 Case Report
Case Report
Placenta Percreta Presenting as an Acute Abdomen in Second Trimester of Pregnancy: Case Report from Middle East
Ahmad Talal Chamsi* and Abdullah S Alshehri
Department of Obstetrics and Gynecology, Security Forces Hospital City, Saudi Arabia
Ahmad Talal Chamsi, Department of Obstetrics and Gynecology Security Forces Hospital, P.O. Box 3643, Riyadh 11481, Saudi Arabia.
Received Date: October 03, 2018; Published Date: October 05, 2018
Abstract
Abnormal Placentation carries life-threatening consequences to the mother. Placenta percreta is a rare complication of pregnancy. It occurs mostly in the third trimester and presents with severe postpartum hemorrhage and placenta retention. It is rare in the second trimester of pregnancy. Placenta percreta is becoming more common as cesarean section and other uterine surgeries increase. The presence of a uterine scar remains a major risk factor. Clinical presentation is variable with Antepartum hemorrhage is a usual scenario. However, it is usually seen in the third trimester. The presentation here is rare since it occurred in the second trimester rendering clinical suspicion difficult as was evident in the case. We here present a rare presentation of placenta percreta occurring in the second trimester as an acute abdomen secondary to uterine rupture and intraabdominal hemorrhage. She had a life-saving total hysterectomy and good postoperative recovery period. This might be the first case to be presented from Middle east with such scenario. Careful evaluation of a pregnant lady with an acute abdomen must be done with consideration of abnormal placentation as a cause, especially in a patient with risk factors for abnormal placentation.
Keywords: Placenta; Percreta; Accreta; Previa; Increta; Pregnancy; Second Trimester; Acute abdomen
Introduction
Abnormal Placentation carries life-threatening consequences to the mother. Several types of abnormal placentation exist (Accreta, Increta, and Percreta). The different types vary depending on the degree of myometrial involvement. The accreta type is most common and easier to manage. The increta and percreta varieties are less common, difficult to manage and associated with severe maternal morbidity and mortality as a result of postpartum hemorrhage [1].
Placenta percreta is a rare complication of pregnancy. It occurs mostly in the third trimester and presents with severe postpartum hemorrhage and placenta retention. It is rare in the second trimester of pregnancy. Although the diagnosis is almost always clinical, however clinical diagnosis can be difficult. Both ultrasound and magnetic resonance imaging (MRI) may have misleading results. The diagnostic confirmation is histological, based on the absence or poor development of the basal layer of the endometrium [2]. Placenta percreta is becoming more common as cesarean section and other uterine surgeries increase. The presence of a uterine scar remains a major risk factor [2]. We here present a rare presentation of placenta percreta occurring in the second trimester as an acute abdomen. This case demonstrates how an unusual presentation can be well managed with multidisciplinary cooperation between obstetricians, vascular surgeons, urologist, Anesthesiologist and Intensivist. This might be the first case to be presented from Middle east with such scenario. Careful evaluation of a pregnant lady with an acute abdomen must be done with consideration of abnormal placentation as a cause, especially in a patient with risk factors for abnormal placentation.
Case Description
A 45 years old G4P3+0 Saudi lady at 22 weeks gestation presented to Security Forces Hospital Emergency Department with acute onset of Abdominal Pain that started few hours prior to presentation. Patient has sought medical advice in a private hospital and diagnosed as an acute appendicitis. The patient has left the private hospital and presented to Security Forces Hospital for another opinion. The pain had progressively increased in intensity and was associated with nausea and vomiting. Her pas medical history included hypothyroidism on Levothyroxine. Previous surgical history included 3 low transvers cesarean deliveries.
On presentation, the patient’s blood pressure was 90/52, her heart rate was 120bpm, Oxygen Saturation was 98% in room air, examination revealed diffuse abdominal tenderness. Pelvic Bedside scan revealed a single viable intrauterine pregnancy going with 22 weeks. Abdominal Ultrasound was not conclusive, so a decision was made for diagnostic laparoscopy to rule out appendicitis.
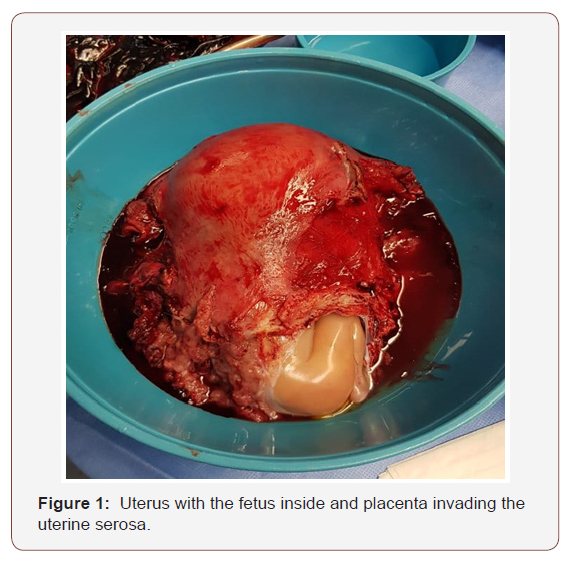
The laparoscopy scope revealed an abdomen full of blood. The surgeons converted to laparotomy. A Midline supra-umbilical incision was made but they did not find the source of bleeding. Vascular surgeon has joined the surgical team as the primary surgeons has suspected a rupture aneurysm. They extended the abdominal incision below the umbilicus and surgeons saw the source of bleeding. It was a uterine rupture just above the bladder and bleeding coming from the placenta. Obstetricians and Gynecologists were called and joined the procedure and a decision for hysterectomy was made. It was a challenging hysterectomy as the pelvis was full of blood, the placenta has invaded of the lower segment and part of the bladder, left broad ligament and the upper vagina, and the tissue are very fragile to be held by clamps. Vascular surgeons while doing bilateral internal iliac artery ligation, the right ureter was injured. After the hysterectomy was complete, a piece of the placenta was left attached to the upper vagina, with no bleeding (Figure 1). Urologist did ureter reimplantation and bladder repair. Abdomen was irrigated with 6 liters normal saline and hemostatic agents were placed, hemostasis was achieved. Patient was shifted to intensive care unit. She received a total of 12 Packed Red Blood Cells, 12 Units of Platelets, and 12 Units of Fresh Frozen Plasma. Her Hemoglobin dropped intra op to 4 g/dl. Her post-operative, post transfusion hemoglobin was 9 g/dl. She had an uneventful postoperative recovery period.
Discussion
Placenta percreta is characterized by the invasion of the chorionic villi through the myometrial and serosal layer of the uterus, typically in the absence of normal decidualized endometrialstroma. This absence of the decidua basalis leads to a clinically adherent placenta. Uterine instrumentation, previous cesarean section, and other procedures causing myometrial scarring all increase the risk of abnormal placentation [1, 2]. The incidence of abnormal placentation is relatively low, and demographic data about it is limited to small series and case reports [1]. The average incidence is estimated at 1 in 7000 deliveries [2]. Placenta percreta represents 5 to 7% of all abnormal placentation [3,4]. Even though rare and difficult to diagnose, it remains very important because of its possible fatal outcome with a reported maternal mortality rate of 2 to 7% [5,6]. The diagnosis is even more difficult when this occurs in the second trimester as was the case in our patient. However, the presence of a previous classical scar and her age were risk factors for the disease.
Though the cause of placenta percreta as reported by Morken et al. [7] is unknown, several risk factors have been associated with this condition notably, placenta praevia, a previous caesarean section, multiple pregnancies, a history of dilatation and curettage, high parity and increasing maternal age. The patient therefore had some risk factors as noted above and the placenta was found adherent to the previous scar, a finding that was not known to us as the patient was unbooked in our hospital. A previous scar is a major risk factor as the decidua basalis in this zone is expected to be poorly vascularized and presents as a zone of weakness for subsequent placental villi penetration [1].
Clinical presentation is variable with Antepartum hemorrhage is a usual scenario [8]. However, it is usually seen in the third trimester. The presentation here is rare since it occurred in the second trimester rendering clinical suspicion difficult as was evident in the case. Other reports indicate that placenta percreta can present as an acute abdomen [7] or even painless hematuria following bladder invasion [9].
Several diagnostic modalities may facilitate the antepartum diagnosis of abnormal placentation. These include transvaginal and trans- abdominal ultrasound with color imaging, and magnetic resonance imaging (MRI). Finberg et al [10] reported a sensitivity of 94% and a specificity of 79% for prenatal ultrasound in diagnosing the morbid placenta adhesion. One Bedside ultrasound was done for our patient, nevertheless the diagnosis was missed. This was probably due to the inexperience of the ultra sonographer, a factor which greatly prejudices the antepartum diagnosis.
The management of placenta percreta follows one of two options, radical surgery (hysterectomy) or conservative management [11]. Traditionally, abdominal hysterectomy is the treatment of choice for placenta percreta and indicated in cases of severe hemorrhage [7].
Though the conservative approach is believed to carry a higher risk of maternal death it preserves fertility and provides some psychological support to the woman [6]. It involves either of the following procedures: leaving the placenta in place with packing; a piecemeal blunt dissection with packing; uterine curettage with packing; closing of the uterine defect; localized excision and uterine repair; uterine packing with uterine or even hypogastric artery ligation; bilateral uterine artery embolization; and pelvic artery ligation [6,12,13]. Our patient had the radical approach due to the severe bleeding that she had, and it was a life-saving surgery.
The major complication of placenta percreta is severe bleeding. This can be associated with hypovolemic shock and subsequent death. Post-operative infection as was the case in our patient remains pertinent and life threatening. O’Brien et al. [6] reported a 28% post-operative infection rate. Other complications include uterine rupture, coagulation problems, invasion of adjacent organs, uterine inversion following manual placental removal, formation of fistulae, and of course the loss of reproductive functions.
The follow up of patients managed for placenta percreta involves strict surveillance and prompt management of complications. If it is suspected that part of the placenta is left in place, the patient would require follow up to ensure placental tissue resolution. This would involve regular clinical and ultrasound assessment and βhCG assay.
Conclusion
Placenta percreta, though a rare entity, remains a very serious clinical problem due to its life and fertility threatening consequences. Its antepartum diagnosis can be suspected based on risk factors and the clinical presentation of the patient. Its management remains difficult, but total abdominal hysterectomy with loss of fertility remains the treatment of choice especially in our case. However, conservative management may be used for minor forms of the disease (placenta acreta and increta). Such a decision must take into consideration the age of the woman, the extent of damage to the uterus, the gestational age and associated medical conditions such as diabetes, immuno-depression, cardiac and renal disorders.
Ethical Approval
Given the nature of the article, the management of the patient was not modified by the study, so it was considered exempted from IRB approval.
Patient had an informed consent for the management and permission for using the data for research study if needed.
Conflict of Interests
Author said no Conflict of Interest.
References
- Armstrong CA, Harding S, Dickinson JE (2004) Clinical aspects and conservative management of placenta accreta. The Obstetrician and Gynaecologist 6: 132-137.
- Veenstra MJ, Spinder T, Dekker GA, Van Geijn, HP (1995) Post-partum intra-abdominal hemorrhage due to placenta percreta. European Journal of Obstetrics and Gynaecology and Reproductive Biology 62: 253-256.
- Breen JL, Neubecker R, Gregori CA, Franklin JE Jr (1977) Placenta accreta, increta, and percreta. A survey of 40 cases. Obstet Gynecol 49(1): 43-47.
- Pridjian G, Rich NF, Montag AG (1990) Pregnancy hemoperitoneum and placenta percreta in a patient with previous irradiation and ovarian failure. Am J Obstet Gynecol 162(5): 1205-1206.
- Aboulafia Y, Lavie O, Granovsky-Grisaru S, Shen O, Diamant YZ (1994) Conservative surgical management of acute abdomen caused by placenta percreta in second trimester. Am J Obstet Gynecol 170(5 Pt 1): 1388-1389.
- O’Brien JM, Barton JR, Donaldson ES (1996) The management of placenta percreta: conservative and operative strategies. Am J Obstet Gynecol 175(6): 1632-1638.
- Morken NH, Henriksen H (2001) Placenta percreta--two cases and review of the literature. Eur J Obstet Gynecol Reprod Biol 100(1): 112- 115.
- Cox SM, Carpenter RJ, Cotton DB (1995) Placenta percreta: ultrasound diagnosis and conservative surgical management. Obstetrics and Gynecology 71(3): 454-456.
- Price FV, Resnik E, Heller KA, Christopherson WA (1991) Placenta previa accreta involving the urinary bladder: a report of two cases and review of the literature. Obstet Gynecol 78(3 Pt 2): 508-511.
- Finberg HJ, Williams JW (1992) Placenta accreta: prospective sonographic diagnosis in patients with placenta praevia prior to caesarean section. J Ultrasound Med 11(7): 333-343.
- Ophir E, Tendler R, Odeh M, Khouri S, Oetinger M (1999) Creatinine kinase as a biochemical marker in the diagnosis of placenta increta and percreta. Am J Obstet Gynecol 180(4): 1039-1040.
- Harika G, Gabriel R, Napoleone C, Quereux C, Wahl P (1994) Placenta percreta with bladder invasion: surgical strategy to avoid massive blood loss. Eur J Obstet Gynecol Reprod Biol 57(2): 129-131.
- Lee LC, Lin HH, Wang CW, Cheng WF, Huang SC (1995) Successful conservative management of placenta percreta with rectal involvement in a primigravida. Acta Obstet Gynecol Scand 79(10): 839-841.
-
Ahmad T C, Abdullah S A. Placenta Percreta Presenting as an Acute Abdomen in Second Trimester of Pregnancy: Case Report from Middle East. W J Gynecol Women’s Health. 1(1): 2018. WJGWH.MS.ID.000505.
-
Percreta; Accreta; Previa; Increta; Pregnancy; Second Trimester; Acute abdomen; Postpartum; Ultrasound; Magnetic resonance imaging (MRI); Endometrium; Cesarean; Uterine scar; Gestation; Nausea; Hypothyroidism; Levothyroxine; Intrauterine; Supra umbilical.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






