Case Report
Case Report
Mulifocal Secondary Exstracranial Meningioma: Case Report
Selma Sönmez Ergün1*, Yusuf Erbayat1, Can Koç1, Meliha Gündağ Papaker2 and Pelin Yildiz3
1Professor, Department of Plastic Reconstruktive and Aesthetic Surgery, Bezmialem Medical School, Bezmialem Vakıf University, Istanbul-Turkey
2Department of Neurosurgery, Bezmialem Medical School, Bezmialem Vakıf University, Istanbul-Turkey
3Department of Pathology, Bezmialem Medical School, Bezmialem Vakıf University, Istanbul-Turkey
Selma Sönmez Ergün, Professor Surgery, Bezmialem Medical School, Bezmialem Vakıf ,University, Istanbul-Turkey.
Received Date: September 05, 2023; Published Date: September 13, 2023
Abstract
Meningiomas arise from arachnoid cells of the meninges and are classified as Grade I (benign), Grade II (atypical), and Grade III ( malignant) according to the WHO classification [1, 2]. Extracranial cutaneous meningiomas are rare tumors and can be divided into 2 types as primary and secondary. Primary extracranial meningiomas arise from ectopic arachnoid cells or the differential development and maturation of multipotent mesenchymal cells, whereas secondary meningiomas develop from an intracranial component associated with metastasis, seeding during surgery, or direct bone invasion of the intracranial meningiomas [1-3]. A female patient with multifocal secondary extracranial meningiomas located on the left temporoparietal and left mastoid area is presented here.
Introduction
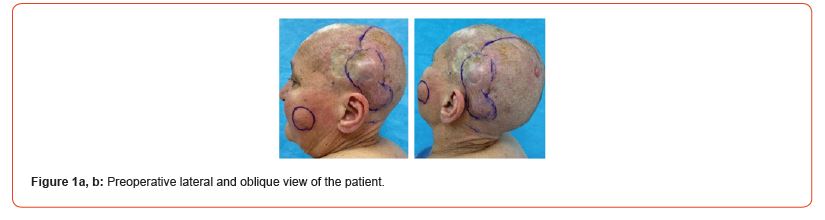
A 71-year-old female patient was admitted to our clinic with the complaints of two masses on her scalp that had been present for 3 years and a cystic lesion on the left buccal area. She reported that she had surgery in 2014 due to BCC that developed in the same region. Physical examination revealed a hard, immobile mass of 3x3 cm in size under the lateral part of the grafted area on the left temporoparietal region, and a hard, immobile mass of 3x2 cm in size on the left mastoid region, and a pinkish-gray skin lesion 1x1 cm in size on the upper part of the occipital region, and a partly mobile cystic lesion 4x3 in size.on the left buccal area (Figures 1a, b).
The initial neck examination was negative for lymphadenopathy A punch biopsy was performed from the mass that located under the grafted area of the scalp. The result was reported as benign skin appendage tumor (trichoepithelioma) due to basaloid cell proliferation which contains keratinous cysts. Since basal cell carcinoma recurrence was clinically suspected in the case, it was planned to remove the whole lesion.
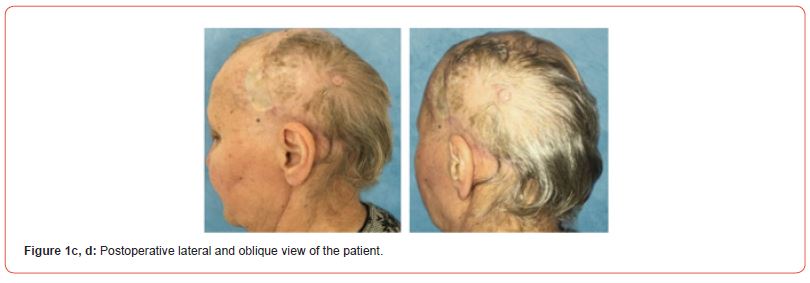
The masses on the scalp were excised as ‘en bloc’ with a margin of safety. Biopsies were taken from the cranial bone. The defect was covered with a transposition flap from the occipital region. The defect on the flap donor area was repaired with a split-thickness skin graft taken from the left thigh. The sebaceous cyst on the left cheek was extirpated. The patient was followed up with dressings, recovered uneventfully (Figures 1c, d).
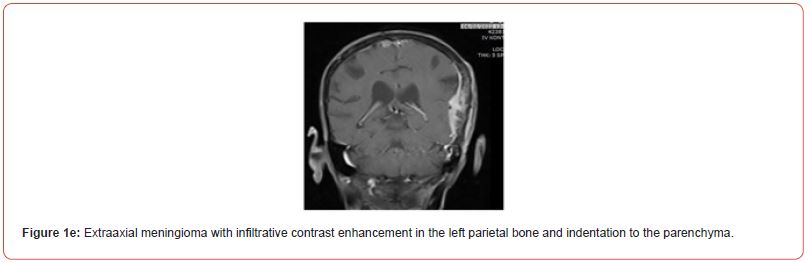
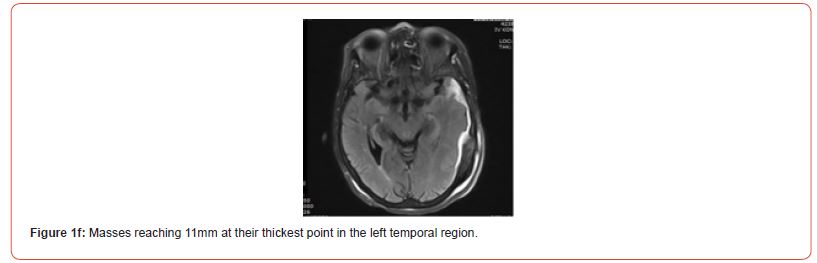
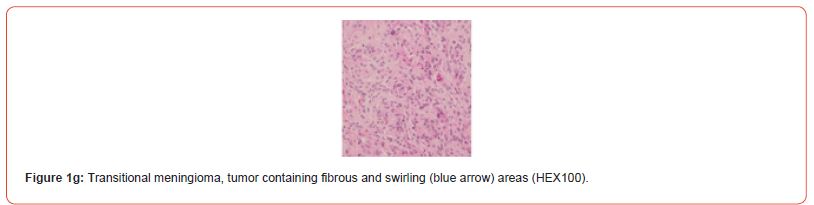
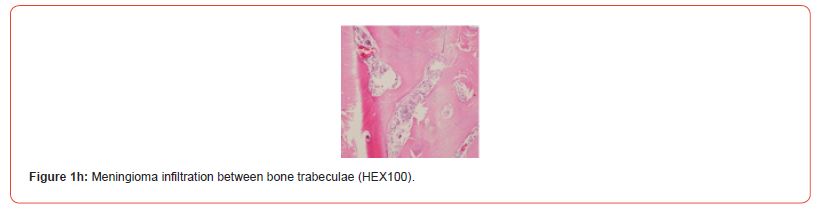
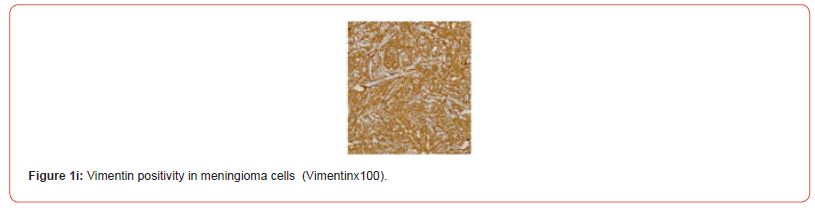
The histopathological result of the masses was reported as transitional type meningioma (Figure1g, h). Brain MRI revealed 3 meningiomas and erosion in the left parietal bone (Figure1e, f). The patient was evaluated as having secondary extracranial meningiomas, and was referred to the Neurosurgery Clinic for Gamma Knife treatment. There was no recurrence at 18-months follow-up.
Discussion
Meningiomas are common benign intracranial tumors in adults. They usually present as slow-growing intracranial lesions that tend to enlarge [4]. They are generally located intracranial, intraorbital and intravertebral, although they are rare, they can also be localized in other organs. They show a slight female predominance, and the prognosis of the disease is better than males [1-4]. The incidence of meningiomas ranges from 13% to 18% of all primary intracranial neoplasms, while the incidence of extracranial meningiomas ranges from 1% to 2% of all meningiomas [2]. Extracranial meningiomas are most commonly located in the orbit, outer plate of the calvarium, scalp, paranasal sinuses, nasal cavity, parapharyngeal region, and parotid [2].
Although secondary cutaneous meningiomas are associated with metastasis, seeding during surgical resection or extension of an intracranial meningioma; multiple reoperations due to tumor recurrence, radiation therapy, wound complications, immunosuppression, ‘high grade’ tumors and cerebrospinal fluid fistula are risk factors for the development of secondary cutaneous meningiomas [5]. Among these risk factors, our patient possibly had immunosuppression. Secondary cutaneous meningiomas are mostly associated with Grade II or Grade III meningiomas, but in some case reports, it has been shown that Grade 1 meningioma may also develop cutaneous extension, as in our case [6].
In order to reduce the recurrence rate in the treatment of cutaneous meningioma, complete surgical resection of the cutaneous and intracranial component should be performed, a part of the healthy bone around the affected bone should be removed and cranial reconstruction should be performed [5]. In our case, the cutaneous component was completely resected, and Gamma Knife treatment was applied because the patient did not accept intracranial surgery. In conclusion; by presenting this case, we aimed to contribute to accumulation of clinical data, to raise awareness of this rare disease and to reduce the morbidity with early diagnosis and treatment.
Acknowledgements
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
-
Selma Sönmez Ergün*, Yusuf Erbayat, Can Koç, Meliha Gündağ Papaker and Pelin Yildiz. Mulifocal Secondary Exstracranial Meningioma: Case Report. World Journal of Dermatology & Cosmetics. 1(1): 2023. WJDC.MS.ID.000504.
-
Atopic dermatitis, Allergic conjunctivitis, Dermatology, Allergic rhinitis, Atopic skin, Cosmetics, Skin lesions, Atopy, Inflammatory symptoms
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.