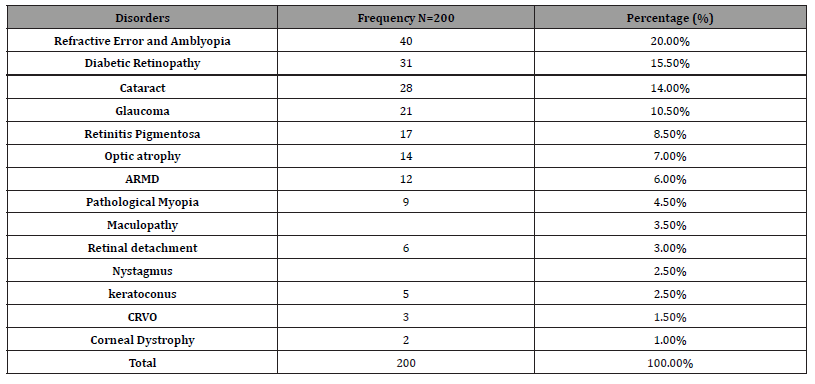
*Data were as expressed frequency and percentage.
Functional Vision Assessment
Functional vision component was also assessed. Patients with decrease visual acuity recorded were 37.5%, contrast sensitivity 18.5%, color vision 60.9%. 100% patient were suffering from distance vision problem. 40.5% patient were near vision problem. 59% patient were night vision problem. 83.8% patient were day vision problem. 82.5% patient were glare problem and 55.0% patient were mobility problem.
Visual and refractive status
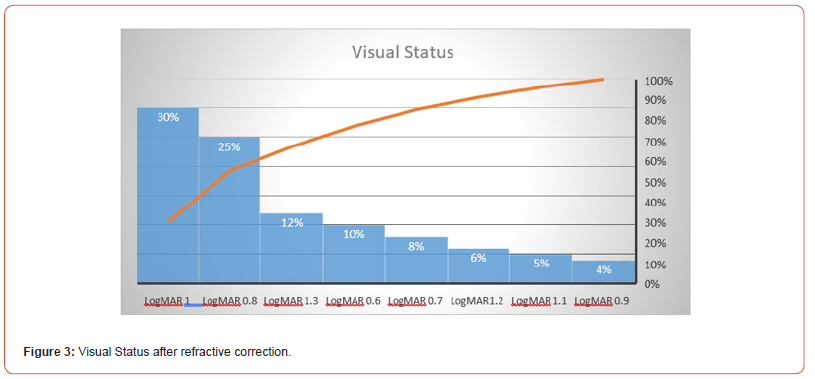
In this study, 145 (72.5%) had refractive errors and 81 (55.86%) were myopic. The mean refractive error was -3.50 (SD ± 4.15), and the range of better eyes was (-0.50 to -20.00 D). Their average visual acuity was 0.90 LogMar (sd ±0.21). Among these, about 64 (44.14%) patients were hyperopic mean refractive error +3.25 (SD ±3.83D) in the better eye with visual acuity of 0.95 LogMar (SD ±0.23) (Figure 3). The mean Visual Acuity Log MAR 0.95 (sd ±0.21) in the better eye with mode 1.00 logMAR; 30% had visual acuity 1.0logMAR and 25% had 0.80logMAR (Figure 3). Almost two-third of the low-vision patients seen had some amount of refractive error. Visual acuity can be improved by spectacle correction in many lowvision patients.
Optical & Non-Optical devices of low vision
Glasses were prescribed for 130 (65.00%) patients with dioptric power ranging from +12.0D to -22.0D. Telescopes were prescribed for 35 (17.5%) patients. Mean telescopic magnification was 3.5 X (sd: ±0.75, range 2X to 6X). Handheld and stand magnifiers were prescribed for 60 (30 %) with mean power 3.0X (sd: ±1.56, range 2X to 8X) (Table 2) After conventional spectacles, telescopes and magnifiers were the most commonly prescribed optical low-vision device in this study. Multiple devices were also prescribed for several cases.
Table 2:Optical & Non-Optical devices of low vision.
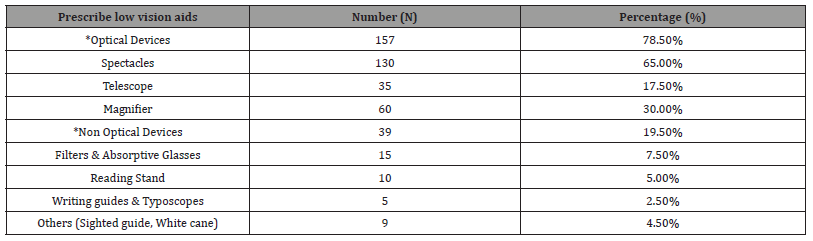
*Multiple Responses were included. Multiple devices were prescribed for some cases.
Intervention Given to low vision patient:
In this study, we prescribed optical aids about 157 (78.50%) and non-optical aids for 39 (19.50%). Patients who were visually impaired and had best corrected vision in their better eye <6/60, were given Visually Impairment Certificate from the BSMMU Low Vision Department. It’s about 35 (17.50%), and we referred them to the social welfare department for VI card. We issued letters to the school about 27 (13.50%) students who are studying currently and about 10 (5.00%) for students who are legally blind; we referred them to the school for blind education. We also referred them about 57 (28.50%) for orientation and mobility (O & M) training center to use their remaining vision and other senses to learn techniques and skills and survive in any environment for the rest of their lives.
Table 3:Intervention Given to low vision patient.
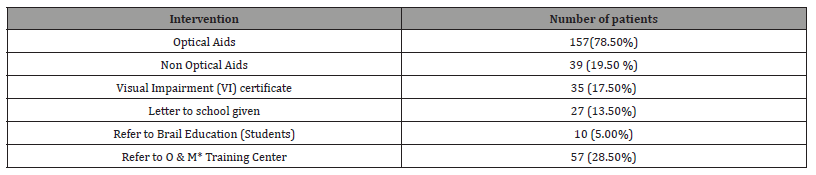
*O & M = Orientation and Mobility Training.
Discussion
The BSMMU Low Vision department is providing low vision rehabilitation service for those patient who referred from Retina clinic, Cornea clinic, Glaucoma Clinic, Pediatric Ophthalmology clinic, Neuro Ophthalmology clinic and others Hospital. The present study we studied 200 subjects and found females were 52.5% more sufferings with low vision than male (47.5%). The similar proportion was also observed in a Survey of Blindness in Saki East, Oyo State, Nigeria;2022 [6]. Most of the visually impaired patients treated at this study were of working age. In a study conducted at the low-vision clinic of Nepal Eye Hospital, the similar finding was observed [7]. Future research should identify the possible causes of sufferings with low vision more females than male and barriers with accessing low-vision services. Our results also suggest that women suffer from vision problems earlier than men. More than half are women (53. 96%) belonged to the age group from 10 to 30, while only two-thirds of the men (35. 97%) belonged to this age group. Approximately two-thirds of the visually impaired patients we treat are under the age of 50, which corresponds to active working age. which is a major challenge for our society. Which is similar with previous study. They observed females get low-vision problems earlier than males: more than half of the females (58.97%) were in the age group 0-20 years but only one-third of the males (30.61%) were in this age group [7].
In this study we found the most common causes of low vision is Refractive Error & Amblyopia 20%, Diabetic Retinopathy 15.5%, Cataract 14.0% and Glaucoma 10.5%. This results indicate uncorrected refractive error, that subsequently leads to refractive amblyopia is a prime cause of low vision, which can be avoidable cause. Which is consistent with previous study. They found Refractive Error (68.3%) is the prime cause of low vision [6]. In a study conducted 2003 in Bangladesh, the main causes of low vision were cataract (74.2%), refractive error (18.7%), and macular degeneration (1.9%). Cataract was the predominant cause (79.6%) of bilateral blindness followed by uncorrected aphakia (6.2%) and macular degeneration (3.1%) [8]. However, in our study, we observed that the most common cause of low vision is uncorrected refractive error (20%), which is due to increasing rate of cataract surgery. We also observed, Diabetic Retinopathy (15.5%) is the second leading cause of low vision. it is also an alarming issue, because most people are unconscious of Diabetic Retinopathy. They eventually lose their vision, and the rate is rapidly growing. In order to prevent vision loss, it is essential to identify and treat diabetic retinopathy as soon as possible. Cataract (14.0%) and Glaucoma (10.5%) were also identified as significant causes of low vision. But in several study found cataract (34.1% to 79.6%) was the predominant causes of low vision [2,8,9,7,10,11]. In our study other causes are Retinitis pigmentosa 8.5%, Optic atrophy 7%, ARMD 6%, Pathological Myopia 4.5%, Maculopathy 3.5%, Retinal detachment 3%, Nystagmus 2.5%, keratoconus 2.5%, CRVO 1.5%, Corneal Dystrophy 1%. The similar findings were also observed in several study [2,9,12,13,14,11,7].
Telescopes and magnifiers were the most frequently prescribed optical low-vision device in this study after traditional eyeglasses. We prescribed spectacles about 65%, telescope 17.5% and magnifier 30% of patients. Patients who were prescribed both telescope and magnifier, most of the patient interested to use magnifiers rather telescope. Because of near work give the most priorities then distance work. This is similar to the results of some other study, where the most frequently prescribed low-vision devices were non-illuminated hand magnifiers, illuminated hand magnifiers and illuminated stand magnifiers [15, 16]. However, our results differ from other studies [12,17,18]. and a university-based clinic in the UK where most of the prescribed low vision devices are telescope [19]. These difference are likely to most of the patients in our clinic are working age group. Patient who had not improve with optical aids, non-optical devices such as Filters & Absorptive Glasses 7.50%, Reading Stand 7.50%, Writing guides & Typoscopes 2.50% were prescribed.
The BSMMU Low Vision Department issued Visually Impairment Certificates for individuals who were visually impaired. We referred them to the social welfare department for a VI card (17.5%). We also provide letter to school 13.50%, and referred for brail education 5.0%. In order to train the patient’s orientation and mobility training, we also referred them to rehabilitation center. so that they might learn how to survive. However, there are not enough blind rehabilitation centers in Dhaka City. So the government should draw attention and establishes more rehabilitation centers for the blind in the country. According to the current study’s findings, patients with low vision feel that their functional status and quality of life are significantly degraded. To properly understand the results of lowvision services, vision-targeted health status questionnaires may be helpful in addition to the clinical assessment. Results from study showing a connection between low-vision services and improved functional status and quality of life may raise public awareness of the potential advantages of low-vision services and persuade Medicare and managed care plans to cover such treatments. We predict that increasing access to low-vision services will result from confirmation of the quantifiable profits in visual function [20-24].
Conclusion
We evaluated patients with low vision at the BSMMU hospital and prescribed low vision aids. About two-thirds of the patients with low vision who were seen under 50 and most of them were working age. Compared to men, women sufferings more with low vision. Appropriate refraction and spectacles play an essential part in the management of low vision patients. Most low vision patients saw significant improvements in their eyesight while using a telescope and magnifier. Due to the number of low vision patients is increasing, this service should become more accessible and affordable. More Ophthalmologists and Optometrists should be trained for low vision services, and regular training for advancing low vision management is also recommended.
Authors contribution
[Syed Mohammad Didarul Alam (SMDA), Syed Abdul wadud
(SAW), Shams Mohammad Noman (SMN), Mohammad Alauddin
(MA)].
Conception & Design:
SAW, SMDA.
Acquisition, analysis and interpretation of data:
SMDA, MA. Manuscript drafting and revising it critically: SAW,
SMN, SMDA. Approval of the final version of manuscript: SAW, SMN,
SMDA, MA, Guarantor accuracy and integrity of the work: SAW
Acknowledgments
The authors would like to express the most profound gratitude to all of the low vision patients whose data were used in this study and also thankful to the low vision unit.
Funding
None.
Conflict of Interest
The author declares no conflict of interest.
Ethical approval
Ethical approval wasn’t taken, due to hospital recorded data was used.
References
- World health organization. Blindness and vision impairment. fact sheet, 2011.
- Aggarwal R (2015) Double vision: Making eye care through cross-subsidization. France: Insead.
- Bourne RRA, Flaxman SR, Braithwaite T, Cincinelli MV, Das A, et al. (2017) Magnitude, term poral trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health 5: e888-897.
- World Health Organization.
- Shawkat Ara Shakoor, Mustafizur Rahman, AHM Enayet Hossain, Mohammad Moniruzzaman, Mahfuzur Rahman Bhuiyan, et al. (2022) Prevalence of blindness and its determinants in Bangladeshi adult population: results from a national cross-sectional survey. 12(4): e052247.
- Olusegun Adetomiwa Adediran, Tunji Sunday Oluleye, Olutoke Omolara Ayorinde, Mary Ogbenyi Ugalahi, Caleb Damilep Mpyet (2022) Survey of Blindness in Saki East, Oyo State, Nigeria. J West Afr Coll Surg 12(1): 41-47.
- Kishor Sapkota, Douk Hoon Kim (2017) Causes of low vision and major low-vision devices prescribed in the low-vision clinic of Nepal Eye Hospital, Nepal. Anim Cells Syst (Seoul) 21(3): 147-151.
- BP Dineen, R RA Bourne, SM Ali, DM Noorul Huq, GJ Johnson (2003) Prevalence and causes of blindness and visual impairment in Bangladeshi adults: results of the National Blindness and Low Vision Survey of Bangladesh. Br J Ophthalmol 87: 820-828.
- Fashe Markos Cherinet, Sophia Yoseph Tekalign, Dereje Hayilu Anbesse, Zewdu Yenegeta Bizuneh (2018) Prevalence and associated factors of low vision and blindness among patients attending St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. BMC Ophthalmol. 18(1): 232.
- Lingam Vijaya, Ronnie George, Rashima Asokan, Lokapavani Velumuri, Sathyamangalam Ve Ramesh (2014) Prevalence and causes of low vision and blindness in an urban population: The Chennai Glaucoma Study; Indian J Ophthalmol 62(4): 477-481.
- Vinay Nangia, Jost B Jonas, Ronnie George, Lingam Vijaya (2018) Prevalence and causes of blindness and vision impairment: Magnitude, temporal trends and projections in South and Central Asia. Br j Ophthalmol 103(7): 871-877.
- Gudlavalleti VS Murthy (2017) Eye care in South Asia, 1988-2018: developments, achievements and future challenges. Community Eye Health 30(100): 99-101.
- Konstantinos Oikonomidis, Stavroula Almpanidou, Persefoni Talimtzi, Angeliki Kakavouti Doudou, Spyridon M Metaxas, et al. (2023) Compliance with the Use of Low-Vision Aids in a Greek Population: An Explorative Study. cureus 15(7): e42730.
- Crossland MD, Silver JH (2005) Thirty years in an urban low vision clinic: changes in prescribing habits of low vision practitioners. Optom Vis Sci 82: 617-622.
- Lindsay J, Bickerstaff D, McGlade A, Toner A, Jackson AJ (2004) Low vision service delivery: an audit of newly developed outreach clinics in Northen Ireland. Ophthalmic Physiol Opt. 24(4): 360-368.
- Wolffsohn JS, Cochrane AL (1999) The changing face of the visually impaired: the Kooyong low vision clinic’s past, present and future. Optom Vis Sci 76(11): 747-754.
- Kansakar I, Thapa HB, Salma KC, Ganguly S, Kandel RP, et al. (2009) Causes of vision impairment and assessment of need for low vision services for students of blind schools in Nepal. Kathmandu Univ Med J 7(25): 44-49
- Van Rens GH, Chmielowski RJ, Lemmens WA (1991) Results obtained with low vision aids. A retrospective study. Doc Ophthalmol 78: 205-210.
- Leat SJ, Rumney NJ (1990) The experience of a university-based low vision clinic. Ophthalmic Physiol Opt 10(1): 8-15.
- Ahmed M (2018) Universal Eye Health Critical to Achieving SDG-3: Good Health and Well-Being of People. Retrieved from Universal-Eye-Health-Critical-to-Achieving-SDG3:-GoodHealth-and-WellBeing-of-People.
- Burton MJ, Ramke J, Marques AP, Bourne RR, Congdon N, et al. (2021) The Lancet Global Health commission on Global Eye Health: vision beyond 2020. Lancet Glob Health 9(4): e489-e551.
- Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 9(2): e144-e160.
- Jashim Uddin Ahmed, Sadeq Ahmed, Asma Ahmed, Mohammad Abdul Majid (2019) Caring Vision: Fighting Against Blindness in Bangladesh. FIIB Business Review 8(1): 17-24.
- Rita de cássia ietto, Montilha, Keila MiriaM, Monteiro de carvalho, Maria elisaBete Rodrigues, et al. (2014) Optical and nonoptical aids for reading and writing in individuals with acquired low vision. Arq Bras Oftalmol 77(2): 91-104.
-
Aysha Siddika Mukta*, Syed Mohammad Didarul Alam, Syed Abdul Wadud and Shams Mohammad Noman. A Comprehensive Study on the Causes of Low Vision and Effective Management Strategies at BSMMU Low Vision Clinic. W J Opthalmol & Vision Res. 5(2): 2025. WJOVR.MS.ID.000608.
-
Low vision, Visual impairment, Macular degeneration, Vision problems, Surgery, Blindness, Optometric examination, Visual acuity, Glaucoma
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






