 Editorial
Editorial
Fetal Assessment in the 21st Century
Boris M Petrikovsky, Gynecologist, Maternal Fetal Medicine Specialist, Newyork, USA.
Received Date: August 31, 2018; Published Date: December 07, 2018
Editorial
Placental insufficiency remains the major reason for fetal hypoxia and accounts for 20-40% of perinatal mortality. There is no unanimity of opinion in the obstetrical community concerning the use of available tests of fetal well-being. These antepartum tests may be divided into three major groups:
a. Fetal heart rate assessment (NST, OCT).
b. Assessments of fetal biophysical activities other than fetal heart rate (fetal breathing movements, fetal gross body movements, fetal tone, and assessment of amniotic fluid volume).
c. Evaluation of maternal-fetal circulation (Doppler assessment of uterine, umbilical and major fetal vessels).
Non-stress testing (NST) remains the gold standard of antepartum fetal assessment. Its sensitivity lies in the prediction of fetal well-being, not fetal disease. Therefore, reactive NST usually reflects good fetal health, but positive result does not always signify fetal hypoxia.
Since its introduction, the fetal biophysical profile has played an important adjunctive role in antepartum fetal assessment. Utilization of different parameters which reflect various aspects of fetal activity (NST, fetal respiratory and gross body movements, fetal tone and amount of amniotic fluid) have allowed obstetricians to increase their diagnostic accuracy of antepartum fetal testing. Biophysical score of 8-10 corresponds to good fetal condition and requires no intervention. Testing should be repeated in one week if biophysical profile score is 4-6. If fetal lungs appear mature, delivery is indicated at this time. Otherwise the test should be repeated and if it still is non-reassuring, delivery should be undertaken. Biophysical score between 0 and 2 calls for immediate delivery.
We start fetal testing with NST. The criteria for reactivity include two or more FHR accelerations of at least 15 bpm, lasting at least 15 seconds during a 20-minute period.
If the NST is reactive, the only other parameter we assess is the amount of amniotic fluid. If the latter is adequate, the testing is over, and the patient is advised that fetal oxygen insufficiency is highly unlikely.
The NST has a 75% false-positive rate, because the majority of fetuses when sleeping exhibit “flat” FHR tracing without accelerations.
If the NST is non-reactive we proceed directly to assessment of the fetal biophysical profile (FBP). Alternative methods known as stress tests (oxytocin challenge test, nipple stimulation test), are less desirable because of the possibility of complications, most common of which is uterine overstimulation.
According to the gradual hypoxia concept, the biophysical activities that first become evident in the course of fetal development are the last to disappear in the case of hypoxia. Thus, if the NST is non-reactive, but the rest of fetal biophysical markers are present, the fetus is probably unaffected and required no further testing. The FBP score ranges from 0 to 10, with each of the five components if present and normal given a score of 2 and if absent or abnormal given a score of 0.
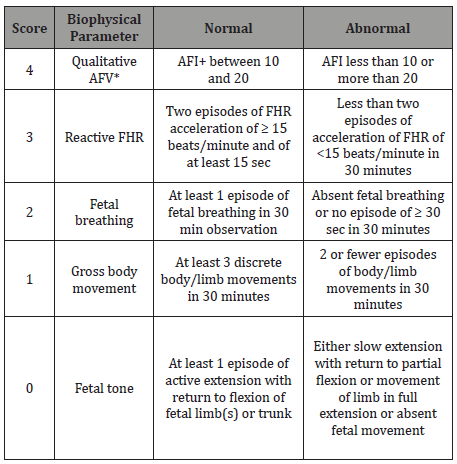
We have modified the current scoring system by introducing a “weighted fetal biophysical profile” in which each component of FBP is scored according to its importance in diagnosing fetal hypoxia. Amniotic fluid (AF), if adequate in volume, 4; NST, if reactive, 3; fetal breathing, 2; fetal movement, 1; and finally, fetal tone, 0. The idea of excluding fetal tone from FBP, total score can range from 0 to 10. A detailed description of “weighted” FBS is presented in Table 1. Our preliminary study of 500 high-risk patients has shown that the “weighted” biophysical score has a better correlation with neonatal outcome than the “traditional” score.
Table 1: Weighted biophysical profile scoring.
A retrospective analysis of biophysical scores in 860 high-risk pregnancies using ranking logistic regression analyses compared the “traditional” and “weighted” biophysical scoring system. A “weighted” score of 8 and above was associated with a favorable outcome in all cases; whereas a “traditional” score of 8 was assigned to several fetuses who were later found to be hypoxic. An unfavorable fetal outcome had a better correlation with the “weighted” score than with the “traditional” score.
As more collaborative data is collected, in both prospective or retrospective fashions, the validity of the “weighted” score will be further evaluated.
Major clinical errors in interpreting fetal biophysical profiles
Weekly assessment for most patients is sufficient provided initial FBP is normal. However, there are certain high-risk cases (insulin-dependent diabetes mellitus) that are in need of more frequent testing
a. Interval between testing when the previous test result is normal, equivocal, or abnormal.
b. Inexperience of the operator and faulty technique.
c. Reluctance to evaluate an abnormal test result.
d. Management based on the biophysical profile results without considering the overall clinical context of each case.
With the advances in neonatal care there is a tendency towards initiation of fetal testing earlier in the course of pregnancy. Antepartum testing can be started at 26 -28 weeks of pregnancy in most cases.
Antepartum fetal testing should be performed weekly in most pregnant patients and twice a week in extremely high-risk mothers and fetuses (severe IUGR, fetal tachyarrhythmias, severe alloimmunization, etc.).
Doppler assessment of fetal well-being is not a routine part of antepartum testing in the authors’ instructions. However, it is successfully used in selective conditions such as IUGR, twin to twin transfusion syndrome, and the presence of fetal cardiac abnormalities. Umbilical and fetal Doppler data are always used in conjunction with standard technique of fetal evaluation.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
-
Boris M Petrikovsky. Fetal Assessment in the 21st Century W J Gynecol Women’s Health. 1(4): 2018. WJGWH.MS.ID.000516.
Fetal, Assessment, Placental, Insufficiency, Hypoxia, Perinatal, Mortality, Obstetrical, Heart, Biophysical, Amniotic fluid, Circulation, Doppler, Umbilical, Fetal vessels, Oxytocin, Overstimulation, Biophysical, Antepartum, Twin transfusion.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






