 Research Article
Research Article
Knowledge, Attitudes and Practices About Contraception in Patients who had Undergone A Caesarian Section in N’Djamena Mother and Child University Hospital
Gabkika Bray Madoué1*, Foumsou Lhagadang1, Saleh Abdelsalam2 and Hinsoubé Guelo2
1N’Djamena Mother and Child University Hospital, Chad
2N’Djamena faculty of health human sciences, Chad
Gabkika Bray Madoué, Department of genecology and obstetrics, N‘Djamena Mother and Child University Hospital, Chad.
Received Date:February 22, 2021; Published Date: March 12, 2021
Summary
Background: Postpartum contraception is the set of methods designed to prevent pregnancy after a caesarean section [1]. It can be instituted during the caesarean section or in the post-partum period.
The aim of this study is to evaluate the knowledge and practice of contraception in patients who have undergone a caesarean section at N’Djamena Mother and Child University Hospital.
Patients and method: This were a 3-month cross-sectional and descriptive study from September 1st, 2020 - November 30th, 2020 on knowledge, attitudes and practices about contraception in caesarian section patients.
Results: The 20-24 age group was the most represented with 42%.Patientts resided in N’Djamena in 60%.Married women were the most represented with 93.3% . Patients had average knowledge about contraception in 77.3%. Injectable contraceptives were the commonly known of the modern contraceptive methods with 80.7%. Periodic abstinence was the best-known natural method with 61.3%. Implants were the most chosen contraceptive method with 48%. The proposal to use the contraceptive method was made in 79 , 3% of cases by health workers. The most well-known advantages of contraceptives by clients were birth spacing with 82.7%. Infertility was the contraceptive method disadvantage most reported by clients with 54%.
Conclusion: The prescription of contraceptive methods in patients who have undergone a caesarean section is part of our common practice. Injectable contraception remains the commonly known hormonal contraception. The desire to avoid pregnancy is the benefit most noted by patients.
Keywords: Contraception; Caesarean section; NMCUH
Introduction
Postpartum contraception is the set of methods designed to prevent pregnancy after a caesarean section [1]. It can be instituted during the caesarean section or in the post-partum period. There is a disparity in the rate of use of contraceptive methods around the world. The rate of modern contraceptive use is 55% worldwide, reaching 22% in Africa with a rate less than 10% in its central part [1,2]. These disparities in contraceptive use rates also exist between urban and rural areas. For example, high rates can be observed in urban areas compared to rural areas. In Chad, according to data from the 2015 mixed survey, the prevalence of modern contraception is less than 5% for all women of childbearing age [3]. Foumsou L, et al [4] in a hospital series at N’Djamena Mother and Child University hospital in 2016 reported that the rate of contraceptive use in the post-partum period is 15.9%. However, several factors such as social and cultural factors are involved in the use of contraceptives. Few data exist on contraception after Caesarean section in our context. The aim of this study is to evaluate the knowledge and practice of contraception in patients who have undergone a caesarean section at N’Djamena Mother and Child University Hospital.
Patients and Methods
This was a three (3) month cross-sectional and descriptive study from September 1, 2020 - November 30, 2020 on knowledge, attitudes and practices about contraception in caesarian section patients.
Patients were interviewed. According to the answers given during the interview, the knowledge of the patients is classified as follows:
Average knowledge = knowledge of contraceptive methods or their effects.
Good knowledge = knowledge of contraceptive methods and their effects
The data was entered using Word and Excel 2014 software and analyzed using SPSS 18.0.
Results
Age
Area of origin: Patients resided in N’Djamena in 60% of cases (n=90) (Table 1).
Table 1: Age distribution.
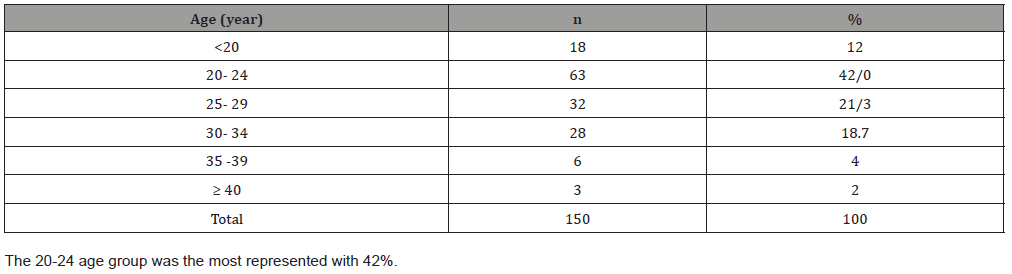
The average age was 25.31 ± 5.51 years with extremes of 17 and 45 years.
Marital status: Married women were the most represented with 93.3% of the cases (n=140), among the remaining we noted: 3 living with a partner (2%), 6 divorced (4%) and one single (0.7%).
Level of education: Patients with primary education were most represented with 36.7% (n=55), followed by those with no schooling (28.7%, n=43) and secondary education (20.7%, n=31).
Parity: Parity was dominated by paucipares 44.7% (n=67), followed by multiparous (34%, n=51) and primiparous (21.3%, n=32).
General knowledge of the contraceptive method
Patients had average knowledge about contraception in 77.3% followed by no knowledge (13.3%, n=20) (Table 2).
Knowledge of natural methods
Periodic abstinence was the best-known natural method with 61.3%, followed by exclusive breastfeeding (42%, n=63), complete abstinence (32.7%, n=40) and interrupted coitus (27.3%, n=26.6%) (Tables 3&4).
Table 2: knowledge of modern methods of contraception.
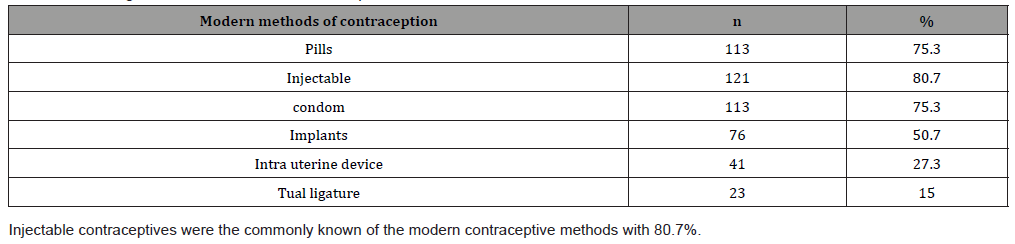
Table 3: Distribution of users according to the chosen method.
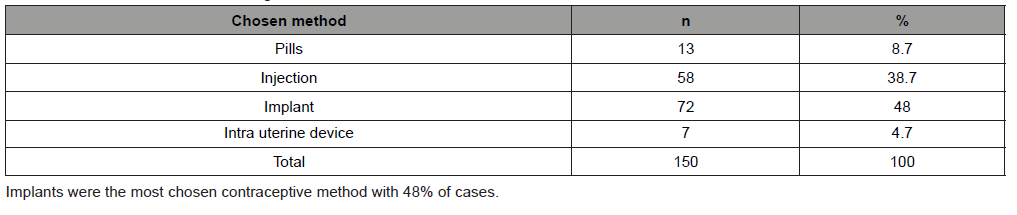
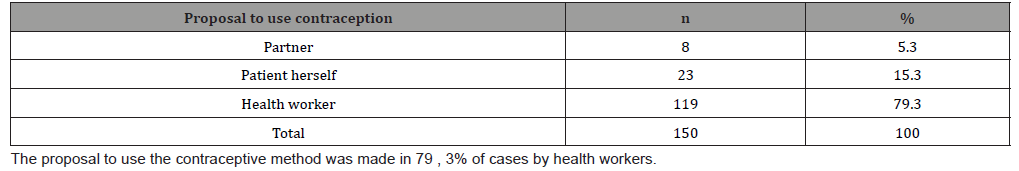
Table 4: Proposal to use the contraceptive method.
Advantages of the contraceptive method
The most well-known advantages of contraceptives by clients were birth spacing with 82.7%. This was followed by avoiding unwanted pregnancies (66%, n=99) and avoiding STI/HIV (38%, n=57).
Disadvantages of contraceptive methods
Infertility was the contraceptive method disadvantage most reported by clients with 54%.soot by weight gain (48.7%, n=73), and cycle disorder (48%, n=72).
Discussion
According to Lansac [5], the need for contraception is high among sexually active young people. This assertion is corroborated in this series with an average age of contraceptive users of 25.31± 5.51 years. The age group between 20 and 24 years old was the most represented with 42%. This result is close to that of Foumsou, et al [4] in N’Djamena in 2016 who reported an average age of 24.1 years and a high proportion of the 21-25 age group with 32.1%.
National data show a high rate of contraceptive use in urban areas compared to rural areas. We noted that 60% of clients resided in the city of N’Djamena against 40% outside N’Djamena (rural). This result is higher than that of Rahariniaina, et al. [6] in Ramainandro in Madagascar in 2015 who noted that 34% of clients lived in urban areas 34% versus 20% in rural areas.
Regarding marital status, married women represented 93% of the cases. The same observation was made by Foumsou, et al. [7] in N’Djamena Chad in 2015 who point out that 88.4% of patients were married. These results could be explained by cultural factors. Indeed, the occurrence of pregnancy outside marriage is not tolerated by many tribes in Chad. The occurrence of pregnancy outside of marriage is experienced as a disgraceful factor for families.
According to the literature [7,8], birth control becomes a requirement or an imperative if the number of children increases. This rhymes with a high proportion of multiparous women among clients requesting contraceptives. This series contrasts this observation with a higher proportion of paucipara. This could be explained by the haunting of iterative caesarean sections forcing patients to limit maternity.
According to recent data, information on contraceptive methods is provided through the usual means of communication [9]. Patients’ level of knowledge about different contraceptive methods may be related to their level of education and general culture. Thus, clients’ knowledge of contraceptive methods may be scattered. We noted that patients with average knowledge of contraceptive methods accounted for 77.3%. This rate is lower than that reported by Byamungu, et al. [10] in Bukavu in DRC in 2015 and Leye, et al. [8] reported a good knowledge of contraceptive methods of 79.3% and 81% respectively. The rate obtained in this series is thought to be linked to the high proportion no schooled and primary level patients (65.4%). In fact, schooling is a means of increasing knowledge globally and general culture more specifically.
Injectable contraceptives were most commonly known by clients with 80.7% Foumsou, et al. [4] in a previous study found a similar rate with 81% of clients knowing about injectable contraceptives. The same is true for Rahariniaina, et al. [6] who found a rate of 77.8% of clients knowing about injectable contraceptives. The availability of the product in many health care settings, especially the easier mode of use and the long duration of action may explain these results.
In the absence of hormonal contraception, the natural method can be used to prevent pregnancy. There are many such methods and knowledge about them is often based on their effectiveness. We noted that 61.3% of clients knew about periodic abstinence. This result is higher than Foumsou, et al. [7] found that users knew about periodic abstinence as a contraceptive method in 59.4%.
In order to avoid pregnancy in clients with uterine scarring, a long-acting contraceptive method is needed. This will help to avoid the mistakes associated with forgetting to take the pill [4,7]. We reported that 48% of the clients had opted for the implant. This result is close to that of Gennai in Monpellier, France in 2012 [11] who reported an implant use rate of 51.9%.
In general, the antenatal and postnatal consultations are also devoted to educating patients to improve their condition by offering them contraception, which appears to be a safe method to avoid pregnancy [12], thus the staff can encourage a couple to use contraception. This remains true in this series, with 79.3% of clients reporting being counselled by health workers on the use of contraception. This result differs from that of Coulibaly, et al. [13] in Cote d’Ivoire in 2019, who point out that 48% had been counselled by their spouses. This result can be explained by the overall decision in the couple.
Birth spacing remains the most frequently cited advantage for the use of contraceptive methods in certain African series [6-8]. This series corroborates those of these authors with 82.7% who cited birth spacing as the advantage of using contraception.
One of the factors that can hinder the use of contraceptives is bleeding [5]. However, other embarrassing effects, such as non-permanent sterility, are often cited as reasons for limiting contraceptive use. More than half of the clients (54%) cited infertility as a disadvantage of contraceptive methods. This result is higher than Barry [14] in Bamako in 2015, who found that 27% of users considered infertility to be the disadvantage of contraceptive methods.
Conclusion
The prescription of contraceptive methods in patients who have undergone a caesarean section is part of the common practice at N’Djamena Mother and child Hospital. The demographic characteristics of the clients are young, married and mostly urban. The clients’ level of knowledge and their practice are diverse. Injectable contraception remains the commonly known hormonal contraception. Among the natural contraceptive methods, Interrupted coitus is the best known. The decision to use contraception is facilitated by the health staff. The implant is the most commonly used method of contraception. The desire to avoid pregnancy is the benefit most noted by patients. The most reported disadvantage is infertility.
Through this study we can say that there is still a need to raise awareness among pregnant women in order to further boost the practice of contraception in patients who have undergone a caesarean section.
Acknowledgement
None.
Conflict of Interest
Authors declare no conflict of interest.
References
- Gronier H, Robing, Dewaily D (2011) Contraception. Practitioner's view. 61: 849-857.
- Sépou A, Enza J, Nali NM (2000) Difficulties related to the expansion of Contraception in urban and semi-urban areas of the Central African Republic. Med Afri Noire 47(2) :73-78
- (2015) National Institute of Statistics for Economic and Demographic Studies (INSEED). Chad Demographic and Health Survey III(EDST3).
- Foumsou L, Gabkika BM (2018) Post partum hormonal contraception at the Mother and Child Hospital of N'D Annales de l'Université de N'Djamena Série C 10: 97-108.
- Lansac J, Body G (2012) Gynaecology. Paris: Masson.
- Rahariniaina M (2015) Knowledge, attitudes, practices and modern contraceptive prevalence. Ramainandro: University of Tananarive.
- Foumsou L, Dangar GD, Djimasra TO (2015) Problem of Family Planning in the Hospitals of the city of N'Djamena. Med Afr Noire 62(4): 230-236.
- Leye MM, Niang K, Seck I, Camara PI, Faye A, et al. (2012) Knowledge, attitudes and practices of modern contraception in the health district of Bambeye, Senegal. Med Afr Noire 59(9): 430-436.
- Gabkika BM, Foumsou L, Adamou MA, Doune N, Tchoubou BM.
- (2016) Annales de l'Université de Bangui Série D 2(N°001): 27-30.
- Byamungu N, Kabinda J, Mvula M (2015) Knowledge and attitudes of adolescents in the Discrit Sanitaire of Bukavu (DRC) about contraception. Rev med Gd lacs 4(1): 40-46.
- Gennai J (2012) Contraception et précarité : enquête auprès de femmes consultant en centre de protection maternelle et infantile. Montpellier :'Université de Montpellier, France.
- Gabkika BM, Foumsou L, Saibana G, Abdelsalam S (2019) Contraception Method Following Spontaneous Abortion in N'djamena Mother and Child Hospital. South Asian Res J Nurs Health Care 1(2): 69-71.
- Coulibaly M (2019) Perceptions and practices of contraception in an urban co-community in the city of Abidjan. Abidjan: Université Félix Houphouet Boigny.
- Barry Sidibé (2015) Studies on the knowledge, attitudes and practices of resident students at the FAST Campus in Bamako in the area of family planning. University of Bamako.
-
Gabkika Bray Madoué, Foumsou Lhagadang, Saleh Abdelsalam. Knowledge, Attitudes and Practices About Contraception in Patients who had Undergone A Caesarian Section in N’Djamena Mother and Child University Hospital. W J Gynecol Women’s Health. 4(5): 2021. WJGWH.MS.ID.000598.
Contraception, Caesarean section, NMCUH, Pregnancy, Caesarean, Post-partum
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






